21 Orbits
21.1 Imaging Techniques
The orbits are osseous cavities in the anterior skull that contain the globe of the eye (“eyeball”) and serve as the source of vision. Imaging of the orbits plays a critical role in the diagnosis and management of various acute, chronic, and congenital conditions of the eye, orbit, and brain. In such imaging, computed tomography (CT) is superior for osseous detail and is rapidly available, whereas magnetic resonance imaging (MRI) is superior for revealing anatomic features and soft tissue characterization.
Computed tomography is typically the mainstay of acute orbital imaging for trauma and infection. In imaging for trauma, no intravenous contrast material is needed; however, postcontrast imaging is helpful for identifying abscesses in the setting of infection. Because of the dose of radiation needed, it is not appropriate to perform imaging both before and after the administration of contrast material, and if contrast is needed, the osseous structures of the orbit and surrounding areas can still be evaluated without dedicated unenhanced imaging.
Magnetic resonance imaging is very helpful in the examination of inflammatory conditions and both neoplastic and non-neoplastic masses affecting the orbit, and it is also helpful in characterizing congenital abnormalities of the eyes. Imaging both without and with contrast is typically indicated in MRI of the orbits, and for many indications it is important to also perform a dedicated MRI of the brain.
21.2 Anatomy
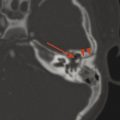
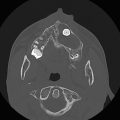
The globe of the eye has several substructures that can be identified through careful analysis of imaging. Along the anterior aspect of the globe is the lens, and anterior to this is the anterior chamber of the eye (Fig. 21.1 and Fig. 21.2). The movement of the globe is controlled by six extraocular muscles, five of which extend posteriorly to the orbital apex in a conelike configuration (Fig. 21.1 and Fig. 21.2), while the inferior rectus muscle attaches to the anterior floor of the orbit. The virtual cone created by the extraocular muscles is used to describe the location of structures in and around the orbit, with the optic nerve, superior ophthalmic vein, and intraconal retrobulbar fat in the intraconal space, and with the extraconal space predominantly containing fat as well as the lacrimal gland (Fig. 21.1 and Fig. 21.2).


21.3 Size and Position of the Globe
The size of the globe can be measured from the anterior aspect of the cornea to the position of the insertion of the optic nerve (Fig. 21.1a and Fig. 21.2), a measurement known as the axial length of the globe. The globe increases in size during infancy. In the setting of microcephaly, the appearance of the globes in relation to that of the head can suggest enlargement of the globes, and exact measurements can therefore help determine whether they are of appropriate size. The axial length of globe is approximately 18 mm in infancy, and reaches an adult size of approximately 24 mm over the first decade of life.
A measurement from the anterior aspect of the cornea to the lens provides the depth of the anterior chamber of the eye. This measurement can be inexact, especially because of slight obliquity of the lens, but typically ranges from 2 to 3.5 mm. A depth of the anterior chamber that exceeds 4 mm can be suggestive of glaucoma (Fig. 21.3). A shallow anterior chamber can be seen after a corneal laceration, and in some patients may be the only sign, on imaging, of an open globe (Fig. 21.4).


The midpole of the globe should be at, or slightly posterior to, a line connecting the medial and lateral points on the orbital rim (Fig. 21.5). Projection of the globe anterior to this line represents proptosis, which can be seen with a retrobulbar space-occupying lesion, including a tumor, hematoma, or muscle hypertrophy in thyroid eye disease.

The posterior contour of the globe should conform to that of a circle. Any outward deviation raises concern about a possible coloboma or morning glory disc anomaly (MGDA), which is discussed below (Fig. 21.6). Inward projection along the posterior globe is suggestive of papilledema, and warrants funduscopic examination and a workup for possible causes of increased intracranial pressures (Fig. 21.7).


21.4 Orbital Region Infections
Infections in the region of the orbit typically originate in two locations, either the facial soft tissues or the ethmoid sinuses. Ethmoid sinus disease has the potential for extending through the lamina papyracea and into the medial extraconal fat. This is often accompanied by dehiscence/demineralization of the lamina papyracea, but it can be unclear whether the extension of the disease to the orbit is due to such demineralization or occurred through venous channels and then secondarily resulted in dehiscence. In either case, the infection can threaten vision after it reaches the orbit, and an abscess in the orbit represents a surgical emergency. Because this constitutes an infection within the orbit, it is referred to as an orbital infection, in the form of either orbital cellulitis or an orbital abscess. The anterior orbit has a fibrous septum that extends from the globe to the margins of the orbit, and any infection posterior to this septum is referred to as a postseptal process. Because of this, orbital cellulitis and postseptal cellulitis are synonymous terms for the same condition.
A preseptal cellulitis is one that involves the face and periorbital region (and is therefore also known as periorbital cellulitis), without extension posterior to the septum (Fig. 21.8).

All infectious processes in the orbital region carry the risk of inducing a septic thrombophlebitis in the veins of the face and orbit (Fig. 21.9), and accordingly it is imperative to evaluate the caliber and patency of the superior ophthalmic vein and cavernous sinus in all studies of the orbit in which there is concern about infection. Following is a checklist for infectious processes affecting the orbit:

Preseptal or postseptal?
Cellulitis or abscess?
Any osseous demineralization?
Involvement of the ethmoid sinuses?
Patency of the superior ophthalmic vein and/or cavernous sinus?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree