The “Dangerous” Anastomoses I: Ophthalmic Anastomoses
25.1 Introduction
The “dangerous” anastomoses are further subdivided into three separate cases (this case, Case 26, and Case 27), as we believe that a thorough understanding of potential anastomotic routes between the extracranial and the intracranial arteries is of utmost importance for all types of endovascular procedures in the external carotid artery (ECA) territory, including embolization of tumors of the skull base or the face, vascular malformations of the face and the orbit, dural arteriovenous malformations, and epistaxis.
The ECA is closely linked to the internal carotid artery (ICA) through embryology and phylogenetic development. This explains why although many anastomotic channels may not be visualized on routine (i.e., global) catheter angiographies, they are always present and will therefore necessarily open under certain predictable circumstances. As inadvertent embolization through these anastomoses can lead to major complications, such as stroke or cranial nerve palsies, both the circumstances under which the anastomoses may open and their potential localization have to be known by the interventional radiologist.
Anastomoses may open as a) a result of increased pressure on the feeding site of the anastomosis, b) because of increased demand on the receiving site of the anastomosis, or c) as a result of a “sump” effect of flow from the feeding to the receiving end of the anastomosis. Increased pressure in the feeding artery can build up during superselective injections, distal catheterizations, injections in wedged catheter position, or when using an embolizing agent that has the tendency to polymerize slowly and penetrate deep into the vascular bed. An increased demand is present when the proximal receiving artery is occluded or nearly occluded (e.g., a high-degree ICA stenosis may lead to recruitment of the ophthalmic collateral), and finally, high-flow shunts will sump the blood flow toward the shunt and, therefore, keep the anastomotic channels open.
Lasjaunias introduced the concept of functional vascular anatomy by subdividing the arterial anatomy of the head and neck by their territories (i.e., the internal maxillary, linguofacial, pharyngooccipital, thyroidal, cervical, internal carotid, and vertebral territories). He demonstrated that adjacent territories have close vascular and anastomotic interrelationships and will therefore function as potential vascular collaterals. Of these territories, there are three regions that serve as the major extracranial–intracranial anastomotic pathways: the orbital region, where the ophthalmic artery will act as the interface between the internal maxillary and internal carotid territories; the petrocavernous region, where the inferolateral and the meningohypophyseal trunk will be the major route to connect ECA and ICA vessels; and the upper cervical region, where the ascending pharyngeal, the occipital, and the ascending and deep cervical arteries will connect with the vertebral artery. In the following three cases, we discuss these three different regions separately.
25.2 Case Description
25.2.1 Clinical Presentation
A 72-year-old patient presented with idiopathic epistaxis refractory to nasal packing.
25.2.2 Radiologic Studies
See ▶ Fig. 25.1.
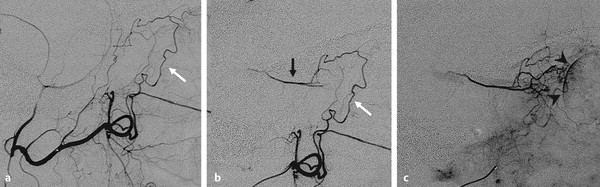
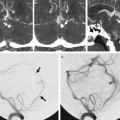
Fig. 25.1 On injection of the left common carotid artery, occlusion of the ICA was seen (not shown). Right ECA angiogram (a) and selective internal maxillary injection in arterial (b) and capillary (c) phase in lateral views demonstrate the anastomosis between the anterior deep temporal artery (white arrow) from the distal IMA to the ophthalmic artery (black arrow) through the lacrimal system. Note the choroidal blush (arrowheads) in the capillary phase that in patients with a patent ICA is not seen because of antegrade washout. No embolization was performed, and the patient was referred to surgery.
25.2.3 Diagnosis
Anastomosis between the anterior deep temporal artery from the distal internal maxillary artery (IMA) to the ophthalmic artery through the lacrimal system.
25.3 Embryology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree