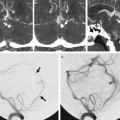
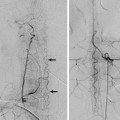
Fig. 30.1 Axial contrast-enhanced CT (a) shows a right hypervascular cervical mass splaying the carotid bifurcation. A preembolization common carotid artery angiogram (b) shows a hypervascular tumor between the ECA and ICA. The main supply is derived from the APhA (arrows), which in this case was the first ECA branch, as well as the occipital artery. A postprocedure angiogram (c) shows complete devascularization of the lesion.
30.1.3 Diagnosis
Carotid body paraganglioma.
30.2 Anatomy
The ascending pharyngeal artery (APhA) typically arises from the medial posterior wall of the proximal external carotid artery (ECA; ~80% of the cases). In the other 20% of cases, the origin may be from the occipital artery (as a branch or as a common trunk), from a common trunk with the lingual and facial arteries, from the carotid bifurcation, and even from the proximal cervical internal carotid artery (ICA), distal to the carotid bulb. In addition, the pharyngeal trunk and the neuromeningeal trunk may have separate origins. These variable patterns can be explained by the fact that the APhA has a separate origin from the ECA in the embryo, as part of the pharyngo-occipital system, rather than the ventral pharyngeal artery (ECA precursor). After its origin, the APhA courses superiorly, following the posterolateral wall of the pharynx, ventral to the ICA and dorsal to the ECA.
The APhA has two main branches, the pharyngeal trunk and the neuromeningeal trunk, and also gives rise to a third smaller but functionally important branch, the inferior tympanic artery.
The pharyngeal trunk supplies the mucosa of the posterior and lateral walls of the pharynx. It has three main branches: the superior, middle, and inferior pharyngeal arteries. There is a rich network of anastomotic vessels with the contralateral APhA and the distal branches of the internal maxillary artery. From an endovascular perspective, it plays a significant role in the treatment of posttonsillectomy hemorrhage (inferior pharyngeal artery) and in refractory epistaxis (middle pharyngeal artery). From the three pharyngeal arteries, the superior pharyngeal artery is the most important source of potentially dangerous anastomoses, as discussed later.
The neuromeningeal trunk has two main branches: the jugular and the hypoglossal branches. The jugular branch enters the skull base through the jugular foramen and runs posterolaterally. It supplies the vasa nervorum of the IX, X, and XI cranial nerves, as well as the posterior fossa dura mater and the walls of the sigmoid and petrosal sinus. The jugular branch plays a significant role in the supply of dural arteriovenous fistulas and is a reason why injections showing the APhA are mandatory in the diagnostic workup of this disease. The hypoglossal branch enters through the hypoglossal canal and supplies the XII cranial nerve and the meninges of the posterior cranial fossa. It also contributes to the odontoid arch through a descending branch. Both branches are involved in the supply of dural-based tumors such as meningiomas, and may be a target for superselective preoperative embolization. See also Cases 28 and 31.
The inferior tympanic artery commonly arises from the proximal neuromeningeal trunk but can arise from the pharyngeal trunk or as a separate branch between both main trunks. It enters the skull through the inferior tympanic canaliculus, together with the tympanic branch of cranial nerve IX (Jacobsen nerve), and gives supply to the vasa vasorum of the ICA. It may also contribute to the supply of cranial nerve VII through connections with the facial arcade. The main importance of the inferior tympanic artery is that it serves as a collateral route to reconstitute the petrous ICA in cases of segmental agenesis of the cervical ICA, better known as the “aberrant ICA” (see Case 3). It plays a significant role in the blood supply to glomus tympanicum and jugulotympanicum tumors.
30.3 Clinical Impact
The APhA is a route for multiple anastomoses with the ICA, branches of the ECA, and the vertebral arteries. ▶ Table 30.1 lists the “dangerous anastomoses” that may lead to focal neurological deficits and/or cranial nerve palsies during endovascular procedures in its territory.
APhA Branch | Anastomotic Branch | Connecting Artery | Parent Vessel |
Pharyngeal Trunk | |||
Superior Pharyngeal Artery | Eustachian Branch |