7 Venous Occlusive Diseases
7.1 Deep Venous Thrombosis
7.1.1 Clinical Case
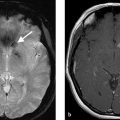
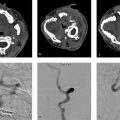
A 45-year-old female, loss of consciousness (Fig. 7.1).
7.1.2 Description of Imaging Findings and Diagnosis
Diagnosis
Restricted diffusion in the bilateral thalami and basal ganglia with extensive venous sinus thrombosis affecting superior sagittal sinus and the deep venous system.
7.1.3 Background
Deep cerebral venous thrombosis is a subset of cerebral vein thrombosis with similar risk factors and epidemiology. Presentation is often substantially more severe than superficial venous thrombosis and includes nausea, vomiting, headache, focal neurological deficit, loss of consciousness, neuropsychiatric symptoms, or seizures. Treatment is generally systemic anticoagulation, even in the presence of hemorrhage. Compared to dural venous sinus thrombosis (DSVT), deep cerebral vein thrombosis carries a much poorer prognosis.
7.1.4 Imaging Findings
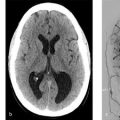
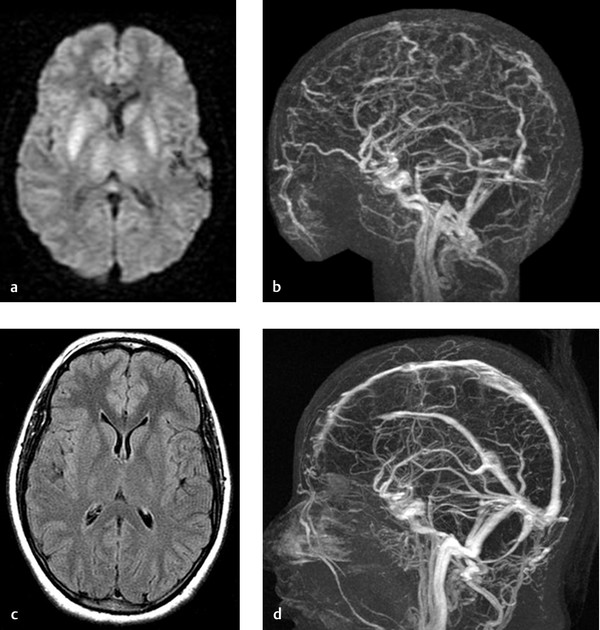
Diagnosis of deep cerebral vein thrombosis is difficult because of the unspecific presentation and the wide variety of differential diagnoses. Typical imaging findings on non-contrast CT include edema of deep structures including the bilateral thalami and basal ganglia with or without hemorrhage and hyperdense clot in the internal cerebral veins and straight sinus (Fig. 7.2). Occasionally, the parasagittal cortex can be involved. Unilateral venous thrombosis is rare, but not unheard of. On MRI, T2-weighted images demonstrate hyperintense swelling of the deep gray structures with possible high T1 signal or hemosiderin deposition indicating hemorrhage. Clot can be identified as linear hyperintense material filling the veins. Acute clot is T2 hypointense and can mimic vascular flow voids. SWI or GRE imaging can be very helpful in confirming the presence of thrombus by identifying blooming artifact. Diffusion weighted imaging (DWI) confirms the presence of predominantly vasogenic edema in the affected regions. Vascular imaging is useful in confirming the diagnosis. MR and CT venography will demonstrate the lack of flow in the deep cerebral veins. It is important for neuroradiologists to comment on extension of thrombus into the dural venous sinuses as well.
The preferred treatment of deep venous thrombosis is anticoagulation therapy. Follow-up imaging is essential in these patients to document resolution of the thrombus. Oftentimes, there is complete recanalization of the occluded vein after several weeks of therapy. This is often accompanied by resolution of parenchymal injury on T2 and DWI (Fig. 7.1).
Differential considerations are manifold and include artery of Percheron infarct (which should demonstrate cytotoxic rather than vasogenic edema on DWI and be confined to the thalamotuberal regions) and bithalamic glioma. In the setting of an artery of Percheron infarct, multiple small patchy infarcts are seen in both thalami rather than the contiguous T2 signal and edema seen in a deep venous thrombosis (Fig. 7.3). Bithalamic gliomas are exceedingly rare. It is important to point out that occasionally, deep cerebral venous thrombosis affects only one hemisphere. Other differential considerations include infectious diseases such as West-Nile Virus encephalitis, CJD, or Japanese Virus Encephalitis; or toxic-metabolic disorders (including acute Wilson Crisis, Carbon Monoxide Poisoning, Leigh Syndrome, etc.) (Fig. 7.3). Clinical history as well as meticulous imaging interpretation are important to make the diagnosis.


7.1.5 What the Clinician Needs to Know
Extent and location of thrombus including involvement of the superficial venous system
The presence of edema in deep gray matter structures and reversibility on follow-up imaging
Hemorrhage
A broad range of differential diagnoses
7.1.6 High-yield Facts
Deep cerebral vein thrombosis classically presents with diffuse bithalamic swelling but a unilateral presentation is not unheard of.
Thrombus is hyperdense on CT and T1 hyperintense on MRI. Blooming artifact is present on GRE/SWI.
CT/MR venography can be confirmatory.
After several weeks of anticoagulation therapy, revascularization of the occluded vein and reversal of parenchymal imaging findings can occur.
Further Reading
[1] Steven A, Raghavan P, Altmeyer W, Gandhi D. Venous Thrombosis: Causes and Imaging Appearance. Hematol Oncol Clin North Am. 2016; 30(4):867–885 [2] Lin N, Wong AK, Lipinski LJ, Mokin M, Siddiqui AH. Reversible changes in diffusion- and perfusion-based imaging in cerebral venous sinus thrombosis. J Neurointerv Surg. 2016; 8(2):e67.2 Cortical Vein and Dural Venous Sinus Thrombosis
7.2.1 Clinical Case
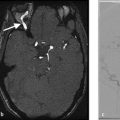
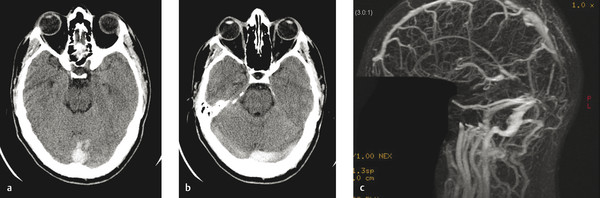
A 55-year-old male with left-sided headache and garbled speech (Fig. 7.4).

7.2.2 Description of Imaging Findings and Diagnosis
Diagnosis
Left temporal lobe edema and hemorrhage secondary to cortical vein thrombosis (CVT).
7.2.3 Background
DSVT is a relatively common cause of infarction and hemorrhage in the young- and middle-aged population. Its prevalence is higher in females. Common risk factors include oral contraceptive use, pregnancy, trauma, coagulation disorders, infection, dehydration, and compressive mass. In about 10% of cases, the cause is unknown. Clinical presentation of DSVT can include headaches, decreased levels of consciousness, altered vision, elevated intracranial pressure, seizures, coma, and death. The pathophysiology of DSVT is related to venous hypertension from poor venous outflow as well as impaired CSF resorption, which can be exacerbated if thrombosis affects the arachnoid granulations as well. Cerebral venous infarction and hemorrhage can occur in up to 50% of cases.
CVT often accompanies DSVT. Isolated CVT is, however, rare. Isolated CVT can present with localized subarachnoid hemorrhage (SAH) with or without parenchymal involvement, edema, or venous infarct.
7.2.4 Imaging Findings
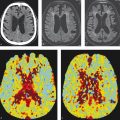
Any of the dural venous sinuses can be affected by DSVT, including the cavernous sinus. In general, findings of DSVT are first identified on non-contrast CT where one can identify hyperdensity of the sinus in the form of a cordlike hyperattenuation with or without underlying cortical edema or peripheral venous hemorrhage (Fig. 7.5). It is important to note that the distal superior sagittal sinus or one of the transverse sinuses may be congenitally absent, thus mimicking dural sinus thrombosis on MRV or CTV. CT venography has a sensitivity of 95% for identifying DSVT with common imaging findings being a filling defect in the sinus, gyral enhancement, and prominent intramedullary veins.
On MRI, conventional spin echo sequences demonstrate loss of the normal flow void of the dural sinuses. In the acute phase, clot is isointense on T1 and hypointense on T2. The clot becomes hyperintense on T1 in the subacute phase (Fig. 7.4). SWI or GRE can identify clot by the presence of blooming artifact. Conventional MRI sequences can be very sensitive and specific in identifying DSVT. MRV will demonstrate lack of flow.
Isolated CVT is a commonly missed diagnosis. There is wide variability in the number, size, and location of cortical veins. Each individual hemisphere can have variations in the size and location of Labbe, Trolard, and the superficial middle cerebral vein, not to mention the smaller cortical veins. Non-contrast CT is usually normal, but occasionally an isolated hyperdense cortical vein can be identified. Because the anatomy of the cerebral venous system is inconstant, MRV, and CTV are not usually helpful unless there is extension of the thrombus into a dural sinus. On MRI, SWI or GRE will demonstrate blooming at the site of the thrombosed vein, T1 hyperintensity, and T2/FLAIR hypointensity. While the T2 and T1 signal changes normalize over time, blooming artifact on T2* weighted imaging can persist for several months. Most common secondary findings include local edema and petechial hemorrhage or hematoma.
In addition to evaluating for direct signs of CVT or DSVT, the radiologist should inspect for secondary signs and sequelae. Identification of cortical infarction in a non-arterial location supports the diagnosis of venous thrombosis. Heterogeneous or gyriform cortical or peripheral hemorrhage along with cortical edema are important to identify (Fig. 7.6). Although the majority of the T2 hypersignal is NOT restricting on DWI (given its vasogenic nature), there may be cortical or gyriforme DWI restriction, which is related to compression of the leptomeningeal perforators due to the compressive vasogenic edema. Follow-up imaging is necessary to document resolution of the thrombus as well as any long-term sequelae, including venous sinus stenosis and development of dural arteriovenous fistulae (further described in other chapters).
There are a few pitfalls to diagnosis of DSVT. Hypoplasia or atresia of the transverse sinus is a relatively common normal anatomic variant (Fig. 7.7). In most patients, the right transverse sinus is larger than the left. There are a few complimentary imaging findings, which can help one determine if a sinus is congenitally small. First, one should inspect the ipsilateral jugular foramen. If the ipsilateral jugular foramen is small then the transverse sinus is likely hypoplastic. Another trick is the so-called Gibraltar Sign, named after the Rock of Gibraltar which has a gradual, asymmetric slope. The bony groove for the superior sagittal sinus often slopes to one side (usually the right). The direction which the bony groove slopes is usually the side of the dominant sinus. Arachnoid granulations are commonly overcalled as thrombus. However, these are usually well-defined focal filling defects within the sinus, are located in the lateral aspects of the transverse sinus, and have CSF signal intensity (Fig. 7.8).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree