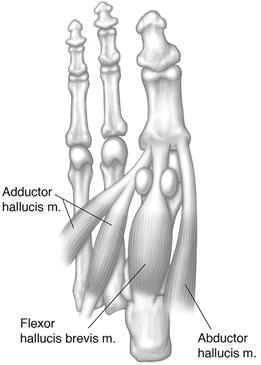
FIGURE 3-121 Illustrations of the sesamoid relationships in the axial (A) and plantar planes (B). C) Axial fat-suppressed fast SE image demonstrating the medial (M) and lateral (L) sesamoids seated in the metatarsal grooves.


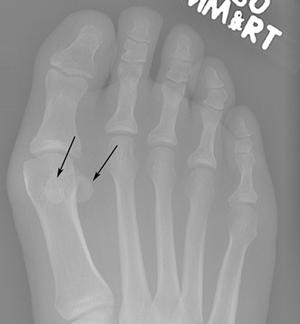
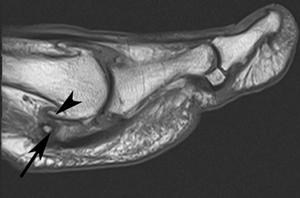
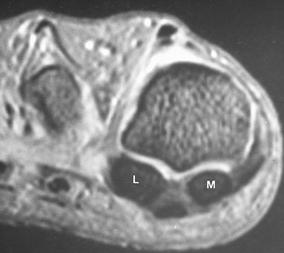
FIGURE 3-122 A) Radiograph demonstrating medial and lateral sesamoids (arrows) formed from single ossification centers. B) Radiograph demonstrating a bipartite medial sesamoid (arrows) with the lateral sesamoid formed from a single ossification center. C) Hallux valgus with rotation of the sesamoids laterally out of the normal metatarsal grooves. D) T1-weighted MR image demonstrating fragmentation of the sesamoid (arrow) and degenerative changes in the first metatarsophalangeal joint with osteophyte formation (arrowhead).
Disorders of the sesamoids account for 4% of all foot injuries [165,175]. Sesamoid disorders occur more commonly in patients with frequent use of high-heeled shoes, in dancers and athletes, especially runners [5,175]. There may also be associated arthropathies. Sesamoiditis is a generic term commonly used for painful disorders of the sesamoids [5,175]. The sesamoids may become inflamed, fracture, or undergo osteonecrosis. In addition to pain, physical examination may reproduce the symptoms by dorsiflexion of the great toe [186].
Routine radiographs including AP, oblique, lateral, and sesamoid views (Fig. 3-123) may be diagnostic [16,57]. The sesamoid may be fragmented, sclerotic, or fractured (Fig. 3-124). Soft tissue swelling over the involved sesamoid is usually present as well. In subtle cases, radionuclide bone scans are useful (Fig. 3-125). Increased tracer occurs in the presence of sesamoid disorders. A normal scan excludes the diagnosis.


FIGURE 3-123 A long-distance runner with chronic pain under the first metatarsal head. AP (A) radiograph shows an absent lateral sesamoid (arrow). Sesamoid view (B) shows only a small remnant (arrow) of the lateral sesamoid resulting from avascular necrosis and bone resorption.


FIGURE 3-124 Lateral (A) and sesamoid (B) views demonstrating sclerosis and fragmentation of the medial sesamoid (arrow) due to fracture with avascular necrosis.

FIGURE 3-125 Technetium-99m methylene diphosphonate bone scan shows increased tracer in the sesamoids and first metatarsophalangeal due to degenerative joint disease and early avascular necrosis of the sesamoids.
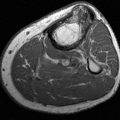
In some cases, ultrasound or MR imaging is required for evaluating unresponsive sesamoid pain [64,175,186]. MR images with a small field of view and digital coil can provide excellent detail for evaluation of marrow edema, tendon and capsular disorders, and synovitis (Fig. 3-126) [14,175].
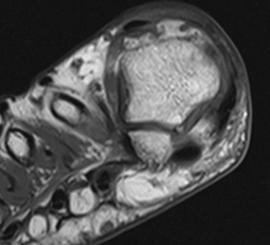
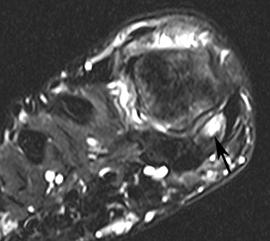
FIGURE 3-126 Marrow edema and fracture of the medial sesamoid. Axial T1- (A) and T2-(B) weighted images demonstrate marrow edema and a subtle fracture (arrow) in the medial sesamoid. There is also synovitis in the joint.
Treatment is usually conservative. Footwear changes, sesamoid pad, and anti-inflammatory medications may be sufficient. However, when conservative measure fail, resection of the sesamoids may be required (Fig. 3-127) [57].

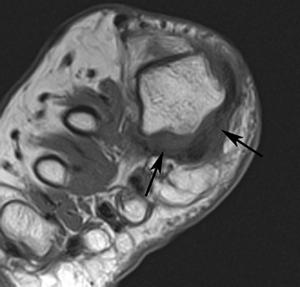
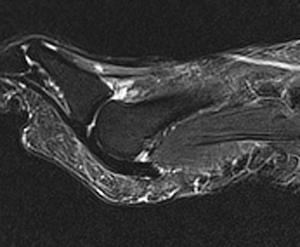
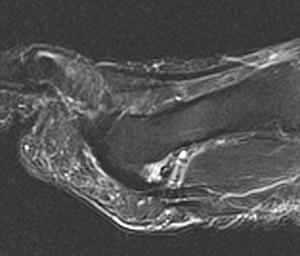
FIGURE 3-127 Sesamoidectomy. A) Standing AP radiograph demonstrates absence of both sesamoids on the right (arrows). B) Axial T1-weighted image demonstrate the absent sesamoid (arrows) with the flexor hallucis longus tendon in normal position. Sagittal T2-weighted images (C,D) with an intact plantar plate.
Bursitis
Bursitis may involve the intermetatarsal bursae (Fig. 3-128) or occur in the plantar (adventitious bursae) (Fig. 3-129) aspect of the foot [124,161]. Studler et al. [161] recently reviewed changes in the plantar aspect of the feet in volunteers and cadaver specimens. Abnormal signal intensity on MR images was noted in 84% of 70 adult volunteers with a mean age of 45 years. Signal intensity changes were evident beneath the metatarsal heads. These findings occurred most commonly beneath the first (70%) and fifth (61%) metatarsals. Signal abnormalities varied, but 91% demonstrated low-signal intensity on T2-weighted images that correlated with fibrous tissue on histologic specimens. Contrast-enhanced imaging is important to confirm fluid filled bursae compared to other pathology such as fibrosis or neuromas. There is peripheral enhancement with plantar or intermetatarsal bursae [5]. Intermetatarsal bursae that measure less than 3 mm are often physiologic [5].
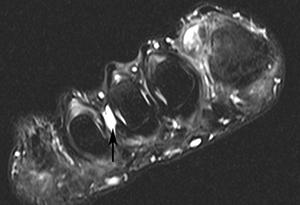
FIGURE 3-128 Intermetatarsal bursa. Coronal fast spin-echo T2-weighted image demonstrating an enlarged intermetatarsal (arrow) bursa between the third and fourth metatarsals.
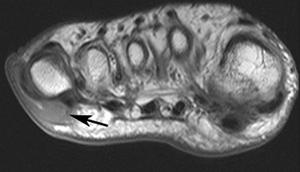
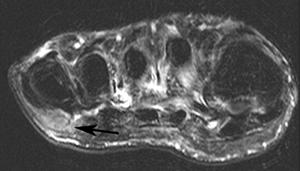
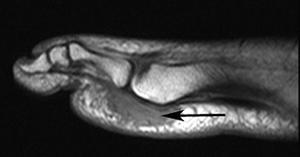
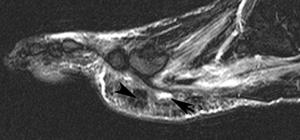
FIGURE 3-129 Abnormal signal intensity with bursa beneath the fifth metatarsal head. Axial T1- (A) and T2- (B) weighted images demonstrate an elliptical area of abnormal signal intensity beneath the fifth metatarsal head (arrow). Sagittal T1- (C) and T2- (D) weighted images show the abnormal soft tissue collection with a small adventitious bursa (arrow in D) and area of low-signal intensity on T2- weighted image D (arrowhead) due to fibrous tissue.
Plantar bursae may be managed conservatively with foot pads or change in footwear. On occasion, anesthetic and steroid injections are indicated when conservative measures are unsuccessful.
Freiberg Infraction
Freiberg infraction is a disorder that most commonly involves the second or third metatarsal heads [5,155]. The etiology is likely multifactorial. However, acute or repetitive trauma is commonly associated. The condition is most common in adolescent females and is also associated with use of high-heeled shoes [5,186]. The condition results in fragmentation, collapse, and fissuring of the metatarsal head.
Radiographs are usually diagnostic and useful for staging Freiberg infraction (Fig. 3-130) [155]. However, when indicated, MR imaging is useful to confirm the diagnosis and exclude other conditions such as synovitis [155]. In the latter, intravenous gadolinium may be useful to detect early synovial changes [14]. Synovitis, like osteonecrosis, also more commonly involves the second metatarsophalangeal joint [155].

FIGURE 3-130 Freiberg Infraction. AP radiograph demonstrating fragmentation of the second metatarsal epiphysis (arrow).
Management of patients with Freiberg infraction can be complex and is based on symptom duration, associated local and systemic disorders, and staging. Staging is based on image features [155].
- Stage I: fissuring of the epiphysis
- Stage II: central articular depression with soft tissue support intact
- Stage III: central depression with medial and lateral marginal projections
- Stage IV: fracture with central portion becoming a loose body and medial and lateral marginal projections
- Stage V: fattening and deformity of the metatarsal head with loss of joint space
Conservative treatment is recommended for Stages I and II as changes may resolve spontaneously (Fig. 3-131) [95,105,155]. Stages IV and V require surgical intervention. Multiple procedures have been used over the years. Approaches include debridement, wedge or shortening osteotomies, core decompression, resection arthroplasty, and joint replacement [95,105,155].



FIGURE 3-131 Conservative management of Freiberg infraction. A) Oblique radiograph demonstrating central depression of the head and a small lateral projection (arrow) (Stage III). AP (B) and oblique (C) images 6 years later demonstrate slight joint space narrowing with a small fragment (arrow in B) along the lateral joint line.
Hallux Rigidus
Hallux rigidus is a syndrome related to degenerative changes of the first metatarsophalangeal articulation resulting in cartilage loss, joint space narrowing and prominent osteophytes, particularly dorsally (Fig. 3-132). There is also restricted motion in the joint [45,86]. Hallux rigidus is second only in frequency to hallux valgus [45]. Coughlin and Shurnas [45] reported that this condition is bilateral in 80% of patients. Some reports demonstrate a male and others a female predominance.


FIGURE 3-132 Hallux rigidus. AP (A) and lateral (B) radiographs demonstrating advanced hallux rigidus with marked loss of joint space, no hallux valgus and prominent dorsal osteophytes with fragmentation (arrow) and soft tissue swelling.
Hallux rigidus usually results from chronic trauma. Athletes involved in track and football are commonly affected [86]. Most patients present with pain, commonly more marked over the dorsal aspect of the joint. Physical examination reveals restricted motion, prominence, and tenderness over the dorsal aspect of the first metatarsophalangeal joint. Pain is exaggerated with dorsiflexion of the first toe [45,74,94].
Joint space narrowing without hallux valgus deformity may be the only radiographic finding initially. In more advanced cases, there is marked loss of joint space, subchondral cysts, and marginal and prominent dorsal osteophytes on the dorsum of the first metatarsal head (Fig. 3-132) [74]. MR imaging features have also been described [157]. Loss of articular cartilage and marrow edema are more clearly demonstrated (Fig. 3-133). However, imaging beyond radiographs is usually not required to diagnose and manage hallux rigidus.
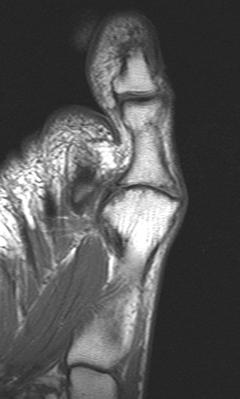
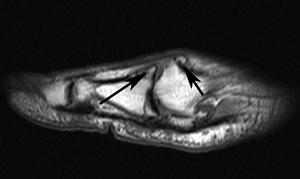
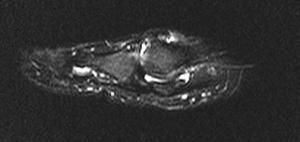
FIGURE 3-133 Hallux rigidus. T1-weighted axial and sagittal (A,B) and T2-weighted (C) sagittal images demonstrate joint space narrowing with prominent osteophytes on the dorsum of the first metatarsal head and proximal phalanx (arrows). There is also a joint effusion and subchondral marrow edema.
Treatment of early hallux rigidus may be successful using changes in footwear or joint injections. However, in more advanced cases, surgical intervention is more effective [157]. Treatment options will be more completely reviewed in Chapter 10.
Morton Neuroma
Morton neuromas are not true neoplasms, but are composed of fibrous tissue and neural degeneration resulting in a mass near the transverse metatarsal ligament (Fig. 3-134) [5]. These lesions occur based on chronic compression of the digital nerves against the intermetatarsal ligament. Morton neuromas may also be the result of compression of the nerve by adventitial bursae [5,186]. The lesions tend to occur more frequently in females using high-heeled footwear [5]. The most common site is between the third and fourth metatarsal heads [5]. Patients present with pain under the metatarsal heads. The pain is often referred to the toes [5,11]. Morton neuromas may be incidental findings as up to 33% may not present with clinical symptoms [11].
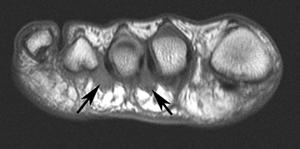
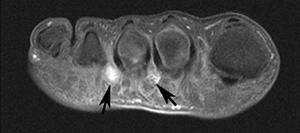
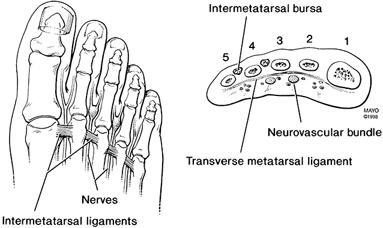
FIGURE 3-134 Morton neuroma. Axial T1- (A) and postcontrast fatsuppressed T1- (B) weighted images demonstrating neuromas between the second and third and third and fourth metatarsal bases. C) Illustration of the location of Morton’s neuromas and intermetatarsal bursae with relation to the transverse metatarsal ligament.
In patients with Morton neuroma, radiographs may show separation of the metatarsal heads. However, this finding is nonspecific and most radiographs are normal. Detection of Morton neuromas can be accomplished with ultrasound or MR imaging [2,14,155,182]. MR images demonstrate a focal soft tissue mass at the plantar between the metatarsal heads below the level of the transverse metatarsal ligament (Fig. 3-134). The lesion is usually equal or slightly greater than muscle density on T1-weighted images and mixed low and high-signal on T2-weighted sequences. Neuromas enhance following intravenous gadolinium. However, the enhancement pattern may not be uniform (Fig. 3-134B) [5,14,182]. Patients may be placed in the prone or supine positions to evaluate the forefoot on MRI. We usually use the supine position, though the prone position reduces motion artifact. Weishaupt et al. [181] reported superior results when the prone position was used to evaluate Morton neuromas.
Conservative treatment is usually used initially. This may include ultrasound-guided steroid injections which are much more successful than non-image-guided injections. When conservative treatment fails surgical intervention is indicated. Neuromas will also be discussed in Chapter 6.
REFERENCES
- Abraham E, Sternaman JE. Neglected rupture of the peroneal tendon causing recurrent sprains of the ankle. J Bone Joint Surg Am. 1979;61:1247–1248.
- Adler RS, Sofka CM. Percutaneous ultrasound-guided injections in the musculoskeletal system. Ultrasound Q. 2003;19:3–12.
- Ala-Ketola L, Peranen J, Kosivisto E, et al. Arthrography in the diagnosis of ligament injuries and classification of ankle injuries. Radiol. 1977;125:63–68.
- Anderson MW, Kaplan PA, Dussault RG, et al. Association of posterior tibial tendon abnormalities with abnormal signal in the sinus tarsi on MR imaging. Skeletal Radiol. 2000;29:514–519.
- Ashman CF, Klecker RJ, Yu JS. Forefoot pain involving the metatarsal region: differential diagnosis with MR imaging. RadioGraphics. 2001;21:1425–1440.
- Aström M, Gentz C-F, Nilsson P, et al. Imaging in chronic Achilles tendinopathy. A comparison of ultrasonography, magnetic resonance imaging and surgical findings in 27 histologically verified cases. Skeletal Radiol. 1996;25:615–620.
- Balen PF, Helms CA. Association of posterior tibial tendon injury with spring ligament injury, sinus tarsi abnormality and plantar fasciitis on MR imaging. Am J Roentgenol. 2001;176:1137–1143.
- Bassett FH, Gates HS, Billys JB, et al. Talar impingement by the anteroinferior tibiofibular ligament. J Bone Joint Surg Am. 1990;72:55–59.
- Bassett FH, Speer KP. Longitudinal rupture of the peroneal tendons. Am J Sports Med. 1993;21:354–357.
- Bencardino J, Rosenberg ZS, Beltran J, et al. MR imaging of dislocation of the posterior tibial tendon. Am J Roentgenol. 1997;169:1209–1112.
- Bencardino J, Rosenberg ZS, Beltran J, et al. Morton’s neuroma: is it always symptomatic? Am J Roentgenol. 2000; 175:649–653.
- Berkowitz JF, Kier R, Rudicel S. Plantar fasciitis: MR imaging. Radiol. 1991;179:665–667.
- Bernaerts A, Vanhoenacker FM, Van de Perre S, et al. Accessory navicular bone: not such a normal variant. JBR-BTR. 2004;87:250–252.
- Berquist TH. MRI of the Musculoskeletal System. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- Berquist TH. Diagnostic and therapeutic injections as an aid to musculoskeletal diagnosis. Semin Intervent Radiol. 1993;10(4):326–343.
- Berquist TH. Imaging of Orthopedic Trauma. 2nd ed. New York, NY: Raven Press; 1992.
- Bianchi S, Zwass A, Abdelwahab IF, et al. Evaluation of tibialis anterior tendon rupture by ultrasonography. J Clin Ultrasound. 1994;22:564–566.
- Black HM, Brand RL, Eichelberger MR. An improved technique for the evaluation of ligamentous injury in severe ankle sprains. Am J Sports Med. 1978;6(5):276–282.
- Blanchard KS, Finlay DBL, Scott DJA, et al. A radiological analysis of lateral ligament injuries of the ankle. Clin Radiol. 1986;37:247–251.
- Blei CL, Nirschl RP, Grant EG. Achilles tendon. US diagnosis of pathologic conditions. Radiol. 1986;159:765–767.
- Boles MA, Lomasney LM, Demos TC, et al. Enlarged peroneal process with peroneus longus tendon entrapment. Skeletal Radiol. 1997;26:313–315.
- Bonutti PM, Bell GR. Compartment syndrome of the foot. J Bone Joint Surg Am. 1986;68:1449–1450.
- Bottger BA, Schweitzer ME, El-Noueam KI, et al. MR imaging of the normal and abnormal retrocalcaneal bursae. Am J Roentgenol. 1998;170:1239–1241.
- Boyim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19:294–298.
- Brand RL, Collins MDF. Operative management of ligamentous injuries of the ankle. Clin Sports Med. 1982;1(1):117–130.
- Brantigan JW, Pedegana LR, Lippert FG. Instability of the subtalar joint. Diagnosis with stress radiography in 3 cases. J Bone Joint Surg Am. 1977;59:321–324.
- Brestenseher MJ, Trattnig S, Kukla C, et al. MRI vs. lateral stress radiography in acute lateral ankle ligament injuries. J Comput Assist Tomogr. 1997;21(2):280–285.
- Brigido MK, Fessell DP, Jacobson JA, et al. Radiography and US of os perineum fractures and the associated peroneal tendon injuries: initial experience. Radiology. 2005; 237:235–241.
- Bureau NJ, Cardinal E, Hobden R, et al. Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology. 2000;215:497–503.
- Cahill DR. Anatomy and function of the contents of the human tarsal sinus and canal. Anat Rec. 1965;153:1–18.
- Cardone BW, Erickson SJ, Den Hartog BD, et al. MRI of injury to the lateral collateral ligamentous complex of the ankle. J Comput Assist Tomogr. 1993;17(1):102–107.
- Cass JR, Morrey BF. Ankle instability: current concepts diagnosis, and treatment. Mayo Clin Proc. 1984;59:165–170.
- Cerezal L, Abascal F, Canga A, et al. MR imaging of ankle impingement syndromes. Am J Roentgenol. 2003;181:551–559.
- Cerezal L, Abascal F, Garcia-Valtuille R, et al. Ankle MR arthrography: how, why and when. Radiol Clin North Am. 2005;43:693–707.
- Cetti R, Andersen I. Roentgenographic diagnosis of ruptured Achilles tendons. Clin Orthop. 1993;286:215–221.
- Chandnani VP, Harper MT, Ficke JR, et al. Chronic ankle instability: evaluation with MR arthrography MR imaging, and stress radiography. Radiology. 1994;192:189–194.
- Chen JP, Allen AM. MR diagnosis of traumatic tear of the spring ligament in a pole vaulter. Skeletal Radiol. 1997; 26:310–312.
- Cheung Y, Rosenberg ZS, Magee T, et al. Normal anatomy and pathologic conditions of ankle tendons: current imaging techniques. RadioGraphics. 1992;12:429–444.
- Cheung Y, Rosenberg ZS, Ramsinghani R, et al. Peroneus quartus muscle: MR imaging features. Radiology. 1997; 202:745–750.
- Cheung Y, Perrich KD, Gui J, et al. MRI of isolated distal fibular fractures with widened medial clear space on stressed radiographs: which ligaments are interrupted? Am J Roentgenol. 2009;192:108.
- Chien AF, Jacobson JA, Famadar DA, et al. Imaging appearances of lateral ligament reconstruction. RadioGraphics. 2004;24:999–1008.
- Chundru U, Liebskind A, Seidelmann F, et al. Plantar fasciitis and calcaneal spur formation are associated with abductor digiti minimi atrophy on MRI of the foot. Skeletal Radiol. 2008;37:505–510.
- Church CC. Radiographic diagnosis of acute peroneal tendon dislocation. Am J Roentgenol. 1977;129:1065–1068.
- Clark HD, Kitaoka HB, Berquist TH. Imaging of tendon injuries about the ankle. Orthopedics. 1997;20(7):639–643.
- Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology and radiologic assessment. Foot Ankle Int. 2003;24:731–743.
- Delfaut EM, Demondion X, Bieganski A, et al. Imaging of foot and ankle nerve entrapment syndromes: from well demonstrated to unfamiliar sites. RadioGraphics. 2003;23:613–623.
- DeLuca PA, Bauta JV. Pes cavovarus as a late consequence of peroneus longus tendon rupture. J Pediatr Orthop. 1985;5:582–583.
- DiGiovanni BF, Fraga CJ, Cohen BE, et al. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000;21:809–815.
- do Carmo CCM, de Almeida Melao LIF, de Lemos Weber MFV, et al. Anatomical features of the plantar aponeurosis: cadaveric study using ultrasonography and magnetic resonance imaging. Skeletal Radiol. 2008;37:929–935.
- Dokter G, Lundaw LA. The accessory soleus muscle: symptomatic soft tissue tumor or accidental finding. Neth J Surg. 1981;33(3):146–149.
- Edwards GS, DeLee JC. Ankle diastasis without fracture. Foot Ankle. 1984;4(6):305–312.
- Evans GA, Frenyo SD. The stress-tenogram in diagnosis of rupture of the lateral ligament of the ankle. J Bone Joint Surg Br. 1979;61:347–351.
- Farooki S, Yao H, Seeger LL. Anterolateral impingement of the ankle: effectiveness of MR imaging. Radiology. 1998;207:357–360.
- Farooki S, Sokoloff RM, Theodorou DJ, et al. Visualization of ankle tendons and ligaments with MR imaging: influence of passive positioning. Foot Ankle Int. 2002;23:554–559.
- Fernandes R, Aguiar R, Trudell D, et al. Tendons of the plantar aspect of the foot: MR imaging and anatomic correlation in cadavers. Skeletal Radiol. 2007;36:115–122.
- Fernandez-Canton G, Casado O, Capelastagui A, et al. Bone marrow edema syndrome of the foot: one year follow-up with MR imaging. Skeletal Radiol. 2003;32:273–278.
- Fleischli J, Cheleuitte E. Avascular necrosis of the hallucial sesamoids. J Foot Ankle Surg. 1995;34(4):358–365.
- Fowler A, Phillip JF. Abnormality of the calcaneus as a cause of painful heel. Br J Surg. 1945;32:494–498.
- Funk DA, Cass JA, Johnson KA. Acquired adult flat foot secondary to posterior tibial tendon pathology. J Bone Joint Surg Am. 1986;68:95–102.
- Gallo RA, Kolman BH, Daffner RH, et al. MRI of tibialis anterior tendon rupture. Skeletal Radiol. 2004;33:102–106.
- Garth WP. Flexor hallucis tendinitis in ballet dancers. J Bone Joint Surg Am. 1981;63:1489.
- Gazdag AR, Cracchiolo A. Rupture of the posterior tibial tendon: evaluation of injury of the spring ligament and clinical assessment of tendon transfer and ligament repair. J Bone Joint Surg Am. 1997;79:675–681.
- Giuffrida AY, Lin SS, Abidi N, et al. Pseudo os trigonum sign: missed posteromedial talar facet fracture. Foot Ankle Int. 2003;24:642–649.
- Gregg JM, Silberstein M, Schneider T, et al. Sonography of plantar plates in cadavers: correlation with MRI and histology. Am J Roentgenol. 2006;186:948–955.
- Grogan DP, Walling AK, Ogden JA. Anatomy of the os trigonum. J Pediatr Orthop. 1990;10:618–622.
- Hayeri MR, Trudell DJ, Resnick D. Anterior ankle impingement and talar bony overgrowths: osteophyte or enthesophyte? Paleopathologic and cadaver study with imaging correlation. Am J Roentgenol. 2009;193:Web exclusive.
- Heckman DS, Reddy S, Pedowitz D, et al. Operative treatment of peroneal tendon disorders. J Bone Joint Surg. 2008;90A:404–418.
- Hilgason JW, Chandnani VP, Yu JS. MR arthrography: a review of current technique and applications. Am J Roentgenol. 1997;168:1473–1480.
- Hillier JC, Peace K, Hulme A, et al. MRI features of foot and ankle injuries in ballet dancers. Br J Radiol. 2004;77:532–537.
- Ho VW, Peterfly C, Helms CA. Tarsal tunnel syndrome caused by strain of an anomalous muscle. An MRI-specific diagnosis. J Comput Assist Tomogr. 1993;17(5):822–823.
- Horsfield D, Murphy G. Stress views of the ankle joint in lateral ligament injury. Radiography. 1985;51:7–11.
- Inglis AE, Scott N, Sculo TP, et al. Rupture of the tendon Achilles: an objective assessment of surgical and non-surgical treatment. J Bone Joint Surg Am. 1976;58:990–993.
- Jarde O, Diebold P, Havet E, et al. Degenerative lesions of the plantar fascia: surgical treatment by fasciectomy and excision of heel spur. A report of 38 cases. Acta Orthop Belgica. 2003;69:267–274.
- Johnson KA. The Foot and Ankle. New York, NY: Raven Press; 1994.
- Karasick D, Schweitzer ME. Tear of the posterior tibial tendon causing asymmetric flatfoot. Radiologic findings. Am J Roentgenol. 1993;161:1237–1240.
- Karasick D, Schweitzer ME. The os trigonum syndrome: imaging features. Am J Roentgenol. 1996;166:125–129.
- Karjalainen PT, Soila K, Aronen HJ, et al. MR imaging of overuse injuries of the Achilles tendon. Am J Roentgenol. 2000;175:251–260.
- Karr SD. Subcalcaneal heel pain. Orthop Clin North Am. 1994;25(1):161–175.
- Kelikian AS. Operative Treatment of the Foot and Ankle. Stamford, CT: Appleton and Lange; 1999.
- Kerr R, Frey C. MR imaging in tarsal tunnel syndromes. J Comput Assist Tomogr. 1991;15:280–286.
- Khoury, NJ, El-Khoury GY, Saltzman CL, et al. MR imaging of posterior tibial tendon dysfunction. Am J Roentgenol. 1996;167:675–682.
- Khoury NJ, El-Khoury GY, Saltzman CL, et al. Rupture of the anterior tibial tendon: diagnosis with MR imaging. Am J Roentgenol. 1996;167:351–354.
- Khoury NJ, El-Khoury GY, Saltzman CL, et al. Peroneus longus and brevis tendon tears: MR imaging evaluation. Radiology. 1996;200:833–841.
- Kier R, Dietz MJ, McCarthy SM, et al. MR imaging of the normal ligaments and tendons of the ankle. J Comput Assist Tomogr. 1991;15:477–482.
- Kijowski R, De Smet A, Mukharjee R. Magnetic resonance imaging findings in patients with peroneal tendonopathy and peroneal tenosynovitis. Skeletal Radiol. 2007;36:105–114.
- Kim S, Huh Y-M, Song H-T, et al. Chronic tibiofibular syndesmosis injury of the ankle: evaluation with contrast-enhanced fat-suppressed 3D fast spoiled gradient-recalled acquisition in the steady state MR imaging. Radiology. 2007;242:225–235.
- Kjaerguard-Anderson P, Anderson K, Soballe K, et al. Sinus tarsi syndrome: presentation of 7 cases and review of the literature. J Foot Surg. 1989;28:3–6.
- Kjaerguard-Anderson P, Wethslund JD, Helmig P, et al. The stabilizing effect of the ligamentous structures in the sinus and canalus tarsi on movement in the hindfoot: an experimental study. Am J Sports Med. 1988;16:512–516.
- Klein MA. MR imaging of the ankle. Normal and abnormal findings in the medial collateral ligament. Am J Roentgenol. 1994;162:377–383.
- Klein MA. Reformatted three-dimensional fourier transform gradient-recalled echo MR imaging of the ankle: spectrum of normal and abnormal findings. Am J Roentgenol. 1993;161:831–836.
- Klein MA, Spreitzer AM. MR imaging of the tarsal sinus and canal. Normal anatomy, pathologic findings, and features of sinus tarsi syndrome. Radiology. 1993;186:233–240.
- Koulouris G, Connell D, Schneider T, et al. Posterior tibiotalar ligament injury resulting in posteromedial impingement. Foot Ankle Int. 2003;24:575–583.
- Larson E. Experimental instability of the ankle: a radiographic investigation. Clin Orthop. 1986;204:193–200.
- Lawson JP. Clinically significant radiologic anatomic variants of the skeleton. Am J Roentgenol. 1994;163:249–255.
- Lee SK, Chung MS, Baek GH, et al. Treatment of Freiberg disease with intra-articular wedge osteotomy and absorbable pin fixation. Foot Ankle Int. 2007;288:43–48.
- Lektrakul N, Chung CB, Lai Y-M, et al. Tarsal sinus: arthrographic, MR imaging, MR arthrographic and pathologic findings in cadavers and retrospective study data in patients with sinus tarsi syndrome. Radiology. 2001;219:802–810.
- Lillich JS, Baxter DE. Common forefoot problems in runners. Foot Ankle. 1986;7:145–151.
- Lohman M, Kivisaari A, Vehmas T, et al. MRI abnormalities of the foot and ankle in asymptomatic, physically active individuals. Skeletal Radiol. 2001;30:61–66.
- Luck MD, Gordon AG, Blebea JS, et al. High association between accessory soleus muscle and Achilles tendonopathy. Skeletal Radiol. 2008;37:1129–1133.
- Lurk SC, Erickson SJ, Timins ME. MR imaging of the ankle and foot: normal structures and anatomic variants that may simulate disease. Am J Roentgenol. 1993;161:607–612.
- Ly JQ, Bui-Mansfield LT. Anatomy of and abnormalities associated with Kager’s fat pad. Am J Roentgenol. 2004;182:147–154.
- Maeseneer MD, Marcelis S, Jager T, et al. Sonography of the normal ankle: a target approach using skeletal reference points. Am J Roentgenol. 2009;192:487–495.
- Majors NM. Role of MRI in prevention of metatarsal stress fractures in collegiate basketball players. Am J Roentgenol. 2006;186:255–258.
- Mann RA, Thompson FM. Rupture of the posterior tibial tendon causing flat foot. J Bone Joint Surg Am. 1985;67: 556–561.
- Maresca G, Andriani F, Falez F, et al. Arthroscopic treatment of bilateral Freiberg Infraction. Arthroscopy. 1996;12:103–108.
- Melao L, Canella C, Weber M, et al. Ligaments of the transverse tarsal complex: MRI-anatomic correlation in cadavers. Am J Roentgenol. 2009;193:662–671.
- Mellado J, Rosenberg ZS, Beltran J. Low incorporation of soleus tendon: a potential diagnostic pitfall of MR imaging. Skeletal Radiol. 1998;27:222–224.
- Mengiardi B, Pfirrmann CWA, Vienne P, et al. Medial collateral ligament complex of the ankle: MR appearance in asymptomatic subjects. Radiol. 2007;242:817–824.
- Meyer JM, Garcia J, Hoffmeier P, et al. Subtalar sprain: a roentgenographic study. Clin Orthop. 1988;226:169–173.
- Michelson J, Easley M, Wigley FM, et al. Posterior tibial tendon dysfunction in rheumatoid arthritis. Foot Ankle Int. 1995;16(3):156–161.
- Miller TT, Staron RB, Feldman F, et al. The symptomatic accessory navicular bone: assessment with MR imaging. Radiology. 1995;195:849–853.
- Morti R. Dislocation of the peroneal tendon. Am J Sports Med. 1977;5(1):19–22.
- Muhle C, Frank LR, Rand T, et al. Collateral ligaments of the ankle: high resolution MR imaging with a local gradient coil and anatomic correlation in cadavers. RadioGraphics. 1999;19:673–683.
- Murr S. Dislocation of the peroneal tendon with marginal fracture of the lateral malleolus. J Bone Joint Surg Br. 1961;43:563–565.
- Myerson MS, Cerrato RA. Current management of tarsometatarsal injuries in the athlete. J Bone Joint Surg. 2008;90A:2522–2533.
- Nazarian LN, Rawool NM, Martin CE, et al. Synovial fluid in the hindfoot and ankle: detection of amount and distribution with US. Radiology. 1995;197:275–278.
- Nazarian LN. Ultrasound of the ankle and foot. Semin Ultrasound CT MR. 2000;21:275–284.
- Nazarian JA, Cerezal L, Narvaez J. MRI of sports-related injuries to the foot and ankle: part 1. Curr Probl Diagn Radiol. 2003;July/August:139–155.
- Nazarian JA, Cerezal L, Narvaez J. MRI of sports-related injuries of the foot and ankle: part 2. Curr Probl Diagn Radiol. 2003;July/August:177–193.
- Newmark H, Olken SM, Mellon WS, et al. A new finding in radiographic diagnosis of Achilles tendon rupture. Skeletal Radiol. 1982;8:223–224.
- Oae K, Takao M, Naito K, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227:155–161.
- O’Brien T. The needle test for complete rupture of the Achilles tendon. J Bone Joint Surg Am. 1984;66:1099–1101.
- O’Donnell P, Saifuddin A. Cuboid edema due to peroneus longus tendinopathy: a report of four cases. Skeletal Radiol. 2005;34:381–388.
- Olivieri I, Scarano E, Ciancio G, et al. Involvement of an inconstant bursa under the second metatarsal bone in spondyloarthritis. Clin Rheumatol. 2004;23:93–94.
- Parellada AJ, Morrison WB, Reiter SB, et al. Unsuspected lower extremity deep venous thrombosis simulating musculoskeletal pathology. Skeletal Radiol. 2006;35:659–664.
- Pastore D, Dirim B, Wangwinyuvirat M, et al. Complex distal insertions of the tibialis posterior tendon: detailed anatomic and MR imaging investigation in cadavers. Skeletal Radiol. 2008;37:849–855.
- Percy EC, Conochie LB. Surgical treatment of ruptured tendo Achilles. J Bone Joint Surg Br. 1975;57:535.
- Perrich KD, Goodwin DW, Hecht PJ, et al. Ankle ligaments on MRI: appearance of normal and injured ligaments. Am J Roentgenol. 2009;193:687–695.
- Pfeiffer WH, Cracchiolo A. Clinical results after tarsal tunnel decompression. J Bone Joint Surg Am. 1994;76:1222–1230.
- Povacz P, Unger F, Miller K, et al. A randomized prospective study of operative and non-operative treatment of injuries of the fibular collateral ligaments of the ankle. J Bone Joint Surg Am. 1998;80:345–349.
- Raatikainen T, Puronen J. Arthrography for diagnosis of acute lateral ligament injuries of the ankle. Am J Sports Med. 1993;21(3):343–347.
- Rademaker J, Rosenberg ZS, Beltran J, et al. Alterations of the distal extension of the musculus peroneus brevis with foot movement. Am J Roentgenol. 1997;168:787–789.
- Raikin SM, Elias I, Nazarian LN. Intrasheath subluxation of the peroneal tendons. J Bone Joint Surg. 2008;90A:992–999.
- Robison P, White LM, Salonen DC, et al. Anterolateral impingement: MR arthrographic assessment of the anterolateral recess. Radiology. 2001;221:186–190.
- Robison P, White LM, Salonen DC, et al. Anteromedial impingement of the ankle: using MR arthrography to assess the anteromedial recess. Am J Roentgenol. 2002;178:601–604.
- Robison P, White LM. Soft-tissue and osseous impingement syndromes of the ankle: role of imaging in diagnosis and management. RadioGraphics. 2002;22:1457–1471.
- Romanus B, Landahl S, Stener B. Accessory soleus muscle: a clinical and radiographic presentation of 11 cases. J Bone Joint Surg Am. 1986;68:731–734.
- Rosenberg ZS, Beltran J, Cheung YY, et al. MR features of longitudinal tears of the peroneus brevis tendon. Am J Roentgenol. 1997;168:141–147.
- Rosenberg ZS, Feldman F, Singson RD, et al. Peroneal tendon injury associated with calcaneal fractures: CT findings. Am J Roentgenol. 1987;149:125–129.
- Rosenberg ZS, Beltran J, Bencardino JT. MR imaging of the foot and ankle. RadioGraphics. 2000;20:S153–S179.
- Rosenberg ZS, Bencardino JT, Astion D, et al. MRI features of chronic injuries of the superior peroneal retinaculum. Am J Roentgenol. 2003;181:1551–1557.
- Rubin DA, Tishkoff NW, Britton CA, et al. Anterolateral soft tissue impingement in the ankle. Diagnosis using MR imaging. Am J Roentgenol. 1997;169:829–835.
- Rule J, Yao L, Seeger LL. Spring ligament of the ankle: normal MR anatomy. Am J Roentgenol. 1993;161:1241–1244.
- Sammarco GJ, Conti SF. Tarsal tunnel syndrome caused by an anomalous muscle. J Bone Joint Surg Am. 1994;76:1308–1314.
- Saupe N, Mengiardi B, Pfirrmann CWA, et al. Anatomic variants associated with peroneal tendon disorders: MR imaging findings in volunteers with asymptomatic ankles. Radiology. 2007;242:509–517.
- Sauser DD, Nelson RC, Lavine MH, et al. Acute injuries of the lateral ligaments of the ankle: comparison of stress radiography and arthrography. Radiology. 1983;148:653–657.
- Schmid DT, Hodler J, Mengiardi B, et al. Fatty muscle atrophy: prevalence in the hindfoot muscles on MR images of asymptomatic volunteers and patients with foot pain. Radiology. 2009;253:160–166.
- Schneck CD, Mesgarzadeh M, Bonakdarpour A, et al. MR imaging of the most commonly injured ankle ligaments. I. Normal anatomy. Radiology. 1992;184:499–506.
- Scholten PE, Sierevelt IN, van Dijk CN. Hindfoot endoscopy for posterior ankle impingement. J Bone Joint Surg. 2008;90A:2665–2672.
- Schweitzer ME, Eid ME, Deely D, et al. Using MR imaging to differentiate peroneal splits from other peroneal disorders. Am J Roentgenol. 1997;168:129–133.
- Schweitzer ME, Karasick D. MR imaging of disorders of the posterior tibialis tendon. Am J Roentgenol. 2000;175:627–635.
- Schweitzer ME, Karasick D. MR imaging of disorders of the Achilles tendon. AJR Am J Roentgenol. 2000;175:613–625.
- Schweitzer ME, Mahashwari S, Shabshin N. Hallux valgus and hallux rigidus: MRI findings. Clin Imaging. 1999;23:379–402.
- Silas SI, Herzenberg JE, Myerson MS, et al. Compartment syndrome of the foot in children. J Bone Joint Surg Am. 1995;77:356–361.
- Smillie IS. Treatment of Freiberg’s Infraction. Pro R Soc Med. 1967;60:29–31.
- Smith RW, Reischl SF. Metatarsophalangeal joint synovitis in athletes. Clin Sports Med. 1988;7:75–88.
- Solan MC, Calder JD, Bendall SP. Manipulation and injection for hallux rigidus: is it worth it? J Bone Joint Surg. 2001;83B:706–708.
- Stanish WD. Lower leg, foot and ankle injuries in athletes. Clin Sports Med. 1995;14(3):651–668.
- Stein RE. Rupture of the posterior tibial tendon in closed ankle fractures. J Bone Joint Surg Am. 1985;67:493–494.
- Stephens MM. Haglund’s deformity and retrocalcaneal bursitis. Orthop Clin North Am. 1994;25(1):41–46.
- Studler U, Mengiardi B, Bode B, et al. Fibrosis and adventitious bursae in plantar fat pad of forefoot: MR imaging findings in asymptomatic volunteers and MR imaging-histologic comparison. Radiology. 2008;246:863–870.
- Taser F, Shafiq Q, Ebraheim NA. Three-dimensional volume rendering of tibiofibular joint space and quantitative analysis of change in volume due to tibiofibular syndesmosis diastases. Skeletal Radiol. 2006;35:935–941.
- Taser F, Shafiq Q, Ebraheim NA. Anatomy of lateral ankle ligaments and their relationship to bony landmarks. Surg Radiol Anat. 2006;28:391–397.
- Taylor DE, Englehardt DL, Bassett FH. Syndesmotic sprains of the ankle: the influence of heterotopic ossification. Am J Sports Med. 1992;20:146–150.
- Taylor JAM, Sartoris DJ, Huang G-S, et al. Painful conditions of the first metatarsal sesamoid bones. RadioGraphics. 1993;13:817–830.
- Tehranzadeh J, Stoll DA, Gabriele OM. Posterior migration of the os peroneum of the left foot indicating a tear of the peroneal tendon. Skeletal Radiol. 1984;12:44–47.
- Termansen NB, Hansen H, Damvolt V. Radiologic and muscular status following injury to the lateral ligaments of the ankle. Acta Orthop Scand. 1979;50:705–708.
- Theodorou DJ, Theodorour SJ, Kakitsubata Y, et al. Plantar fasciitis and fascial rupture: MR imaging findings in 26 patients supplemented with anatomic data in cadavers. RadioGraphics. 2000;20:S181–S197.
- Theodorou DJ, Theodorou AJ, Farooki S, et al. Disorders of the plantar aponeurosis: a spectrum of MR imaging findings. Am J Roentgenol. 2001;176:97–104.
- Thompson TC. A test for rupture of the tendo Achilles. Acta Orthop Scand. 1962;32:461–465.
- Ton ERT, Schweitzer ME, Karasick D. MR imaging of peroneal tendon disorders. Am J Roentgenol. 1997;168:135–140.
- Tuite MJ. MR imaging of the tendons of the foot and ankle. Semin Musculoskeletal Radiol. 2002;6:119–131.
- Umans HR, Elsinger E. The plantar plate of the lesser metatarsalphalangeal joints: potential for injury and role of MR imaging. MRI Clin North Am. 2001;9:659–669.
- Umans HR. Imaging of sports medicine injuries of the foot and toes. Clin Sports Med. 2006;25:763–780.
- Umans HR, Cerezal L. Anterior ankle impingement syndromes. Semin Musculoskeletal Radiol. 2008;12:146–153.
- Uys HD, Rijke AM. Clinical association of acute lateral ankle sprain with syndesmotic involvement: stress radiography and magnetic resonance imaging study. Am J Sports Med. 2002;30:816–822.
- Vogler HW, Stienstra JJ, Montgomery F, et al. Anterior ankle impingement arthropathy. Clin Podiatr Med Surg. 1994;11(3):425–447.
- Wakely CJ, Johnson DP, Watt I. The value of MR imaging in the diagnosis of os trigonum syndrome. Skeletal Radiol. 1996;25:133–136.
- Wang X-T, Rosenberg ZS, Mechlin MB, et al. Normal variants and diseases of the peroneal tendons and superior retinaculum: MR imaging features. RadioGraphics. 2005;25:587–602.
- Ward DW. Syndesmotic ankle sprain in a recreational hockey player. J Manipulative Physiol Ther. 1994;17(6):385–394.
- Weishaupt D, Treiber K, Kundert H-P, et al. Morton neuroma: MR imaging in prone, supine and upright weight-bearing body positions. Radiology. 2003;226:849–856.
- Wredmark T, Carlstedt CA, Bauer H, et al. Os trigonum syndrome: a clinical entity in ballet dancers. Foot Ankle. 1991;11:404–406.
- Yu JS, Resnick D. MR imaging of the accessory soleus muscle appearance in six patients and review of the literature. Skeletal Radiol. 1994;23:525–528.
- Yu JS, Witte D, Resnick D, et al. Ossification of the Achilles tendon. Imaging abnormalities in 12 patients. Skeletal Radiol. 1994;23:127–131.
- Yu JS. Pathologic and post-operative conditions of the plantar fascia: review of MR imaging appearances. Skeletal Radiol. 2000;29:491–501.
- Yu JS, Tanner J. Considerations in metatarsalgia and midfoot pain: an MR imaging perspective. Semin Musculoskel Radiol. 2002;6:91–104.
- Zanetti M, DeSimoni C, Wetz HH, et al. Magnetic resonance imaging of injuries to the ankle joint. Can it predict clinical outcome? Skeletal Radiol. 1997;26:82–88.
- Zanetti M. Founder’s lecture of the ISS 2006: borderlands of normal and early pathological findings in MRI of the foot and ankle. Skeletal Radiol. 2008;37:875–884.
- Zanetti M, Steiner CL, Seifert B, et al. Clinical outcome of edema-like bone marrow abnormalities in the foot. Radiology. 2002;222:184–188.
- Zhu F, Johnson JE, Hirose CB, et al. Chronic plantar fasciitis: acute changes in the heel after extracorporeal high-energy shock wave therapy-Observations at MR imaging. Radiology. 2005;234:206–210.
CHAPTER 4
Fractures/Dislocations
Thomas H. Berquist
- Introduction
- Ankle Fractures
- Talar Fractures and Dislocations
- Anatomy
- Talar Neck Fractures
- Talar Body, Head, and Process Fractures
- Talar Dome Fracture
- Talar and Subtalar Dislocations
- Anatomy
- Calcaneal Fractures
- Midfoot and Forefoot Injuries
- Stress Fractures
- References
INTRODUCTION
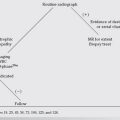
Foot and ankle fractures present a common problem for orthopaedic surgeons, emergency room physicians, family practice physicians, and radiologists. Appropriate use of imaging techniques is important in today’s cost-conscious environment. For example, 10% of emergency department visits are due to ankle sprains [3]. Do imaging procedures need to be ordered in all cases? Clinical algorithms have been developed in an attempt to reduce unnecessary imaging of foot and ankle injuries [2,4,5,13,15,16,29]. The Ottawa ankle rules were instituted to reduce costs of ankle radiographs. Ninety percent of ankle injuries are imaged with radiographs, but the fracture detection yield is less than 15% [2,15,29]. Application of the Ottawa ankle rules (pain over one or both malleoli and one or more of the following: (i) patient 55 years old or older; (ii) inability to bear weight; and (iii) bone tenderness at malleolar tip) before ordering radiographs may reduce costs in treating ankle injuries by 16% to 22% [15,29]. In addition, the American College of Radiology provides appropriateness criteria for which views and modalities should be used in patients with suspected foot and/or ankle injuries. Ankle images should include anteroposterior (AP), lateral, and mortise views; and AP, lateral, and oblique views should be obtained for foot injuries [1].
Radiographs or computed radiography (CR) images remain an effective screening tool for foot and ankle fractures. However, detection of subtle fractures, especially in children, complex fracture patterns, and evaluating the extent of soft tissue injury is more difficult. Additional imaging with CT or MR may be required in the acute setting or when the patients’ symptoms do not respond to treatment [3,9,14]. Haapamaki et al. [9] reported that the three most commonly overlooked fractures in the ankle were posterior and medial malleoli and juvenile Tillaux fractures. They also noted sensitivity for radiographs to be 87% for talar fractures, but only 25% to 33% for midfoot fractures. Lisfranc injuries were missed on radiographs in 24% of cases. These injuries were easily appreciated using CT [9]. Lohman et al. [14] reported improved detection of physeal fractures with MR imaging.
It is essential for those interpreting images to be aware of the manner in which various fractures and soft tissue injuries present, so that the images can be correctly and thoroughly evaluated and additional studies selected when appropriate [3,9,14]. Soft tissue changes may be the only clue to a subtle fracture or ligament rupture. Soft tissue swelling, obliteration of the fat planes or pre-Achilles fat triangle, and the presence of an effusion can be useful in identifying the location of subtle fractures or soft tissue injuries. These findings assist with selecting the next imaging modality to completely evaluate the injuries (Fig. 4-1, also see Fig. 2-3) [23,25,28].

FIGURE 4-1 Lateral radiograph of the ankle demonstrating a large joint effusion with anterior and posterior capsular distention (arrows).
It is also important to understand the clinical significance of certain fracture patterns. Fractures may be complete (involve both cortices) or incomplete (one cortex fractured). The latter are more common in children. Fractures may be comminuted (multiple fragments) or compound (open) [3,12,23].
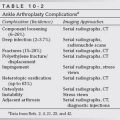
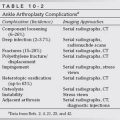
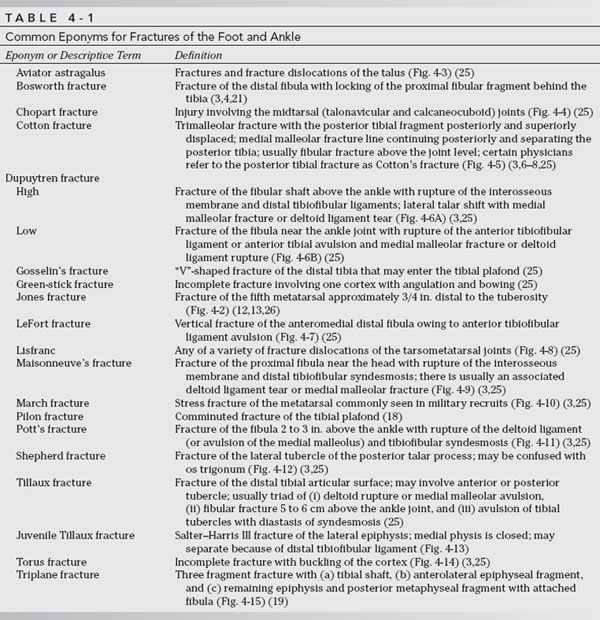
Terms other than complete or incomplete are also used in describing fractures. Avulsion fractures occur at the insertion of ligaments or tendons. Compression is a term usually reserved for vertebral fractures, but it can also be used to describe talar or calcaneal fractures [23]. Pathologic fractures involve bone with underlying abnormality such as osteoporosis or neoplasm. Stress fractures occur in normal bone that is exposed to unusual stress. The metatarsals in military recruits and the tibia and fibula in long-distance runners are commonly involved [3,25]. An insufficiency fracture is a category of stress fracture that occurs in abnormal bone under normal stress. This may occur in a patient with rheumatoid arthritis who becomes active too soon after joint arthroplasty [3,20]. Certain eponyms have been applied to many injuries about the foot and ankle [6–8,18,19,21,25,27]. These terms are frequently used and it is important to understand what they imply. However, eponyms can be confusing and inaccurately used (Figs. 4-2 to 4-15) [3,24,26]. For example, the Jone fracture (Table 4-1) was originally described as a fracture of the proximal fifth metatarsal. However, radiographs were so poor at that time that the fracture site was not clear. Today, the term Jones fracture (see Fig. 4-2) is commonly used to describe a fracture distal to the tuberosity, a condition that is more difficult to treat than a tuberosity fracture [3,10,11,24,26,25]. Today’s approach to proximal fifth metatarsal fractures will be discussed more completely in the Midfoot and Forefoot Injuries section of this chapter. The most commonly used eponyms are summarized in Table 4-1 (Figs. 4-2 to 4-15).
A systematic approach should be used when describing the imaging features of a fracture or fracture dislocation so the injury is completely assessed [3,25]. Eponyms can be confusing and should not be used without describing the associated fractures and soft tissue injury. The time, date, and views or imaging technique should be described first. This method makes it easier to keep examinations in chronologic order. This is followed by a general description of the fracture location, orientation (transverse, oblique, spiral), degree of displacement, angulation, and alignment (see Fig. 4-1). Angulation can be described using the direction of the distal fragment or the apex of the fragments [3,16]. I prefer the latter method of describing angulation (Fig. 4-16) [3]. Articular involvement, including the degree of separation or articular irregularity and the percentage of the articular surface involved, should be described. Soft tissue injury should also be carefully described (see Fig. 4-1) [3,22].


FIGURE 4-2 A) United Jones fracture (arrow). B) Typical proximal avulsion fracture (arrow) with intra-articular extension for comparison.

FIGURE 4-3 Mortise view of the ankle demonstrating a comminuted talar neck fracture (arrow).

FIGURE 4-4 AP view of the midfoot demonstrating a talonavicular fracture dislocation.

FIGURE 4-5 Cotton fracture. AP (A) and lateral (B) radiographs demonstrate a medial malleolar fracture (arrow) and displaced posterior tibial fracture (arrow, lateral view, B). Note the high fibular fracture (upper arrow) in A.


FIGURE 4-6 Dupuytren’s fracture. A) High fibular fracture with deltoid ligament rupture (black arrow). B) Low fibular fracture (arrow) with rupture of the tibiofibular ligaments (open arrow) and a medial malleolar fracture (arrow).
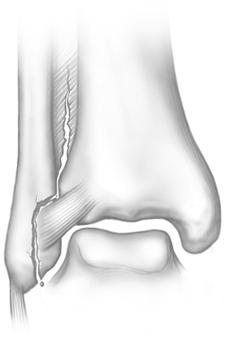
FIGURE 4-7 Illustration of LeFort’s fracture.

FIGURE 4-8 AP radiograph of the foot demonstrating widening of the space between the first and second metatarsal bases (vertical arrow) with displacement of the lesser metatarsals laterally (right horizontal arrow) and the medial cuneiform and first metatarsal medially (left horizontal arrow).


FIGURE 4-9 Maisonneuve fracture. A) AP ankle radiograph demonstrating a medial malleolar avulsion (arrow). B) Lateral view of the upper leg demonstrates an oblique fibular fracture (arrow).
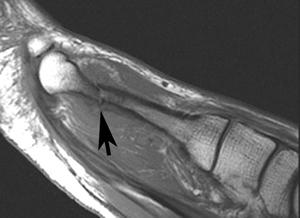
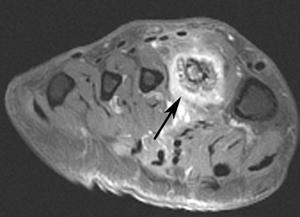
FIGURE 4-10 March fracture. Sagittal T1 (A) and axial contrast enhanced fat suppressed T1-weighted (B) images demonstrating a stress fracture (arrow) of the second metatarsal.

FIGURE 4-11 Pott’s fracture. Fracture of the fibula 2 to 3 in. above the joint with talar shift and medial malleolar avulsion.
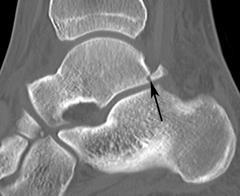
FIGURE 4-12 Sagittal CT image demonstrating a fracture of the posterolateral talar tubercle (arrow).

FIGURE 4-13 AP radiograph of the ankle demonstrating juvenile Tillaux fracture (arrows).

FIGURE 4-14 AP radiograph of the foot demonstrating a torus fracture at the first metatarsal base (arrow).


FIGURE 4-15 AP (A) and lateral (B) radiographs demonstrate a triplane fracture. The fracture looks like a Salter–Harris III fracture on the AP view and a Type II on the lateral view.
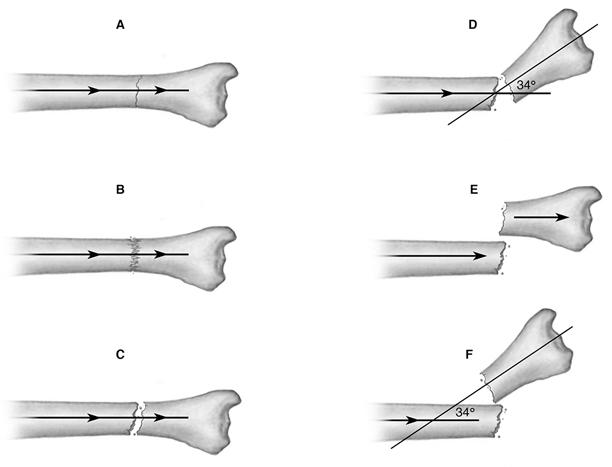
FIGURE 4-16 Illustration of fractures and descriptive terms. A) Undisplaced complete fracture with normal alignment. No angulation or shortening. B) Impacted fracture with trabecular compression. Minimal shortening with no angulation. C) Distracted fracture with separation of fragments but normal alignment and no angulation. D) Complete fracture with medial displacement of the distal fragment or 34° of lateral angulation. E) Complete fracture with dorsal displacement and no angulation. F) Complete fracture with no apposition. One sees shortening and 34° of lateral angulation.
After the interpretation of available images, one should suggest further techniques that may assist in more clearly defining the injury. Postreduction (closed or open) images should be clearly labeled chronologically because more than one film may be taken during manipulation (Fig. 4-17). Position of fragments should be carefully assessed using the same process applied to the original diagnostic studies. Joint space evaluation or failure to reduce a fracture with usual methods may indicate soft tissue interposition or osteochondral fragments, which prevent good position and alignment of fragments. Generally, these changes are evident to the physician reducing the fracture. If noted, after reduction, one should suggest the best technique to demonstrate the problem [22,23].


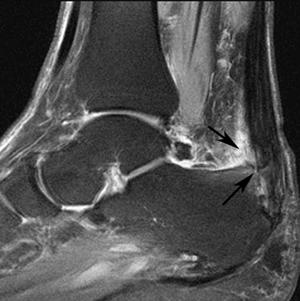





FIGURE 4-17 Radiographs from initial diagnosis through treatment and healing of a metatarsal fracture. Initial interpretation: AP (A) and lateral (B) views of the left foot demonstrate a comminuted oblique fracture of the distal fifth metatarsal diaphysis (arrow). There is dorsomedial displacement of the major distal fragment and slight shortening (note the line on metatarsal heads). Films taken with traction show improvement in length with the change in traction between image 1 (C) and 2 (D). Postreduction AP (E) and lateral (F) views show that reduction is maintained. There is a small medial fragment (arrow). Cast immobilization. AP (G) and lateral (H) views 5 months after injury show that the fracture has healed with slight angular deformity. Shortening of the fifth metatarsal (lines on metatarsal leads) persist.
Discussion of specific foot and ankle fractures and fracture dislocations is most easily accomplished by using anatomic regions. Therefore, ankle, hindfoot, midfoot, and forefoot injuries are discussed separately. Both adult and pediatric disorders are included.
ANKLE FRACTURES
Ankle fractures may be simple or complex with associated ligament ruptures [40,56]. The latter are more common in adults. Generally, fractures in patients older than 15 to 16 years of age are classified and treated using adult criteria. For discussion purposes, it is more effective to review adult and pediatric ankle injuries separately.
Pediatric Fractures
The appearance of ankle fractures in children depends on the age (growth plate development), relationship of the ligaments with the epiphysis, and the mechanism of injury [32,41,45,60,64]. Distal diaphyseal and metaphyseal fractures are frequently incomplete. In most cases, there is a posterior cortical break with buckling (torus fracture) of the anterior cortex above the growth plate (Figs. 4-18 and 4-19) [41]. Fractures of the distal tibia and fibula frequently involve the growth plates (Fig. 4-20). The distal tibia epiphysis is the second most common site for growth plate fracture [61]. In Roger’s series [68], 25% of 188 physeal injuries involved the distal tibia or fibula. Physeal fractures can result in growth or articular deformity if proper diagnosis and treatment are not implemented [52,73,77].