The Spinal Cord Veins
43.1 Case Description
43.1.1 Clinical Presentation
A 6-year-old child was investigated for an objective thrill at the back of her neck and mild headaches. Because abnormal flow voids were described at the craniocervical junction, she was transferred to our institution, where a spinal MRI was performed, followed by a conventional angiography.
43.1.2 Radiologic Studies
See ▶ Fig. 43.1, ▶ Fig. 43.2, and ▶ Fig. 43.3.

Fig. 43.1 Sagittal T2-weighted (a,b) and contrast-enhanced T1-weighted (c) MRIs demonstrate abnormal vessels surrounding the craniocervical junction and in the perimedullary region. At the C5/6 level, there appears to be a conglomerate of abnormal vessels in the cord. There is no cord edema. Case continued in ▶ Fig. 43.2.
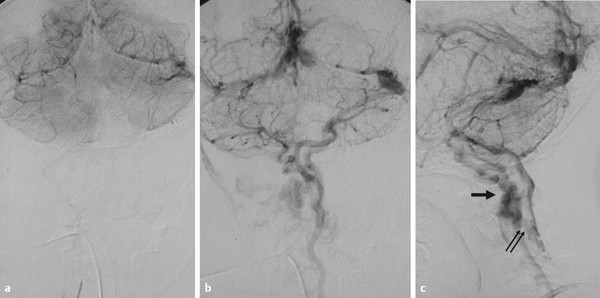
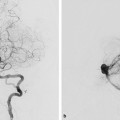
Fig. 43.2 Vertebral artery angiogram in capillary (a) and venous phase (b,c) in anteroposterior (AP) (a,b) and lateral (c) views fails to demonstrate an arteriovenous shunting lesion. Both transverse sinuses, the sigmoid sinuses, and the jugular bulbs and internal jugular veins are missing. The brain drainage is solely via the anterior perimedullary veins, and further downward, via a transmedullary anastomoses at C5/6 to the posterior medullary venous system of the cord. Further caudad, the drainage was via the normal radicular veins into the epidural venous plexus. Case continued in ▶ Fig. 43.3.
Fig. 43.3 The cause for this peculiar drainage pattern was thought to be a benign variant of brain drainage with congenital absence of the jugular foramen, as verified on computed tomography in the bone window (a–d). This case highlights the potential role for the cord to drain the brain, via the perimedullary veins, their intramedullary connections, and their outflow routes to the epidural vertebrovenous plexus.
43.1.3 Diagnosis
Congenital absence of the jugular foramen bilaterally with brain drainage via the perimedullary spinal veins.
43.2 Anatomy
The pattern of spinal venous drainage deviates substantially from that of the arteries, the most important difference being that the spinal arteries always follow the nerves, whereas the veins do not necessarily do so. Their arrangement is described according to the direction of venous drainage from the spinal cord parenchyma out to the epidural plexus.
The blood of the spinal cord parenchyma is drained by intrinsic veins in a radial pattern in an axial plane until the radial veins reach the surface of the spinal cord. They show a horizontal, radial, and symmetrical course in most parts of the spinal cord. Only in the lower thoracic cord, from the lower lumbar enlargement to the cone, are the sulcal veins (0.1–0.25 mm) larger than the numerous radial veins. At the level of the spinal pia mater, blood is accumulated in essentially two longitudinal collectors: the anterior and posterior median spinal vein. The anterior midline vein is located underneath the anterior spinal artery in the subpial space. It has its largest diameter lumbosacrally. In about 80% of cases, it courses together with the filum terminale as a sometimes very large terminal vein to the end of the dural sac. The venous longitudinal system on the anterior and posterior surface of the cord is more variable in course, size, and localization than the arterial system. The longitudinal midline veins are not always continuous and may be replaced by secondary systems of a smaller caliber.
The posterior median spinal vein takes a course independent from the posterolaterally located arteries and is especially large cranial to the thoracolumbar enlargement. Varicose convolutions are frequent. The posterior veins of the thoracolumbar enlargement are located in the perimedullary subarachnoid space. Having the largest diameter of all perimedullary vessels (including the arteries), at up to 1.5 mm, they are the vessels most likely to be seen on normal MRI scans. The vessels are part of a pial vascular network that has been called the venous or coronal plexus of the pia mater.
Intraparenchymal transmedullary venous anastomoses can be present. These midline anastomoses, 0.3–0.7 mm in diameter, connect the anterior and posterior median veins while receiving no tributaries from the intrinsic spinal cord veins (▶ Fig. 43.4). Because of their size, they may be seen on contrast-enhanced MRI.
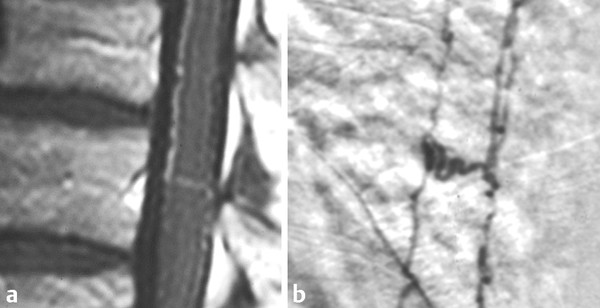
Fig. 43.4 MRI sagittal contrast-enhanced T1-weighted image (a) and corresponding spinal angiogram in venous phase on lateral view (b). Transmedullary venous anastomoses can connect the anterior and the posterior perimedullary venous systems. They sometimes can be visualized on contrast-enhanced MR and are normal variants of the cord drainage. These normal transmedullary veins explain why there are no developmental venous anomalies in the cord: transmedullary anastomoses between the different venous systems are the norm and are not a variation of drainage (which is the case for developmental venous anomalies in the brain where the transcerebral veins typically regress and the deep and superficial venous systems become separated).
Through these large anastomoses, blood can easily be directed from one side of the cord to the other. They are most often found in the thoracic region. At the cervical level, the anterior and posterior median veins connect to the brainstem veins and basal sinuses around the foramen magnum.
The superficial venous blood collectors drain into the epidural venous plexus through radicular veins. The transition of the midline vessel to the radicular vein forms a hairpin course similar to the arterial configuration (▶ Fig. 43.5).
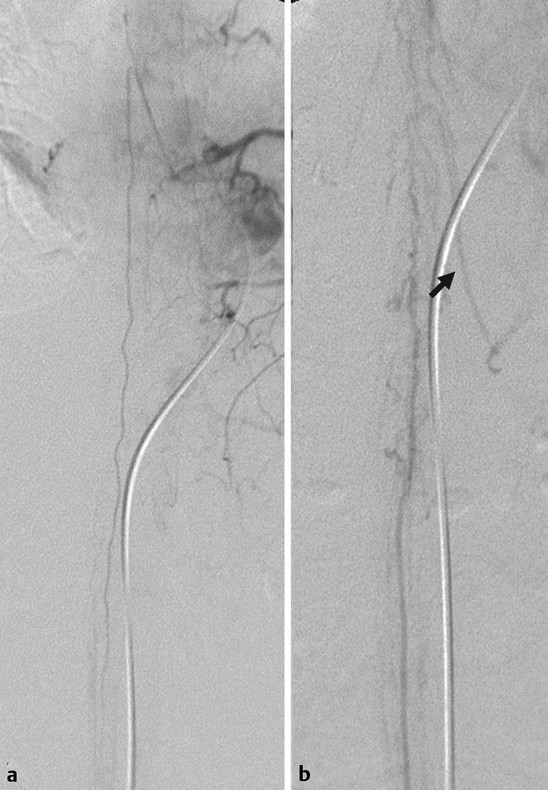
Fig. 43.5 Selective injection into the segmental artery from which the anterior spinal artery originates in arterial (a) and venous (b) phase demonstrates the classical hairpin curve of the anterior spinal artery in the arterial phase. However, it becomes apparent in the venous phase that the venous drainage via the radicular veins can have a similar hairpin course (arrow). As the veins are typically larger in diameter than the arteries, depiction of a “hairpin” vessel on static MR angiogram or CTA could therefore be related both to a slightly enlarged anterior spinal artery (because of increased flow) or a normal-sized venous vessel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree