Persistent Carotid-Vertebrobasilar Anastomoses
4.1 Case Description
4.1.1 Clinical Presentation
A 48-year-old man was evaluated for right-sided weakness with sudden onset 1 week before admission to our hospital.
4.1.2 Radiologic Studies
See ▶ Fig. 4.1; ▶ Fig. 4.2.
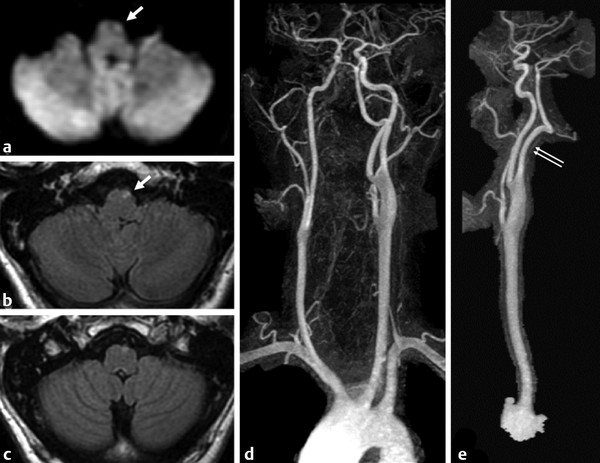
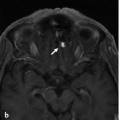
Fig. 4.1 Diffusion-weighted MRI (a) and fluid-attenuated inversion recovery (b,c) weighted images demonstrate a tiny focus of hypersignal in the left anterior medulla oblongata just cranial to the pyramids consistent with recent ischemic stroke. Contrast-enhanced MRA in anteroposterior (AP) (d) and lateral (e) views demonstrates hypoplasia of both VAs in the cervical portion. The basilar artery (BA) is fed by a congenital carotid–vertebrobasilar anastomosis that arises from the left ICA beyond the left common carotid bifurcation and connects to the intradural segment of the VA. This segmental anastomosis is the primitive HA.
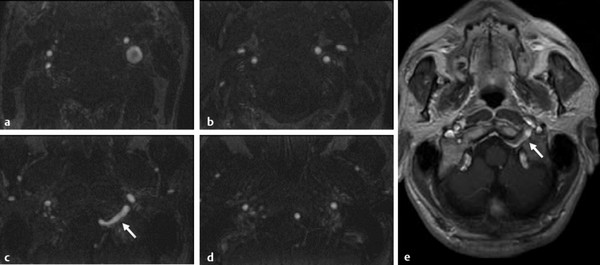
Fig. 4.2 Source images (a–d) and a contrast-enhanced T1-weighted MRI (e) reveal the course of the primitive HA through the hypoglossal canal to form the BA (white arrows).
4.1.3 Diagnosis
Left primitive hypoglossal artery (HA) supplying the posterior circulation with an acute anterior medullary ischemia.
4.2 Embryology and Anatomy
Carotid–vertebrobasilar anastomoses exist briefly in the earlier stages of embryonic development to supply the developing hindbrain. The understanding of the complex and sophisticated developmental anatomy of the craniocervical vasculature has its foundation in the seminal works by Congdon and Padget.
The primordial vascular system is organized into a series of three bilateral longitudinal systems: two ventral ones, the ventral and dorsal aortas that were discussed previously, and a dorsal one, located on the midline ventral to the neural tube, the longitudinal neural arteries. These longitudinal vessels are interconnected by transverse segmental arteries.
When the embryo is 4 mm long (28 ± 1 days; Padget stage I), the posterior circulation and the vertebrobasilar system as such do not exist yet. The caudal division of the ventral aorta courses over the midbrain, whereas the nourishment for the hindbrain comes through bilateral paired branches arising from the dorsal aortas that are usually transitory. At the cervical level, these branches are the first six segmental arteries.
The first and second of these arteries are called proatlantal arteries (PaAs) type 1 and type 2. At the intracranial level, two vessels bridge the dorsal aortas and the longitudinal neural arteries: the HA and, more cranially, the trigeminal artery (TA). Between the HA and the TA, Padget identified a third anastomosis, the otic artery (OtA), a finding that was not replicated in other works and is discussed in greater detail later.
These anastomoses persist for less than 1 week, and then they usually involute at the same time as the posterior circulation is developing. At 29 ± 1 days, the internal carotid artery (ICA) is better defined, and its caudal extremity anastomoses with the cranial longitudinal neural artery, giving origin to a primordial posterior communicating artery (PcomA). At the same time, the vertebrobasilar system begins to acquire its definitive architecture when the bilateral longitudinal neural arteries partially merge on the midline, constituting a primitive basilar artery (BA); at this point, the TA and HA start to disappear. Caudally, the definitive vertebral artery (VA) takes form through a series of longitudinal anastomoses linking the first six cervical intersegmental arteries. The ventral and dorsal portions of the segmental arteries regress, except for the PaA, which links to the BA by its cranial branch. At Padget stage III (31 ± 1 days, 10 mm), the collateral caudal branch of the sixth segmental artery connects with the cranial branch of the seventh segmental artery, which will become the adult subclavian artery, reversing the flow in a caudocranial direction. At this point, the BA blood supply no longer comes from the carotid system but, instead, via the VA, thus establishing the vertebrobasilar system. At this stage, the segmental embryonic vessels have disappeared, although some of them may persist in the adult.
Different studies have reported the general incidence of carotid-vertebrobasilar anastomoses between 0.1% and 1.25%. Probably for hemodynamic reasons, the persistence of these vessels is associated with aberrations in vascular embryogenesis, and thus they are often observed with other abnormalities of the vertebrobasilar circulation or of the circle of Willis.
The following section describes these vessels in the embryonic period and in their persistent form (adult configuration) from caudal to cranial.
4.2.1 Proatlantal Arteries
Proatlantal arteries (PaAs) are the last to disappear in the embryo and are related to the two most cranial intersegmental cervical segmental arteries. Persistence of a PaA has been reported in fewer than 50 cases.
PaA type 2 corresponds to the second intersegmental artery. It arises from the external carotid artery (ECA) and accompanies the second cervical nerve root. It courses posterior to the second cervical space to the vertebral canal. This artery usually regresses to the C2 occipitovertebral anastomosis. When the vessel does not involute, it originates from the ECA shortly after its origin, runs superoposteriorly as a vascular loop, and then ascends and pierces the dura at the C1 level, passing through the transverse foramen of the atlas. It then anastomoses with the contralateral VA V3 segment to form the BA ventral to the medulla.
PaA type 1 corresponds to the first intersegmental artery and is associated with the first cervical nerve. Because it maintains supply to the posterior circulations until the VAs are fully developed, this intersegmental artery is the last to disappear, typically at the 10–12-mm stage of the embryo, when it forms the intracranial part of the VA. If it regresses, the proximal remnant of this artery is, in the adult vasculature, the occipital artery, with its C1 occipitovertebral anastomosis. Persistence of this vessel is rarer than persistence of type 2 PaA. When still present in the postembryonic period, it originates from the posterior wall of the ICA between the C2–C4 level, runs dorsally to the first cervical space, passes in the occipitocervical space, and perforates the dura without ever running in the cervical canal. It joins the V3 segment of the VA in the suboccipital area before penetrating the foramen magnum. The persistent PaA is more often positioned laterally to the ICA in its course and makes a sharp curve dorsally and above the atlas, entering into the cranial cavity. Usually, there are no branches arising from the PaA, and only rarely does the occipital artery arise from the PaA. The ipsilateral, contralateral, or both VAs are hypoplastic or absent in around 50% of cases of persistent PaA (▶ Fig. 4.3; ▶ Fig. 4.4).
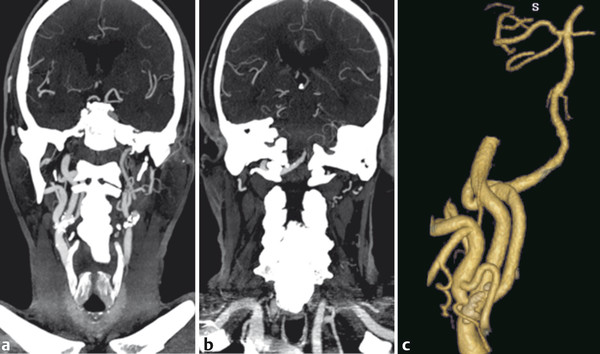
Fig. 4.3 CTA in coronal views (a,b) and 3D reconstruction in oblique view (c) demonstrate a right PaA type 1 supplying the posterior fossa.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree