PART IV Head and Neck Vascular Lesions
A 27-year-year-old man presents with severe hemorrhage after extraction of a loose left lower molar tooth. He was previously healthy and was not on any medication. CT and MRI are performed, followed by angiography.
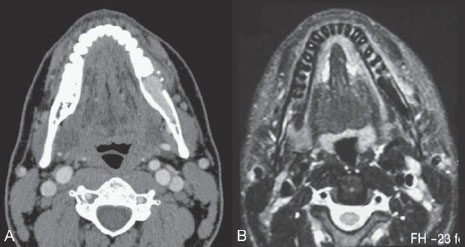
Fig. 31.1 (A) Post-contrast CT scan and (B) T2-weighted MRI.
CT/MRI
Post-contrast CT scan showed an osteolytic lesion at the left side of the mandible with evidence of cortical disruption. There was intense homogeneous enhancement of this lesion, which had an elongated appearance and extended along the mandible. A T2-weighted MR sequence demonstrated the left mandibular lesion as a flow-void structure, consistent with a vascular lesion (Fig. 31.1).
DSA
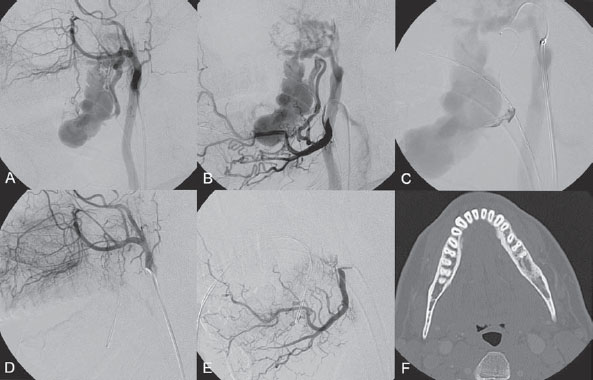
Angiography of the left internal maxillary artery (IMA) and left facial artery (FA) demonstrated a high-flow arteriovenous shunt within the mandible. There was supply from two converging arteries–the inferior alveolar artery from the IMA and the mental artery from the FA–with drainage into an ectatic venous compartment within the left mandible before further drainage into the external jugular vein (Fig. 31.2 A,B).
Mandibular arteriovenous fistulous malformation
Fig. 31.2 DSA. (A) Left IMA and (B) left FA angiograms in lateral views. (C) Hand injection through the microcatheter wedged within the left inferior alveolar artery in lateral view before glue injection. (D) Follow-up left IMA and (E) left FA angiograms at 2 months show complete closure of the fistula. (F) Axial CT scan of the mandible in bone window at 1 year after embolization reveals remodeling of the mandibular bone.
EQUIPMENT
- Standard 5F Access (puncture Needle, 5F vascular sheath)
- Standard 5F multipurpose catheter (Envoy; Cordis, Warren, NJ) with continuous flush and a 0.035-in hydrophilic guidewire (Terumo, Somerset, NJ)
- A 0.012-in flow-related microcatheter (Magic 1.2; Balt International, Montmorency, France) with a 0.008-in hydrophilic guidewire (Mirage; ev3, Plymouth, MN)
- A 10% glucose solution
- Histoacryl/Lipiodol (1 mL/2 mL)
- Contrast material
DESCRIPTION
Following diagnostic angiography, a 5F multipurpose catheter was advanced into the left IMA. A flow-directed microcatheter was introduced over a micro-guidewire into the inferior alveolar branch of the IMA in a wedged position as close to the fistula as possible. Control runs via hand injection through the microcatheter verified the position of the microcatheter. The microcatheter was then flushed with a glucose solution, after which glue at 50% concentration was injected to close the fistulous point under a blank roadmap; this resulted immediately in total obliteration of the fistula (Fig. 31.2C–E). The microcatheter was removed, and control angiography confirmed the complete closure. Follow-up angiography at 3 months revealed no recurrence of the fistula. A follow-up CT scan at 1 year after the procedure demonstrated remodeling of the mandibular bone (Fig. 31.2F).
Intraosseous mandibular arteriovenous malformations (AVMs) and fistulae are rare entities that must be recognized because they may present with life-threatening hemorrhage after tooth extraction or biopsy. These lesions are typically encountered in children and adolescents. Most patients have a history of recurrent minor episodes of bleeding while brushing their teeth. Other, unusual presenting symptoms include facial swelling, changes in skin and mucosal color, bruit, and dental loosening.
CT/MRI
- The high-flow characteristics of facial and scalp AVMs are seen as enhancing tubular structures on post-contrast CT scans or as flow voids on T2-weighted MR sequences.
- Bone resorption is a result of the high-flow nature of these lesions, which can be identified as well-defined osteolytic lesions on bone window CT images.
- MRI will show tubular flow voids within the bone.
CTA/MRA
- Dilated arterial feeders and early filling of the venous segment within the bone may be seen on CTA and MRA.
- Angiography is often done before embolization in an emergency setting.
- Although the major feeders are from the external carotid artery (i.e., branches of the IMA and FA), the intracranial circulation, especially the vertebral arteries in the case of mandibular AVMs, should also be injected to exclude associated intracranial AVMs in the setting of a cerebrofacial arteriovenous metameric syndrome (CAMS).
- A nidus-type lesion with multiple arterial feeders is more often encountered than a fistula-type lesion.
SURGICAL TREATMENT
- In the past, surgery was the treatment of choice for mandibular AVMs; currently, it is still performed when a cure cannot be obtained with endovascular treatment.
- Two techniques can be employed: transmandibular curettage and bone resection with transplantation.
- Surgical ligation of the external carotid artery is ineffective because of the recruitment of collateral feeders and is never indicated because it precludes further endovascular treatment.
- Embolization is the preferred treatment choice in an emergency setting to arrest the acute bleeding that occurs.
- Transarterial embolization with liquid material should aim at closing the fistulous point in fistulatype lesions and at filling the venous segment in nidus-type lesions.
- Transarterial embolization with particles alone will result in incomplete occlusion, recurrence, and rebleeding and is therefore not recommended.
- Proximal arterial occlusion will lead to the recruitment of other vessels to fill the AVM and is contraindicated because these smaller vessels will be more diffcult to catheterize.
- If transarterial embolization is unable to completely occlude the venous segment within the mandible, another endovascular approach can be proposed, such as transvenous embolization with coils or direct percutaneous/transosseous puncture into the venous segment to deliver the embolic material.
- If a surgical procedure is planned for definitive treatment of a facial/mandibular AVM, preoperative embolization may help to decrease surgical blood loss. In this instance, the major feeders are typically embolized with liquid material, followed by particle embolization of the remaining, smaller arterial feeders.
- Pulmonary emboli may develop.
- Stroke and cranial nerve palsies due to extracranial-intracranial anastomoses and embolization of arteries that supply the cranial nerves are extremely rare.
- Local infection and a reaction to the embolic material may occur. Occasionally, a foreign body granuloma may develop, and surgical removal of the embolic material may be required.
Published Literature on Treatment Options
Because mandibular AVMs are rare, only small case series and case reports are found in the literature. In contrast to our presented case, a fistulous lesion, most mandibular AVMs are of the nidus type; therefore, transarterial glue embolization may not result in complete cure if the glue fails to fill the venous segment sufficiently. Many authors prefer direct puncture through the bone to deliver the embolic material, usually glue, into the mandibular venous segment. There have been several case reports of transvenous approaches to the mandibular vein; however, many authors feel that although this is a good alternative treatment, it is often time-consuming and may require a large number of platinum coils, which may not be suitable if the patient is actively bleeding.
PEARLS AND PITFALLS__________________________________________________
- Mandibular AVMs can present with life-threatening bleeding following tooth extraction or biopsy and require emergent embolization.
- Occasionally, they may be a part of a cerebrofacial arteriovenous metameric syndrome (CAMS); therefore, vascular studies of the intracranial circulation are indicated.
- Sucient filling of the intraosseous venous segment is usually needed to cure these lesions, which may be achieved by a transarterial, transvenous, or direct puncture route.
Kiyosue H, Mori H, Hori Y, Okahara M, Kawano K, Mizuki H. Treatment of mandibular arteriovenous malformation by transvenous embolization: A case report. Head Neck 1999; 21 (6): 574–577
Persky MS, Yoo HJ, Berenstein A. Management of vascular malformations of the mandible and maxilla. Laryngoscope 2003; 113(11): 1885–1892
Rodesch G, Soupre V, Vazquez MP, Alvarez H, Lasjaunias P. Arteriovenous malformations of the dental arcades. The place of endovascular therapy: results in 12 cases are presented. J Craniomaxillofac Surg 1998;26(5):306–313
A 22-year-old woman presents with progressive enlargement of a soft pulsatile mass at the vertex that she has had since the age of 12 years. Physical examination reveals a compressible scalp mass at the midline parietal region. The mass is pulsatile, with a thrill on palpation. Outside CT reveals a vascular lesion, and the patient is referred to us for further angiographic evaluation.
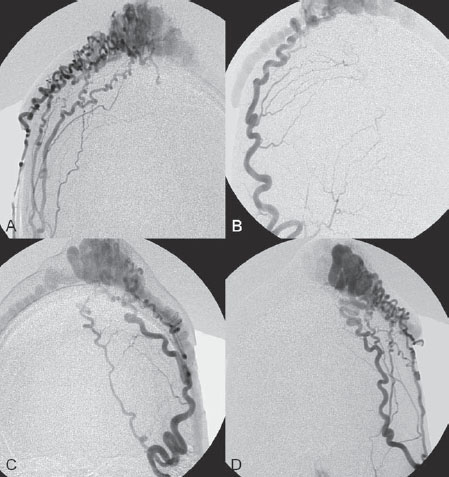
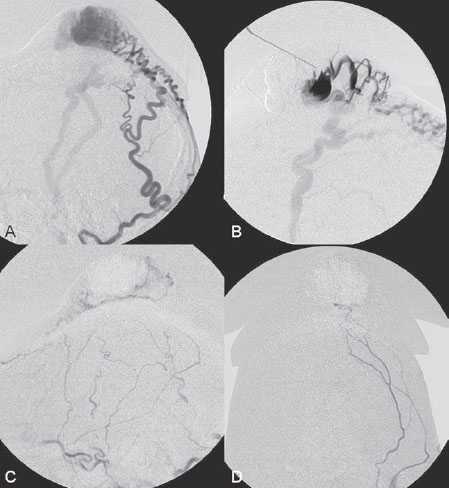
Fig. 32.1 DSA. (A) Right internal maxillary, (B) right occipital, (C) left internal maxillary, and (D) left occipital angiograms.
DSA
Angiograms of the internal maxillary arteries and the occipital arteries revealed a scalp arteriovenous malformation (AVM) at the high parietal region with multiple arterial feeders from subcutaneous branches of the superficial temporal and occipital arteries bilaterally. There was drainage into large ectatic venous pouches that corresponded to the pulsatile mass on physical examination before further drainage into scalp veins bilaterally (Fig. 32.1).
Scalp AVM
EQUIPMENT
- Standard 5F access (puncture needle, 5F vascular sheath)
- Standard 5F multipurpose catheter (Envoy; Cordis, Warren, NJ) with continuous flush and a 0.035-in hydrophilic guidewire (Terumo, Somerset, NJ)
- A 0.012-in flow-related microcatheter (Magic 1.2; Balt International, Montmorency, France) with a 0.008-in hydrophilic guidewire (Mirage; ev3, Plymouth, MN)
- A 21-gauge BD Angiocath (B Braun, Melsungen, Germany) with a connection tube
- A 10% glucose solution
- Histoacryl/Lipiodol (1 mL/3 mL, 1 mL/1 mL)
- Contrast material
DESCRIPTION
The procedure was done under general anesthesia. The skin of the scalp overlying the pulsatile mass was prepared before the procedure. Following diagnostic angiography, a 5F multipurpose catheter was advanced into the right occipital artery. A flow-related microcatheter was introduced over a micro-guidewire into the subcutaneous branch of the occipital artery. Attempts were made to place the microcatheter as close to the AVM as possible; however, this was technically difficult because of multiple kinks in the subcutaneous artery. A hand injection through the microcatheter verified its position. The microcatheter was then flushed with glucose solution, followed by the injection of glue at 25% concentration under a blank roadmap, which resulted in proximal occlusion of the occipital artery branch. The glue did not penetrate the venous pouch. The microcatheter was removed, and the procedure was repeated for the subcutaneous branches of the left superficial temporal and left occipital arteries, with similar results. Because proximal ligation would lead to subsequent reopening of the AVM, direct puncture of the venous pouch was done with a 21-gauge Angiocath, followed by hand injection of contrast to verify the position and venous outflow. The Angiocath was then flushed with glucose solution, and glue at 50% concentration was injected under a blank roadmap. Manual compression of the venous outflow was used to prevent glue migration. The direct puncture was repeated one more time and resulted in complete obliteration of the venous pouch and scalp AVM. The needle was removed, and a control angiogram of the external carotid arteries revealed complete closure of the scalp AVM (Fig. 32.2).
Fig. 32.2 DSA. Left occipital angiogram in (A) lateral view before the procedure and (B) hand injection via a 21-gauge needle into the venous pouch demonstrate the connection between the venous pouch and the scalp veins. Left external carotid artery angiogram in (C) lateral and (D) AP views after transarterial embolization and direct puncture reveals complete obliteration of the scalp AVM.
Scalp AVMs are abnormal AV communications localized within the subcutaneous fatty layer of the scalp. Although we use the term malformation lesions because of the multiplicity of arterial feeders, the AV connections are typically of the fistulous type, without an intervening capillary bed. These lesions have been referred to in the literature as cirsoid aneurysm, aneurysma serpentinum, aneurysma racemosum, and plexiform angioma. They are characterized by an AV shunt, the absence of an intervening capillary bed, and dilated, tortuous draining veins that often cause a cosmetic deformity and may occasionally bleed. The etiology of these lesions is still poorly understood; however, it is generally accepted that they can be either congenital or traumatic in origin. It is estimated that ~30% or more of these lesions are related to blunt, nonpenetrating trauma, with delayed occurrence of the shunt. Iatrogenic fistulae after hair transplantation have also been described in the literature. Most of the patients present with progressive scalp swelling. Rapid enlargement may occur during puberty, menstruation, and pregnancy. Large lesions may be associated with scalp necrosis and secondary malignant changes.
CT/MRI
- High-flow scalp AVMs are seen as enhancing tubular structures on post-contrast CT scan or as flow voids on T2-weighted MR sequences.
CTA/MRA
- Dilated arterial feeders and early filling of the ectatic venous pouches can be seen on CTA and MRA.
- Angiography is necessary for planning the treatment of scalp AVMs.
- The major arterial feeders are the subcutaneous arteries from the superficial temporal, occipital, and posterior auricular arteries. Occasional collaterals from the meningeal arteries may be seen, but this is unusual.
- The venous drainage pattern must be evaluated, in particular to detect intracranial connections and variations, such as a sinus pericranii.
SURGICAL TREATMENT
- Surgical resection is an excellent treatment choice for scalp AVMs and typically yields good cosmetic results. Presurgical embolization and the use of skin expanders in preparation for surgical resection of the AVM are required, especially for large lesions.
- In some cases, although the lesion has already been cured with endovascular treatment, surgical removal of the embolic material may be necessary.
- Ligation of the proximal arterial feeders is no longer performed because of the recruitment of collateral feeders, which complicates future treatment.
- Some large, high-flow AVMs involving the facial region are very difficult to manage, even with multimodality treatment, and may eventually result in a disastrous outcome.
ENDOVASCULAR TREATMENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree