25 Infection and Inflammatory Conditions
25.1 Spinal Infections and Inflammatory Conditions
The spinal cord is a part of the central nervous system (CNS), and as such is surrounded by cerebrospinal fluid (CSF), has a dural covering, and is myelinated by oligodendrocytes. Accordingly, many of the inflammatory conditions that influence the brain, of both infectious and noninfectious origin, can affect the spinal cord. The appearance of these entities on imaging overlaps that of neoplastic entities.
The spinal cord is supported and protected by a dural layer within the scaffolding of the vertebral column. Nerves of the peripheral nervous system leave this protective dural covering to provide motor, sensory, and autonomic innervation to the body. This creates several compartments within which infectious and inflammatory conditions can occur. Appropriate recognition and characterization of these conditions, as well as the differentiation of infectious and inflammatory processes from one another and from potentially neoplastic conditions, can help in the planning of treatment for all of these disease entities.
The involvement by an inflammatory process of the spinal cord (a myelitis) can result in neurologic deficits that can be localized to a specific sensory level, to the point at which a horizontally oriented (transverse) line can be drawn that demarcates symptomatic from asymptomatic levels. Clinically, the inflammatory process in which this can be done is known as a transverse myelitis, and can result from infection, acute disseminated encephalomyelitis (ADEM), neuromyelitis optica (NMO), multiple sclerosis (MS), lupus, vasculitis, trauma, spinal cord infarctions, tumors, and other conditions. Accordingly, transverse myelitis is a clinical finding and not a specific disease process, for which reason transverse myelitis cannot and should not be diagnosed based upon imaging. However, transverse myelitis is often an indication for magnetic resonance imaging (MRI) of the spine, in order to identify which of the entities named above may be present. Because a clinical instance of transverse myelitis can sometimes be idiopathic, there is a clinical entity known as idiopathic transverse myelitis, which in many cases is likely to be related to an immune-mediated process, such as ADEM.
25.2 Spinal Infections
25.2.1 Extradural Infections
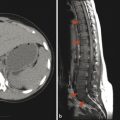
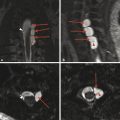
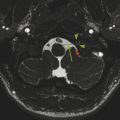
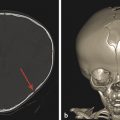
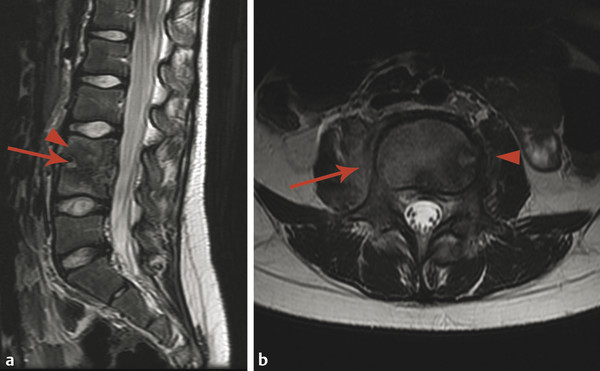
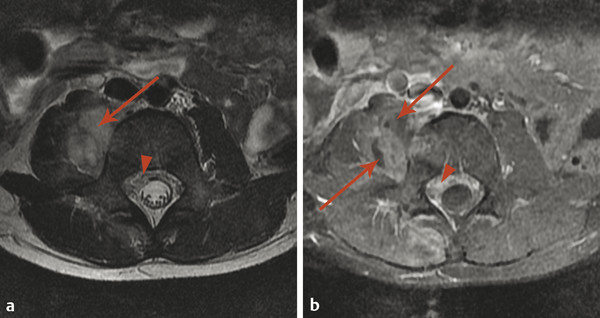
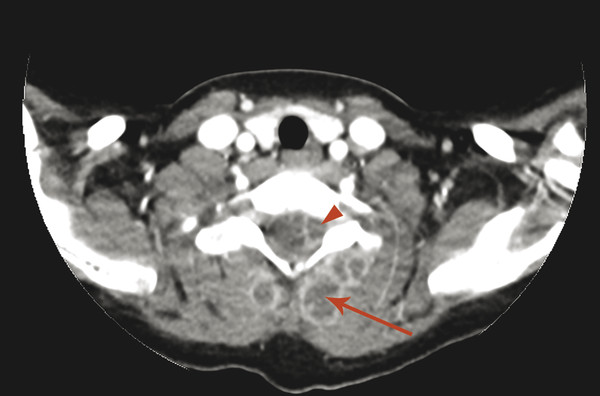
Extradural infections are those that involve the epidural space, the paraspinal space, and the intervertebral disk space, as well as the bone of the spine itself. Osteomyelitis of the spine often originates as diskitis. The intervertebral disk space is highly vascular in young children and may be susceptible to the hematogenous spread of infection. It is important to keep in mind that in young children a spinal infection such as diskitis/osteomyelitis may present as limping, hip pain, or a refusal to bear weight. The first signs of diskitis may be narrowing of the joint space on radiographs (Fig. 25.1). On MRI, there will be fluid within the disk space and heterogeneous enhancement in the disk and adjacent soft tissues. Diskitis may result in osteomyelitis of the adjacent vertebra, or the infection causing it may extend into the paraspinous soft tissues with the development of an abscess, such as in the psoas muscles (Fig. 25.2). This may be amenable to computed tomography (CT)–guided drain placement, particularly if the infection does not respond to intravenous (IV) antibiotics. An extradural infection that extends into the epidural space can result in an epidural abscess that may narrow the thecal sac and is typically a neurosurgical emergency (Fig. 25.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree