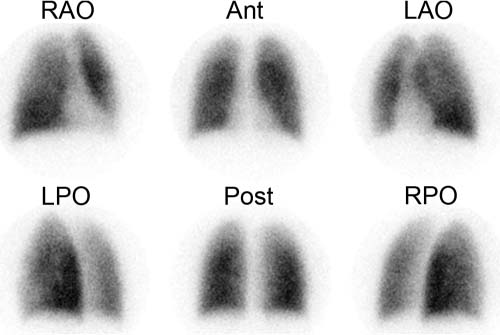
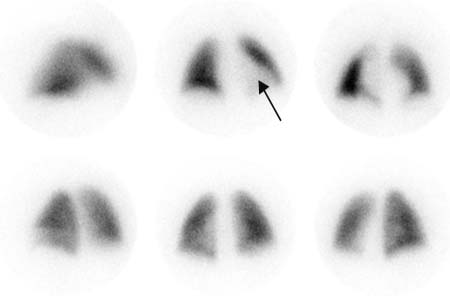
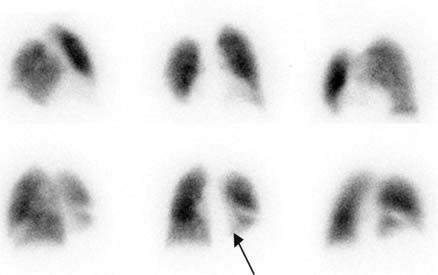
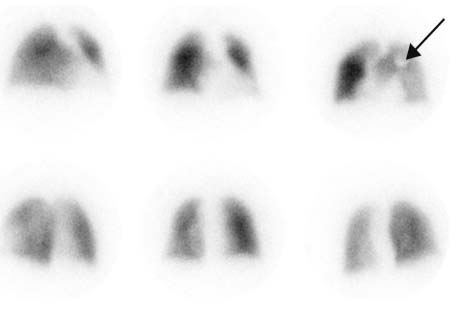
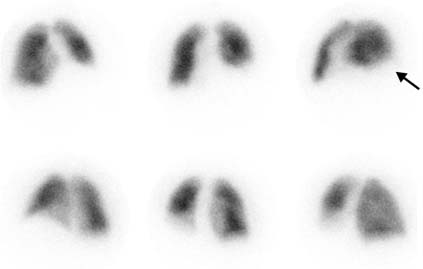
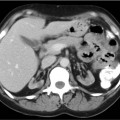
CASE 44 A 26-year-old man presents with shortness of breath and chest discomfort. Fig. 44.1 • A 3.0-mCi dose of 99mTc-MAA is administered intravenously with the patient supine. • The patient should cough and take several deep breaths before administration of the MAA to clear any areas of resting atelectasis. • The patient should breathe normally during tracer injection. • Use a low-energy, all-purpose collimator. • Energy window 20% centered at 140 keV. • Imaging time is 500,000 counts per view. • Matrix size is 128 × 128. • Views are anterior, right anterior oblique, left anterior oblique, posterior, right posterior oblique, and left posterior oblique. Lateral views can also be obtained, although it is important to remember that counts from the contralateral lung will contribute to these views. Homogeneous tracer distribution is seen throughout both lung fields (Fig. 44.1). The lungs are of normal contour. The cardiac silhouette is noted in the left lung field in the anterior projection. • No evidence of pulmonary embolism. There are many causes of shortness of breath or chest pain other than pulmonary embolism. A normal lung scan rules out recent pulmonary embolism. The lung perfusion pattern was normal. Shortness of breath and chest discomfort in this patient were felt to be secondary to anxiety and gastritis. No further follow-up was obtained. Fig. 44.2 Fig. 44.3 Fig. 44.4 Fig. 44.5 Lung perfusion scans provide a method for the diagnosis of pulmonary embolism that is noninvasive and effective. A normal lung scan rules out recent pulmonary embolism. When a perfusion defect is identified, one must first determine the size and anatomic extent of the defect (s) (Table 44.1). Nonsegmental defects do not occupy known vascular distributions and are therefore less likely to be caused by a thromboembolus. Nonsegmental defects include cardiomegaly (Fig. 44.2, arrow), pleural effusion (Fig. 44.3, arrow), a cardiac pacemaker superimposed on the chest wall (Fig. 44.4, arrow), and an elevated hemidiaphragm (Fig. 44.5, arrow; Table 44.1).
Clinical Presentation
Technique
Image Interpretation
Differential Diagnosis
Diagnosis and Clinical Follow-Up
Discussion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree