Infection
Thomas H. Berquist
- Introduction
- Osteomyelitis
- Hematogenous Osteomyelitis
- Osteomyelitis Secondary to Local Extension
- Osteomyelitis in Violated Bone
- Diagnosis
- Treatment
- Complications
- Differential Diagnosis
- Hematogenous Osteomyelitis
- Joint Space Infections
- Radiographic Features
- Radionuclide Imaging
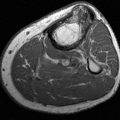
- Magnetic Resonance Imaging
- Ultrasound
- Interventional Techniques
- Treatment
- Differential Diagnosis
- Complications
- Radiographic Features
- Soft Tissue Infections
- Diabetic Foot
- References
Introduction
Infections of the foot and ankle can occur at any age. Clinical presentation varies with the patient’s age, clinical status (i.e., diabetes mellitus, immunosuppression, debilitating disease, postoperative status), location of infection, and type of organism [2,24,27,164,165]. Symptoms may have an abrupt onset or a more chronic or subacute course leading to diagnostic and therapeutic challenges for clinicians and radiologists.
Infections are usually bacterial, but fungal, viral, and parasitic infections may also occur. Infections are usually categorized by site. Osteomyelitis involves the bone, septic arthritis of the joints, infectious tendinitis of the tendon and tendon sheath, and cellulitis of the subcutaneous tissues [24]. Deep soft tissue infection may be severe, resulting in necrotizing fasciitis [148,156,171]. Bursae may also become infected (septic bursitis) [24].
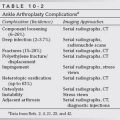
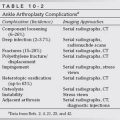
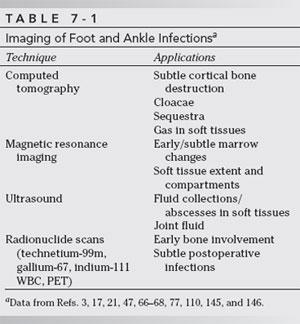
Infections may occur by three routes: (i) direct implantation, such as a puncture wound or surgery; (ii) hematogenous spread; and (iii) spread from a contiguous source such as a diabetic ulcer [24,30,92]. Imaging techniques provide valuable information regarding the extent of involvement (e.g., bone, soft tissue, tendon sheath). The value of each technique differs, depending on the type of infection suspected. The appropriate use of each technique is critical in today’s ever-changing health care environment [149,163]. Table 7-1 provides examples of the advantages of common imaging procedures used to evaluate infection.
This chapter will consider each category of infection separately. Bone, soft tissue, and joint involvement are discussed separately. The final section of this chapter is devoted to infections in the diabetic foot.
OSTEOMYELITIS
The term “osteomyelitis” is reserved for infections involving bone. This term is generally applied to infections whether the cortex, marrow, or periosteum is involved. Infections can be further categorized by describing cortical infection as suppurative periostitis [138]. Sclerosing (Garré’s sclerosing osteomyelitis) osteomyelitis is a term applied to infections that lead to extensive periosteal new bone formation with minimal suppuration [138]. Brodie’s abscess is a localized nidus of infection surrounded by dense bony reaction [22,60,113].
Osteomyelitis may occur via several contamination routes. These mechanisms include (i) trauma or penetrating wounds leading to direct contamination, (ii) bone involvement resulting from spread from a local soft tissue infection, (iii) hematogenous osteomyelitis from organisms reaching bone via the circulation, or (iv) contamination from surgical procedures [24,138]. In the foot, the most common mechanism is trauma, which may lead to direct bone involvement or soft tissue infection and subsequent osteomyelitis [22,24,30,92].
Hematogenous Osteomyelitis
The calcaneus is the most commonly affected bone in the foot. The other tarsal bones and metatarsals are involved less frequently [42,125,130,138]. Hematogenous osteomyelitis is most common in children and older adults [17,122]. Traditionally, hematogenous osteomyelitis has been categorized according to age group (infants, children, and adults) because of differences in clinical and radiographic features [17,18,29,33,36,42,44,138]. The degree of periosteal attachment, vascular anatomy, and variations in the growth plate have a significant impact on the nature of osteomyelitis in these different age groups [24,42,111,151,156].
In infants (less than 1 year of age), vessels in the long bones extend beyond the undeveloped growth plate into the epiphysis. The vessels terminate in the venous lakes similar to the sinusoids in the metaphyseal region of children (Fig. 7-1) [138,151,161]. This vascular pattern accounts, in part, for the higher evidence of epiphyseal and joint space infections in infants with osteomyelitis. If the diagnosis is not established, abnormalities in the growth plate can lead to deformity or cessation of growth [138]. The periosteum is also more loosely attached in infants. Therefore, infections easily elevate and penetrate the periosteum leading to more frequent soft tissue infection and striking periosteal changes on radiographs [24,138,156].
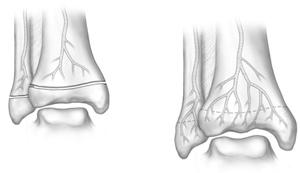
FIGURE 7-1 Illustrations demonstrating vascular patterns at the metaphyseal epiphyseal junction in a child (A) and adult (B).
Metaphyseal and diaphyseal vascular patterns change with development and evolution of the physis (1 to 16 or more years). During this period, the growth plate separates the metaphyseal and epiphyseal blood supply. The metaphyseal vessels in the child are tortuous and form venous lakes in the medullary portion of the metaphysis. Flow rates are reduced in the metaphysis, thus making this region of bone most susceptible to infection [17,78,118,161]. Similar metaphyseal equivalent infections occur near the cartilage in flat and nontubular bones (scapula, ilium, clavicle, calcaneus) in children [125]. Vascular anatomy in these regions is similar to the metaphysis of long bones. Nearly 25% of childhood infections occur in metaphyseal equivalent sites of nontubular bones [24,58,78,138].
The adult vascular pattern evolves with closure of the growth plate (Fig. 7-1B). The metaphyseal vessels enter the epiphysis, thereby allowing infection to involve this region of bone and, more frequently, to enter the adjacent joint space. Periosteum in the adult is more firmly attached, so elevation is more subtle than in children. Infection is more likely to spread along the medullary space. In adults, the spine and bones of the feet are common sites of osteomyelitis [138,161]. Clinically, hematogenous osteomyelitis tends to present with a more abrupt onset (fever, local swelling, limp, or reduced motion in the involved joint) in children [22,111,116,118]. Involvement of multiple sites is more common in infants. In adults, symptoms are often more subtle and only affect one site. Bacteria, mycobacteria, fungi, and viral organisms can all be involved. Staphylococcus aureus is commonly implicated in children and adults, and group B streptococcal organisms are found in infants [8,9].
Osteomyelitis Secondary to Local Extension
Direct extension of soft tissue infection into adjacent bone or joint structures occurs most commonly in the skull, facial bones, and peripheral extremities [88,158]. Initial soft tissue infections may be secondary to burns, penetrating trauma, or soft tissue ulceration and necrosis from diabetes mellitus and ischemic disease [45,53,132].
Infections resulting from puncture wounds in the plantar aspect of the foot are particularly common [93,94,132,166]. Most injuries occur in the barefoot child [92,114]. About 1% of emergency room visits are related to puncture wounds. Up to 15% of these injuries result in infection. Most puncture wounds involve the forefoot (64%), with 25% occurring in the midfoot and 11% in the heel or hindfoot (Fig. 7-2) [92]. Punctures are usually due to nails (80%), needles (7%), wood slivers (4%), and glass (2%) [73,92,132]. Organisms common in the soil, such as Pseudomonas aeruginosa, are commonly isolated [160]. Soft tissue infection is due to S. aureus or S. epidermidis in 75% of cases. P. aeruginosa accounts for only 16% of soft tissue infections but most commonly involves bone [92]. These wounds lead to soft tissue infection with osteomyelitis or joint space infections occurring because of direct extension of the soft tissue process. Osteomyelitis in the calcaneus from heel puncture (blood tests) in infants has also been reported [23].
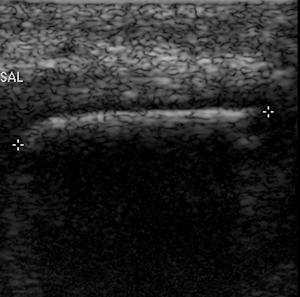
FIGURE 7-2 Ultrasound image demonstrating a wooden foreign body in the plantar aspect of the midfoot.
Frostbite, burns, and other forms of ischemic disease can also affect the soft tissues. Necrotic tissue easily becomes infected. Extension to bone can occur if the condition is not properly treated [138].
Spread of infection in the soft tissues tends to follow the medial, intermediate, or lateral tissue compartments and the tendon sheaths (Fig. 7-3) [62,95,96]. These compartments are created by fibrous septa arising from the plantar aponeurosis [62,144]. The greatest potential space exists in the intermediate or central compartment (Fig. 7-3). Direct contamination to the medial compartment or the lower leg via the flexor hallucis longus can occur [138]. Extension from an infection in the lateral compartment usually enters the dorsal soft tissues of the foot (Fig. 7-3). Medial compartment extension tends to decompress into the intermediate compartment [62,144]. Table 7-2 summarizes the contents and anatomy of the plantar compartments of the foot. The central (intermediate) compartment (Fig. 7-3) is divided by transverse fascia into deep (adductor hallucis muscle) and superficial compartments.
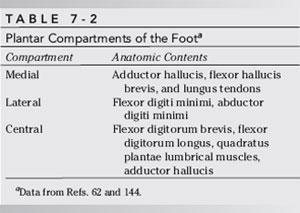

FIGURE 7-3 Illustration of the compartments of the foot and directions infections spread (arrows). 1–5, metatarsals; M, medial compartment; C, central (intermediate) compartment with deep (d) and superficial (s) section; L, lateral compartment.
Osteomyelitis resulting from local soft tissue infection in diabetic patients presents a more complex problem [164,165]. Waldvogel and Popageogion [165] reported that 33% of their patients with osteomyelitis had diabetes. Osteomyelitis was most frequently noted in the phalanges and peripheral joints of the foot. Most patients were 50 to 70 years old. Greenwood [65] noted histories of infection in 25% of diabetic patients, with 10% of diabetic patients presenting with active infection at any given time. Infections tended to develop at pressure points (metatarsal heads and heel), where ischemic changes are more advanced [66]. A more thorough discussion of infections in the diabetic foot occurs in the last section of this chapter.
Osteomyelitis in Violated Bone
Osteomyelitis may develop following surgical procedures, deep puncture wounds that directly involve bone, or open fractures. Diagnoses in these settings may be particularly difficult because of soft tissue injury and the presence of distorted bony anatomy [66,83]. The latter may result from fracture or orthopaedic manipulation and the presence of orthopaedic fixation devices or prosthesis. This mechanism of contamination is not unlike that of direct puncture or infection from an adjacent source.
Diagnosis
Early detection of osteomyelitis can be difficult. The patient’s age, mechanism of contamination, offending organism, previous or current medications, and other factors may affect the clinical and radiographic features of the disease process [1,152,156,161]. Infection following orthopaedic procedures may be particularly difficult to evaluate [66,83].
Clinical features of osteomyelitis differ in infants, children, and adults. Infants generally present with swelling and may be unwilling to move the involved extremity. Children (1 to 16 years old) usually present with a more aggressive clinical picture including high fever, localized pain, swelling, and redness over the site of involvement. In adults, symptoms can be subtle. Laboratory studies may reveal an elevated erythrocyte sedimentation rate and leukocytosis, but blood cultures may be negative in up to 50% of patients [66,86].
Imaging features of osteomyelitis vary with age, clinical setting, and the imaging modality selected. Early diagnosis and treatment are essential to avoid chronic infection and potential complications.
Radiographs (CR Images)
The earliest radiographic features of acute hematogenous osteomyelitis are due to soft tissue changes [138]. These changes are subtle and may only be evident if comparison views of the uninvolved extremity are obtained. Computed radiographic images are easily manipulated on the imaging workstation. Therefore, soft tissues can be more easily evaluated. Swelling of the deep soft tissues adjacent to the involved bone develops 2 to 3 days after the onset of acute hematogenous osteomyelitis. This swelling results in irregularity or displacement of the deep fat planes. Diagnosis at this stage may lead to complete resolution before bone changes develop. As soft tissue involvement progresses, the deep tissue involvement becomes more superficial. This feature is useful in differentiating osteomyelitis from cellulitis. Cellulitis involves the superficial tissues initially and is more commonly noted in infections resulting from puncture wounds. If the infection is not treated, the process progresses to involve the deep tissues, periosteum, cortex, and finally the medullary bone. This is a reversal of the pattern seen with hematogenous osteomyelitis (Fig. 7-4) [138].



FIGURE 7-4 Soft tissue changes due to infected puncture wound. AP (A), lateral (B), and oblique (C) radiographs show soft tissue swelling and increased soft tissue density (open arrows). No bone involvement is evident.
Bone changes are not usually evident for 10 to 14 days or until 35% to 50% of the bone has been destroyed [40,138]. Bone and periosteal abnormalities vary with patient’s age, the type of bone involved, and the organism. There are also subtle differences depending on the clinical presentation (acute, subacute, or chronic). The most common bacterial organism identified in hematogenous osteomyelitis is S. aureus (81% to 92% of cases) [138]. Beta-hemolytic streptococcal infections are not uncommon in infants [33,73,108,138]. Other organisms are identified less frequently, although pneumococcal, gonococcal, and meningiococcal infections do occur. These organisms and certain gram-negative bacteria (Escherichia coli, P. aeruginosa, Klebsiella, and Aerobacter) are more common in debilitated patients, such as those with alcoholism, diabetes, or hypogammaglobulinemia [40,45,49,57,73,86,88,109,138].
Generally, the radiographic changes resulting from acute osteomyelitis do not allow the causative organism to be identified [20,25,138]. In infants (less than 1 year old), lytic areas appear in the metaphysis of the tubular bones or calcaneus near the tuberosity. Impressive periosteal reaction and soft tissue abscess formation may develop along tubular bones. The latter are due to the loosely attached periosteum in this age group. Joint space involvement is also common because of the vascular communication between the metaphysis and epiphysis. Sequestra may also be evident. These features are often better demonstrated with computed tomography (CT). Children have similar radiographic features, except the growth plate and vascular anatomy reduce the incidence of epiphyseal and joint space involvement in the foot and ankle (Figs. 7-5 through 7-7) [110,111,113,115–117].

FIGURE 7-5 AP view of the ankle in a child with classic osteomyelitis. There are lytic areas in the fibular metaphysis with periosteal new bone formation. The epiphysis is normal.


FIGURE 7-6A) Lateral view of the left foot is normal. B) Lytic changes (arrows) adjacent to the right calcaneal growth plate due to osteomyelitis.

FIGURE 7-7 Lateral radiograph of the lower leg demonstrates a permeative pattern in the anterior cortex and marrow due to osteomyelitis.
Acute hematogenous osteomyelitis in adults may involve the epiphysis, metaphysis, or diaphysis [20,24,138]. Epiphyseal involvement results in more frequent extension into the joint space (Fig. 7-8). Periosteal changes are less obvious because the periosteum is more firmly attached to bone in adults than in infants and children. Progression into cortical and periosteal tissues can lead to soft tissue abscess and fistula formation [138].

FIGURE 7-8 Lateral (A) and AP (B) views of the ankle demonstrate a large effusion (curved arrows) with destructive changes in the talus due to osteomyelitis extending into the joint space.
Subacute or chronic osteomyelitis may develop when diagnosis is delayed or the infection is improperly treated. There is no distinct method of separating these categories of infection, although chronic infection is the term applied to infections of more than 6 weeks’ duration [24]. Again, radiographic features vary depending on the organism, type of therapy, and the presence of other underlying diseases (Figs. 7-9–7-11). The periosteal changes may be extensive, forming a dense involucrum (sclerotic layer of bone usually around sequestra) that surrounds the shaft of tubular bones (Fig. 7-11). Small perpendicular cortical tunnels or cloacae may be present that result when necrosis extends through the bone. When this occurs, radiographs may demonstrate adjacent abscesses in the soft issues [138]. Areas of necrotic or dead bone may also be evident. Radiographically, these sequestra are often more dense than the surrounding osteoporotic or hyperemic bone that surrounds them in the medullary or cortical regions. This appearance results from devascularization of sequestra, which prevents these islands of bone from participating in the usual hyperemic changes responsible for osteoporosis or lucency in the vascularized bone [133]. Granulation tissue and suppuration also surround sequestra [138]. Sequestra are usually not evident for at least 3 weeks, and size variation may make them difficult to identify using conventional radiographs. CT is most useful in the identification of subtle sequestra [24,138].


FIGURE 7-9 AP (A) and oblique (B) radiographs demonstrate scleroses and thickening of the cortex and trabeculae of the lateral cuneiform and third metatarsal with loss of joint space due to chronic osteomyelitis and joint space infection.

FIGURE 7-10 Mixed lytic and sclerotic changes in the cuboid due to chronic osteomyelitis.

FIGURE 7-11 Lateral view of the foot shows chronic osteomyelitis of the fifth metatarsal. Changes are secondary to a previous nail puncture with Pseudomonas infection.
In certain cases, infection does not lead to necrosis, but instead causes sclerotic nonpurulent changes [138]. The term Garré’s sclerosing osteomyelitis should be used in this setting. This type of response is more common in the mandible and long bones of the lower extremity than in the foot (Fig. 7-12) [138].

FIGURE 7-12 AP views of the foot demonstrate sclerosing osteo myelitis in the first through third metatarsals. There are also chronic destructive changes in the first metatarsophalangeal joint and collapse of the third and fourth metatarsal heads.
Localized abscesses (Brodie’s abscess) also occur. Patients are usually not systemically ill and often have symptoms for weeks or months. The distal tibia is a common site of involvement. These abscesses are usually due to S. aureus, but in up to 50%, no organism can be identified [113]. Abscesses are usually metaphyseal (60%), well marginated with dense surrounding sclerosis, and range from 4 mm to 4 cm in size (Fig. 7-13). Central sequestra have been identified in up to 20% of patients [113]. When cortical involvement occurs, these lesions present radiographically as a small, lucent nidus surrounded by dense cortical reaction, a feature not unlike osteoid osteoma. Diaphyseal involvement may also occur, especially in adults (Fig. 7-14) [138]. Abscesses may have a serpiginous tract that communicates with the growth plate [60].

FIGURE 7-13 AP view of the ankle showing a large metaphyseal Brodie’s abscess (arrows).
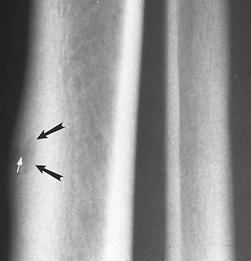
FIGURE 7-14 Small oval Brodie’s abscess (black arrows) with cortical thickening. There is also a sinus tract (white arrow).
As mentioned earlier, most pyogenic bacterial infections have similar radiographic features. However, certain organisms (i.e., mycobacteria, fungi) have different radiographic and clinical features.
Salmonellosis.
Salmonella (S. typhi, S. paratyphi, S. choleraesuis, S. typhimurium, and S. arizonae) can involve bone (approximately 1%) [138,156]. Osteomyelitis due to Salmonella occurs more commonly in patients with sickle cell disease or other hemoglobinopathies, leukemia, lymphoma, and systemic lupus erythematosus [38,138,156]. The exact mechanism of contamination in Salmonella osteomyelitis is uncertain. Patients with sickle cell disease probably develop hematogenous osteomyelitis resulting from bowel infarcts that allow organisms to enter the circulation. Osteomyelitis due to Salmonella has a predilection for the medullary region of the diaphysis and areas of bone infarction [27,49,138].
Tuberculosis.
Tuberculosis osteomyelitis can involve patients in all age ranges, but it is rare in infants [70,126]. Bone and joint involvement occurs in 3% to 5% of patients with tuberculosis (Fig. 7-15) [43,126,138]. Osseous and joint involvement in the foot and ankle is uncommon. Only 0.1% to 0.3% of all extrapulmonary tuberculosis involves the foot and ankle [43]. Dhillon and Nagi reported foot and ankle involvement in 74 patients over an 11.5-year period [43]. The calcaneus was most commonly involved followed by the midfoot and ankle [43]. The infection is more common in the presence of debilitating disease and drug addiction and in certain groups of immigrants [138]. Mycobacterium tuberculosis is contracted via inhalation, whereas M. bovis was common following ingestion of contaminated milk products [48,126]. The latter accounted for up to 20% of musculoskeletal tuberculosis in the past, but it has been largely eradicated. M. tuberculosis still accounts for some cases of infectious arthropathy (spine, hip, knee), but less frequently it causes primary osteomyelitis. When present, the disease usually presents with hematogenous dissemination to the metaphyseal region of long bones in children and the epiphysis in adults. Pulmonary involvement is evident in 50% of patients. The shafts of the metatarsals (tuberculous dactylitis) may show obvious layered periostitis (Fig. 7-16). This type of osteomyelitis is most common in children but has been described in adults [46,52,127]. Multiple metatarsals may be involved in up to 33% of patients. Congenital syphilis can produce a similar radiographic appearance, but it typically involves both feet and ankles and there is less soft tissue swelling than with tuberculous dactylitis [52,127].
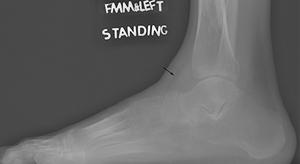
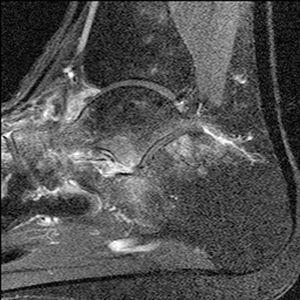
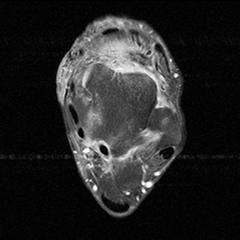
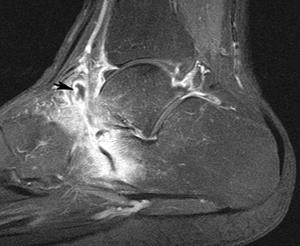


FIGURE 7-15 Multifocal tuberculosis. A) Lateral radiograph demonstrating marked osteopenia of the ankle, hindfoot, and midfoot. There is also an ankle effusion (arrow). B) Sagittal T2-weighted image demonstrates periarticular edema and axial (C) and sagittal (D) postcontrast fat-suppressed T1-weighted images demonstrate the extensive bone and soft tissue involvement with synovial enhancement (arrow). Sagittal T1- (E) and T2-weighted (F) images demonstrate disc and osseous involvement at T12-L1 (arrow).

FIGURE 7-16 AP radiographs of the feet demonstrate periosteal thickening and sclerosis of the left first metatarsal due to tuberculosis. The laminated appearance of the perio – steum is common with tuberculosis.
Dhillon and Nagi reported that osteopenia was the most common radiographic finding (Fig. 7-15) [43]. Circumscribed lytic lesions (cystic tuberculosis) may also be evident, although these changes are more common in the large long bones of the lower extremity than the foot. These lesions may be difficult to differentiate from eosinophilic granuloma, sarcoidosis, cystic angiomatosis, and plasmacytomas [127].
Syphilis.
The organism of syphilis, Treponema pallidum, is a spirochete that may be transmitted transplacentally or by sexual contact in adults. The organism reaches the musculoskeletal system via the circulation. Bone involvement in the neonate may include the diaphysis and metaphysis. The process is usually symmetric (Fig. 7-17) [39,139].
Spirochetes inhibit bone formation, thereby resulting in osteoblastic degeneration. If the infant survives, bone manifestations include widening of the zone of provisional calcification, lucent bands similar to those seen with leukemia or neuroblastoma, and periosteal new bone formation (see Fig. 7-17). These changes are usually symmetric and involve multiple long bones compared with osteomyelitis resulting from more common organisms, which is generally local and asymmetric (see Fig. 7-17) [39]. Syphilitic lesions may regress only to reappear in 5 to 20 years. At this time, the changes resemble the adult form of the disease. The adult or acquired form of syphilis affects the skeleton in 0.5% to 20% of patients. This hematogenous involvement leads to periosteal new bone formation that is generally laminar and evolves into cortical thickening with areas of lytic necrosis (Fig. 7-18). The skull is involved in up to 9% of patients [138]. The tibia and foot are also frequently involved (see Figs. 7-17 and 7-18). These lytic areas or gummas do not appear for several years. Histologically, one sees caseating necrosis and giant cells resembling a tubercle. Less commonly, dactylitis, similar to that seen in tuberculosis, develops in the tubular bones of the hands and feet [138,139].
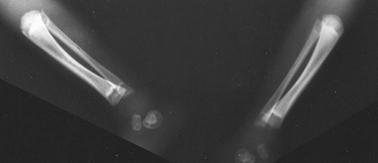
FIGURE 7-17 Leg and ankle radiographs in a neonate with congenital syphilis. Note the symmetric periosteal new bone formation.

FIGURE 7-18 AP and lateral views of the leg and ankle demonstrate neurotrophic arthropathy with talar tilt. There is marked periosteal new bone formation on the tibia and distal fibula with a midtibial gumma (arrow).
Fungal Infections.
Osteomyelitis of fungal origin should be considered in debilitated patients, diabetic patients, patients taking steroids, and patients with osteomyelitis who reside in certain geographic regions. Actinomycosis (Actinomyces israelii or A. bovis) is present in the oral cavity. Osseous involvement generally results from local extension, but hematogenous spread can also occur [127,138,140]. Obviously, local extension most commonly involves the facial bones. Involvement of the foot and ankle is uncommon.
Cryptococcosis (Cryptococcus neoformans) can be acquired by direct implantation into open wounds in the foot because the organism is present in the soil. Skeletal involvement is reported in 5% to 10% of patients [101]. Destructive bone lesions are commonly associated with draining sinuses [101,168].
Blastomycosis (Blastomyces dermatiditis) is prevalent in the Ohio and Mississippi River valleys. Contamination can occur via the skin or by inhalation, which leads to pulmonary involvement. Thus, osteomyelitis may follow direct or hematogenous contamination. Skeletal involvement occurs in up to one half of patients with pulmonary involvement. The tibia and tarsal bones are commonly affected [32]. Radiographically, there are patchy destructive lesions and draining sinuses. Whitehouse and Smith [167] suggested that lytic bone lesions, soft tissue infection, and pulmonary disease should suggest the diagnosis of blastomycosis.
Coccidioidomycosis (Coccidioides immitis) is an inhalation disease endemic in the southwestern portion of the United States [19,25,37,133]. Bone involvement occurs frequently (10% to 20%) [167]. About one third of cases initially present with transient polyarthritis [19,37]. Areas of bony prominence, such as the calcaneal tuberosity, and the diaphysis of the metatarsals are common sites of involvement (Fig. 7-19). Involvement is often symmetric with aggressive periostitis, unlike osteomyelitis resulting from more typical organisms [37,138,167]. Associated pulmonary involvement is common [167].

FIGURE 7-19 Coccidioides immitis osteomyelitis. Lateral view of the calcaneus shows marked soft tissue swelling posteriorly (open arrows) with lytic destructive changes on the calcaneus, talus, and tibia.
Histoplasma capsulatum and H. duboisii are present in the soil, contaminating the lungs (histoplasmosis) initially. The axial skeleton is more commonly involved than the foot and ankle. Children are affected more frequently than adults [89,133].
Other fungal infections that may affect the foot and ankle include sporotricosis, candidiasis, mucormycosis, and aspergillosis [138]. Multiple lytic lesions, usually eccentric and well marginated, are typical. Radiographic changes do not vary significantly from those described earlier.
Miscellaneous Infections.
Leprosy may also cause osteomyelitis and neuropathic arthropathy in the foot [50]. Osteomyelitis develops in 3% to 5% of patients following a long (3- to 6-year) incubation period. The process usually follows soft tissue involvement, so bone involvement begins in the periosteum [50,138]. The phalanges are most commonly involved. Differentiation of the neurotrophic changes from chronic infection is difficult radiographically [50].
Neuropathic changes in leprosy occur with infection of the neural structures and soft tissues [71]. In a large series reported by Horibe et al. [71], 40 of 449 patients with leprosy demonstrated clinical and radiographic (Fig. 7-20) evidence of neuropathic arthropathy. The ankle, midtarsal, tarsometatarsal, and subtalar joints are involved in decreasing order of frequency [71].



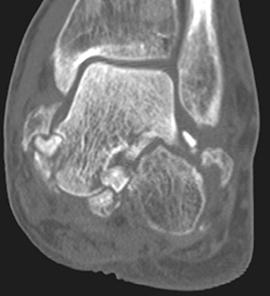

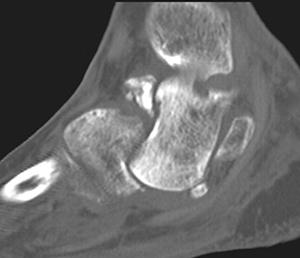
FIGURE 7-20 Neuropathy in the hindfoot due to leprosy. AP (A) and lateral (B) radiographs demonstrate advanced neuropathic arthropathy in a 50-year-old nondiabetic male. Note the near vertical position of the talus. Axial (C) coronal (D), and sagittal (E,F) CT images demonstrate the bony fragmentation to better advantage.
Rubella and cytomegalic inclusion disease can present with similar radiographic findings in neonates infected during the first trimester of pregnancy [138,142]. Periosteal changes, if present, are not usually as dramatic as in congenital syphilis (see Fig. 7-17). The long bones are most commonly affected. Mixed lucent and sclerotic changes in the metaphysis result in a “celery stalk” appearance (see Fig. 7-21). With healing, a prominent line often forms at the metaphyseal margin [138,142]. Adults and older children rarely have radiographic findings, even though clinical arthropathy has been described [138].

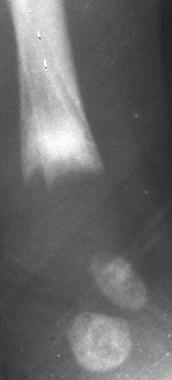
FIGURE 7-21 AP (A) and lateral (B) radiographs demonstrate sclerotic changes with celery stalk appearance due to rubella infection in a neonate.
Parasitic infections rarely affect the skeleton. Soft tissue involvement with subsequent cystic calcification can develop. This feature is more common with cysticerosis (Taenia solium) and trichinosis (Trichinella spiralis). Ecchinococcus granulosus may involve the adult skeleton in 1% to 2% of patients. Radiographically, areas of involvement are cystic with central trabeculation. Cortical expansion may also be evident [138].
Radiographic features of osteomyelitis differ if the source is a contiguous infection rather than an infection acquired by the hematogenous route (see Figs. 7-2 and 7-5). Bone involvement following contiguous infection generally follows local trauma, vascular insufficiency, or other devitalizing mechanisms that allow soft tissues to become infected (see Fig. 7-3). The plantar surface of the foot is frequently involved [53,95,96,138]. Anatomic studies have demonstrated that the deep layers of the midplantar intermuscular planes and the tendon sheaths are most commonly involved in spread of these infections [144]. P. aeruginosa is present in the soil and is frequently implicated. The earliest radiographic findings are swelling and distortion of the plantar fat and septa. As with hematogenous infection, the radiographic features are not usually evident for 10 to 21 days. Bone involvement begins in the periosteum and outer cortex, unlike hematogenous osteomyelitis, which typically involves the metaphyseal marrow. Ledermann et al. [95,96] reported that the first and fifth metatarsal are most commonly involved in patients with osteomyelitis associated with foot ulcers. In these patients, there was associated joint space infection in 33% [95]. Periosteal changes are more common in children because of the loose periosteal attachment.
Radiographic findings in osteomyelitis following surgical intervention or fracture may be especially subtle. After acute fracture, necrosis of osteocytes occurs at the fracture line extending to the area of closest vascular supply. This causes widening and some irregularity of the fracture line. Complex or comminuted fractures may have multiple fragments at the fracture site. Some of these fragments may lose their blood supply and resemble sequestra. Additional confusion may occur because of the osteoporosis that occurs with immobilization. The degree of periosteal callus is variable depending on the extent of injury and size of the hematoma adjacent to the fracture site. In the foot and ankle, hematomas are generally smaller than in the thigh or calf, so callus is generally less exuberant [17].
Sequential radiographs are useful in following the progress of normal fracture healing. Any variation in the normal sequence of radiographic or clinical findings such as delay in union, local pain, erythema, or swelling may suggest infection [17]. Radiographic features (Figs. 7-22 and 7-23) are similar to those mentioned earlier, but they may be obscured by architectural changes near the fracture. This can reduce the confidence in radiographic findings and delay diagnosis. CT, MR imaging, and isotope studies (see next sections) may be most useful in this setting (Fig. 7-24) [20,63,119,146].