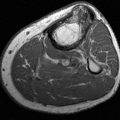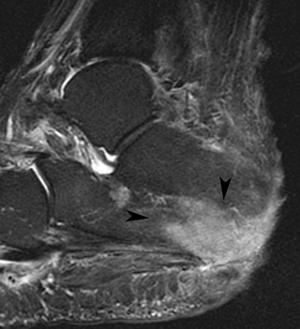
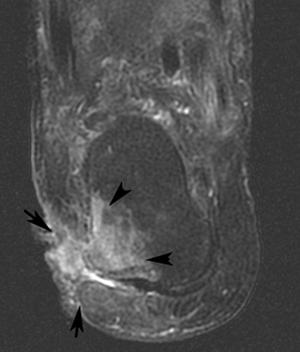
FIGURE 7-59 Soft tissue infection progressing to osteomyelitis. Axial (A), sagittal (B), and coronal water-sensitive MR sequences demonstrate the soft tissue wound (arrows) leading to osteomyelitis in the calcaneus (arrowheads).
Deep soft tissue and bone and joint involvement must be treated more aggressively. Deep infections may be caused by the organisms noted earlier. However, multiple organisms, including anaerobic organisms, are more often cultured in deep infection (60% of cases) [47,98]. Surgical intervention is often extensive in these patients. Unfortunately, culture material from sinus tracts and superficial ulcers is often inaccurate. Accuracy rates may be as low as 49% [97,98]. Therefore, examination of deep tissue specimens or bone biopsy is usually necessary to isolate the organism or organisms [14,57]. Before surgical planning, it is also important to be certain the blood supply is adequate. This may be accomplished with noninvasive techniques, MR angiography, or conventional angiographic techniques [34,52]. Tissue debridement, amputation of specific digits or forefoot segments, or more proximal amputation can be planned appropriately with accurate vascular mapping.
REFERENCES
- Ahmadi ME, Morrison WB, Carrino JA, et al. Neuropathic arthropathy of the foot with and without superimposed osteomyelitis: MR imaging characteristics. Radiology. 2006;238:622–631.
- Alldred AJ, Nesbit NW. Hydatid disease of bone in Australia. J Bone Joint Surg. 1964B;46:260–267.
- Al-Sheikh W, Sfakianakis GN, Mnaymneh W, et al. Subacute and chronic bone infection. Diagnosis using In-111, Ga-67, Tc-99m MDP bone scintigraphy and radiography. Radiology. 1985;155:501–506.
- Ang JGP, Gelfand MJ. Decreased gallium uptake in acute hematogenous osteomyelitis. Clin Nucl Med. 1983;8:301–303.
- Anzilotti K, Schweitzer ME, Hecht P, et al. Effect of foot and ankle MR imaging on clinical decision making. Radiology. 1996;201:515–517.
- Arnold PG, Irons GB. Lower extremity muscle flaps. Orthop Clin North Am. 1984;15:441–449.
- Ash JM, Gilday DL. The futility of bone scanning in neonatal osteomyelitis. J Nucl Med. 1980;21:417–420.
- Autto JH, Ayoub EM. Streptococcal osteomyelitis and arthritis in the neonate. Am J Dis Child. 1978;129:1449–1451.
- Averill LW, Hernandez A, Gonzalez L, et al. Diagnosis of osteomyelitis in children: utility of fat-suppressed contrast-enhanced MRI. Am J Roentgenol. 2009;192:1232–1238.
- Azouz EM. Computed tomography in bone and joint infections. Can Assoc Radiol. 1981;3:102–106.
- Beltran J, Campanini S, Knight C, et al. The diabetic foot. Magnetic resonance imaging evaluation. Skeletal Radiol. 1990;19:37–41.
- Beltran J, McGhee RB, Shaffer PB, et al. Experimental infections of the musculoskeletal system evaluation with MR imaging and Tc-99m MDP and Ga-67 scintigraphy. Radiol. 1988;167:167–172.
- Beltran J, Noto AM, Herman LT, et al. Joint effusions. MR imaging. Radiology. 1986;158:133–137.
- Berendt AR, Peters EJG, Bakker K, et al. Specific guidelines for treatment of diabetic foot osteomyelitis. Diabetes/Metab Res Rev. 2008;24(suppl):S190–S191.
- Berkowitz ID, Wenzel W. “Normal” technetium bone scans in patients with acute osteomyelitis. Am J Dis Child. 1980;134:828–830.
- Berney S, Goldstein M, Bishko F. Clinical and diagnostic features of tuberculous arthritis. Am J Med. 1972;53:36–42.
- Berquist TH. MRI of the Musculoskeletal System. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- Bessler EL, Conway JJ, Weiss SC. Neonatal osteomyelitis examined by bone scintigraphy. Radiology. 1984;152:685–688.
- Bisla RS, Taher TH. Coccidiomycosis of bone and joints. Clin Orthop. 1976;121:196–204.
- Bliznak J, Ramsey J. Emphysematous septic arthritis due to E. coli. J Bone Joint Surg Am. 1976;59:145–145.
- Boerman OC, Rennen H, Oyen WJG, et al. Radiopharmaceuticals to image infection and inflammation. Semin Nuc Med. 2001;31:286–295.
- Bonakdapour A, Gaine VD. Radiology of osteomyelitis. Orthop Clin North Am. 1983;14:21–37.
- Borris LC, Helleland H. Growth disturbance in the hind foot following osteomyelitis of the calcaneus in the new born. J Bone Joint Surg Am. 1986;68:32–35.
- Boutin RD, Joachim B, Sartoris DJ, et al. Update of imaging of orthopedic infections. Orthop Clin North Am. 1998;29:41–66.
- Bried JM, Speer DP, Shehah ZM. Coccidiodes immitis osteomyelitis in a 12 month old child. J Pediatr Orthop. 1987;7:328–330.
- Brower AC. Septic arthritis. Radiol Clin North Am. 1996;34:293–310.
- Brown JT, Miller A. Peroneal tenosynovitis following acute gonnoccal infection. Am J Orthop. 1996;25:445–447.
- Bybee JD, Rogers DE. Phagocytic activity of polymorphonuclear leukocytes obtained from patients with diabetes mellitus. J Lab Clin Med. 1964;64:1–13.
- Capitano MA, Kirkpatrick JA. Early roentgen observations in acute osteomyelitis. Am J Roentgenol. 1970;188:488–496.
- Caputo GM, Cavanaugh PR, Ulbrecht JS, et al. Assessment and management of foot disease in patients with diabetes. N Engl J Med. 1994;331:854–860.
- Chandnani VP, Beltran J, Morris CS, et al. Acute experimental osteomyelitis and abscesses. Detection with MR imaging versus CT. Radiology. 1990;174:223–226.
- Cherniss, EI, Waisbren, BA. Blastomycosis osteomyelitis. A clinical study of 40 cases. Ann Intern Med. 1956;44:105–123.
- Chilton SJ, Aftimos SF, White PR. Diffuse skeletal involvement of streptococcus osteomyelitis in the neonate. Radiology. 1988;134:390.
- Chomel S, Douek P, Moulin P, et al. Contrast-enhanced MR angiography of the foot: anatomy and clinical application in diabetes. Am J Roentgenol. 2004;182:1435–1442.
- Chused MJ, Jacobs WM, Sty JR. Pseudomonas arthritis following puncture wounds of the foot. J Pediatr. 1979;94:429–431.
- Clarke AM. Neonatal osteomyelitis. A disease different from osteomyelitis in older children. Med J Aust. 1958;1:237–239.
- Conaty JP, Biddle M, McKeever FM. Osseous coccidiodal granuloma. J. Bone Joint Surg Am. 1959;41:1109–1122.
- Craig JG, Amin MB, Wu K, Eyler WR, et al. Osteomyelitis of the diabetic foot: MR imaging-pathologic correlation. Radiology. 1997;203:849–855.
- Cremin BJ, Fisher RM. The lesions of congenital syphilis. Br J Radiol. 1970;43:333–341.
- Curtiss PH. Some uncommon forms of osteomyelitis. Clin Orthop. 1973;96:84–87.
- Curtiss PH. The pathophysiology of joint infection. Clin Orthop. 1973;96:129–135.
- D’Amato CR, Pitchon HE. Hematogenous osteomyelitis of the tarsal navicular. J Med Soc N J. 1985;82:644–647.
- Dhillon MS, Nagi ON. Tuberculosis of the foot and ankle. Clin Orthop. 2002;398:107–113.
- Dick VQ, Nelson JD, Hatalin KC. Osteomyelitis in infants and children. Am J Dis Child. 1975;129:1273–1278.
- Dillon DS. Successful treatment of osteomyelitis and soft tissue infections in ischemic diabetic legs by local antibiotic injections and end diastolic pneumatic pressure boot. Ann Surg. 1986;204:643–649.
- Donohoe KJ. Selected topics in orthopedic nuclear medicine. Orthop Clin North Am. 1998;29:85–101.
- Eckman MH, Greenfield S, Mackey WC, et al. Foot infections in diabetic patients. JAMA. 1995;273:712–720.
- Enarson DA, Fuji M, Nakielna EM, et al. Bone and joint tuberculosis. A continuous problem. Can Med Assoc J. 1979;120: 139–145.
- Engh CA, Hughes JL, Abrous RC, et al. Osteomyelitis in the patient with sickle cell disease. Diagnosis and management. J Bone Joint Surg. 1971;53A:1–15.
- Enna CD, Jacobson RR, Rausch RO. Bone changes in leprosy. A correlation of clinical and radiographic features. Radiology. 1971;100:295–306.
- Erdman WA, Tomburro F, Jayson HT, et al. Osteomyelitis. Characteristics and pitfalls of MR imaging. Radiology. 1991;180:533–539.
- Ersoy H, Rybicki FJ. MR angiography of the lower extremities. Am J Roentgenol. 2008;190:1675–1684.
- Feingold ML, Resnick D, Niwayama G, et al. The plantar compartment of the foot. A roentgen approach. Invest Radiol. 1977;12:281–288.
- Feldman F, Auerback R, Johnston A. Tuberculosis dactylitis in the adult. Am J Roentgenol. 1971;112:460–479.
- Fitzgerald RH, Ruttle PE, Arnold PG, et al. Local muscle flaps in treatment of chronic osteomyelitis. J Bone Joint Surg. 1985;67A:175–185.
- Fitzgerald RH, Brewer NS, Dohlin DS. Squamous cell carcinoma complicating chronic osteomyelitis. J Bone Joint Surg. 1976;58A:1146–1148.
- Gilday DL. Problems of scintigraphic detection of osteomyelitis. Radiology. 1980;135:791.
- Gilmour WN. Acute hematogenous osteomyelitis. J Bone Joint Surg. 1962;44B:841–853.
- Gitelis S, Brebach GT. The treatment of chronic osteomyelitis with biodegradable antibiotic-impregnated implant. J Orthop Surg. 2002;10:53–60.
- Gohil VK, Dalinka MK, Edeiken J. The serpiginous tract. A sign of subacute osteomyelitis. J Can Assoc Radiol. 1973;24: 337–339.
- Gold RH, Tong DJF, Crim JR, et al. Imaging of the diabetic foot. Skeletal Radiol. 1995;24:563–571.
- Goodwin DW, Salonen DC, Yu JS, et al. Plantar compartments of the foot. MR appearance in cadavers and diabetic patients. Radiology. 1995;196:623–630.
- Green SA, Ripley MJ. Chronic osteomyelitis in pin tracts. J Bone Joint Surg Am. 1984;66:1092–1098.
- Greene G, Mauer AH, Malmud LS, et al. “Cold spot” imaging with gas gangrene in three phase skeletal scintigraphy. Clin Nucl Med. 1983;8:410–412.
- Greenwood AM. A study of the skin in 500 cases of diabetes mellitus. JAMA. 1927;89:714–781.
- Gross T, Kaim AH, Regazzoni P, et al. Current concepts in posttraumatic osteomyelitis: a diagnostic challenge with new imaging options. J Trauma. 2002;52:1210–1219.
- Guhlmann A, Brecht-Krause D, Suger G, et al. Flourine-18-FDG PET and Technetium-99m antigranulocyte antibody scintigraphy in chronic osteomyelitis. J Nucl Med. 1998;39: 2145–2152.
- Guhlmann A, Brecht-Krause D, Suger G, et al. Chronic osteomyelitis: Detection with FDG PET and correlation with histopathologic findings. Radiology. 1998;206:749–754.
- Gutierrez K. Bone and joint infections in children. Pediatr Clin N Am. 2005;52:779–794.
- Haygood TM, Williamson SL. Radiographic findings of extremity tuberculosis in childhood. Back to the future. RadioGraphics. 1994;14:561–570.
- Horibe S, Tada K, Nagano J. Neuropathy of the foot in leprosy. J Bone Joint Surg. 1988;70B:481–485.
- Horowitz SD, Durham JR, Nease B, et al. Prospective evaluation of magnetic resonance imaging in the management of acute diabetic foot infections. Ann Vasc Surg. 1993;7:44–50.
- Howard JB, McCracken GH Jr. The spectrum of group B streptococcal infections in infancy. Am J Dis Child. 1974; 129:1449–1451.
- Howie DW, Savage JB, Wilson TG. Technetium phosphate bone scan in diagnosis of osteomyelitis in children. J Bone Joint Surg. 1983;65A:431–437.
- Isreal O, Gips S, Jerushalmi J, et al. Osteomyelitis and soft tissue infection. Differential diagnosis with 24 hr/4 hr ratio of Tc-99m MDP uptake. Radiology. 1987;163:725–726.
- Jacobson JA, Andresen R, Jaovisidha S, et al. Detection of ankle effusion. Comparison study in cadavers using radiography, sonography and MR imaging. Am J Roentgenol. 1998;170:1231–1238.
- Jacobson JA, Powell A, Craig JG, et al. Wooden foreign bodies in soft tissue. Detection at US. Radiology. 1998;206:45–48.
- Jaramillo D, Treves ST, Kasser JR, et al. Osteomyelitis and septic arthritis in children: appropriate use of imaging to guide treatment. Am J Roentgenol. 1995;165:399–403.
- Jay PR, Michelson JD, Mizel MS, et al. Efficacy of three-phase bone scans in evaluating diabetic foot ulcers. Foot Ankle Int. 1999;20:347–355.
- Johnson PH. Pseudomonas infection of the foot after puncture wounds. JAMA. 1968;204:262–266.
- Johnson PW, Collins MS, Wenger DE. Diagnostic utility of T1-weighted MRI characteristics in evaluation of osteomyelitis of the foot. Am J Roentgenol. 2009;192:96–100.
- Jones DC, Cady RB. Cold bone scans in acute osteomyelitis. J Bone Joint Surg. 1981;63B:376–378.
- Kaim A, Ledermannn HP, Bongartz G, et al. Chronic post-traumatic osteomyelitis of the lower extremity: comparison of magnetic resonance imaging and combined bone scintigraphy/immunoscintigraphy with radio-labelled monoclonal antigranulocyte antibodies. Skeletal Radiol. 2000;29:378–386.
- Keidar Z, Militianu D, Melamed E, et al. The diabetic foot: initial experience with 18F-FDG PET/CT. J Nucl Med. 2005;46:444–449.
- Kelly PJ. Bacterial arthritis in adults. Orthop Clin North Am. 1975;6:973–982.
- Kelly PJ. Osteomyelitis in the adult. Orthop Clin North Am. 1975;6:983–987.
- Kim EE, Pjara EA, Lowry PA, et al. Osteomyelitis complicating fracture. Pitfalls in 111-In leukocyte scintigraphy. Am J Roentgenol. 1987;148:927–930.
- Kirchenbaum SE, Minenberg ML. Pedal and lower extremity complications of substance abuse. Am J Podiatr. 1982;72: 380–387.
- Klingberg WG. Generalized histoplasmosis in infants and children. J Pediatr. 1950;36:728–741.
- Kumar R, Basu S, Torigian D, et al. Role of modern imaging techniques for diagnosis of infection in the era of 18Fluorine deoxyglucose positron emission tomography. Clin Micro Rev. 2009;21:209–224.
- Larcos G, Brown ML, Sutton RL. Diagnosis of osteomyelitis of the foot in diabetic patients. Value of 111-In leukocyte scintigraphy. Am J Roentgenol. 1991;157:527–531.
- Laughlin TJ, Armstrong DG, Caporusso J, et al. Soft tissue and bone infections from puncture wounds in children. West J Med. 1997;166:126–128.
- Lavery LA, Harkless LB, Ashry HR, et al. Infected puncture wounds in adults with diabetes. Risk factors for osteomyelitis. J Foot Ankle Surg. 1994;33:561–566.
- Lavery LA, Walker SC, Hackless LB, et al. Infected puncture wounds in diabetic and non-diabetic adults. Diabetes Care. 1995;18:1588–1591.
- Ledermann HP, Morrison WB, Schweitzer ME. MR image analysis of pedal osteomyelitis: distribution, patterns of spread and frequency of associated ulceration and septic arthritis. Radiology. 2002;223:747–755.
- Ledermann HP, Morrison WB, Schweitzer ME, et al. Tendon involvement in pedal infection: MR analysis of frequency, distribution and spread of infection. Am J Roentgenol. 2002;179:939–947.
- Lipsky BA, Pecosaro RE, Wheat LJ. The diabetic foot. Soft tissue and bone infection. Infect Dis Clin North Am. 1990;4:409–432.
- Lipsky BA. New developments in diagnosing and treating diabetic foot ulcers. Diabetes/Metab Res Rev. 2008; 24(suppl):S66–S71.
- Lisbona R, Rosenthal L. Radionuclide imaging of septic joints and their differentiation from periarticular osteomyelitis and cellulitis in pediatrics. Clin Nucl Med. 1997;2:337–343.
- Littenberg B, Mushlin AL. Technetium bone scanning in the diagnosis of osteomyelitis: a meta-analysis of test performance. J Gen Intern Med. 1992;7:158–164.
- Littman MC. Cryptococcosis (torulosis). Am J Med. 1959; 27:976–999.
- Love C, Palestro CJ. Radionuclide imaging of infection. J Nucl Med Tech. 2004;32:47–57.
- Magnuson JE, Brown ML, Hauser MF, et al. Indium-111 white blood cell scintigraphy versus other imaging tests in suspected orthopedic prosthesis infection. A comparison. Radiology. 1988;168:235–239.
- Marcus CD, Ladam-Marcus VJ, Leone J, et al. MR imaging of osteomyelitis and neuropathic osteoarthropathy in the feet of diabetics. RadioGraphics. 1996;16:1337–1348.
- Mauer AH, Chen DCP, Camargo EE. Utility of three phase skeletal scintigraphy in suspected osteomyelitis. J Nucl Med. 1981;22:941–949.
- Mauer AH, Millmond SH, Knight LC, et al. Infection in diabetic osteoarthropathy. Use of Indium-labeled leukocytes for diagnosis. Radiology. 1986;161:221–225.
- Mazua JM, Ross G, Cummings RJ. Usefulness of magnetic resonance imaging for diagnosis of acute musculoskeletal infections in children. J Pediatr Orthop. 1995;15:144–147.
- Meinen IA, Jacobs NM, Yeh TF, Libern LD. Group B streptococcal osteomyelitis and septic arthritis. Am J Dis Child. 1979;133:291–296.
- Merkel KD, Brown ML, Dewanjee MR, et al. Comparison of indium labeled leukocyte imaging with sequential technetium-gallium scanning in diagnosis of low grade musculoskeletal sepsis. A prospective study. J Bone Joint Surg. 1985;67A:465–476.
- Merkel KD, Fitzgerald RH, Brown ML. Scintigraphic evaluation of musculoskeletal sepsis. Orthop Clin North Am. 1984;15:401–416.
- Miller EH, Semian DW. Gram negative osteomyelitis following puncture wounds of the foot. J Bone Joint Surg. 1975;57A:535–537.
- Miller TT, Randolph DA Jr, Staron RB, et al. Fat-suppressed MRI of musculoskeletal infection. Fast T2-weighted techniques versus gadolinium enhanced T1-weighted images. Skeletal Radiol. 1997;26:654–658.
- Miller WB, Murphy WA, Gilula LA. Brodie’s abscess. Reappraisal. Radiology. 1979;132:15–23.
- Miron D, Raz R, Kaufman B, et al. Infections following nail puncture wounds of the foot. Case reports and review of the literature. Isr J Med Sci. 1993;29:194–197.
- Mollan RA, Piggot J. Acute osteomyelitis in children. J Bone Joint Surg. 1977;59B:2–7.
- Moore TE, Yuh WTC, Kathol MH, et al. Abnormalities of the foot on patients with diabetes mellitus. Findings on MR imaging. Am J Roentgenol. 1991;157:813–816.
- Morrey BF, Bianco AJ, Rhodes KA. Hematogenous osteomyelitis in uncommon sites in children. Mayo Clin Proc. 1978;53:707–713.
- Morrison WB, Schweitzer ME, Ganville-Batte W, et al. Osteomyelitis of the foot. Relative importance of primary and secondary MR imaging signs. Radiology. 1998;207:625–632.
- Morrison WB, Schweitzer ME, Wapner KL, et al. Osteomyelitis in feet of diabetics. Clinical accuracy, surgical utility and cost effectiveness of MR imaging. Radiology. 1995;196:557–564.
- Murray IPC. Photopenia in skeletal scintigraphy of suspected bone and joint infection. Clin. Nucl Med. 1982;7:13–20.
- Mushlin AI, Littenberg B. Diagnosing pedal osteomyelitis. Testing choices and their consequences. J Gen Intern Med. 1994;9:1–7.
- Nazarian LN, Rowool NM, Martin CE, et al. Synovial fluid in the hind foot and ankle. Detection of amount and distribution with US. Radiology. 1995;197:275–278.
- Nguyen VD, London J, Cone RO III. Ring sequestrum. Radiographic characteristics of skeletal fixation pin tract osteomyelitis. Radiology. 1986;158:129–131.
- Nixon GW. Hematogenous osteomyelitis of metaphyseal equivalent locations. Am J Roentgenol. 1978;130:123–129.
- O’Connor B, Steel WM, Saunders R. Disseminated bone tuberculosis. J Bone Joint Surg. 1970;52A:537–542.
- Ogden JA, Light TR. Pediatric osteomyelitis. Arizona hinshavii osteomyelitis. Clin Orthop. 1979;139:110–113.
- O’Mara RE, Wilson GA, Burke AM. Skeletal imaging in osteomyelitis. J Nucl Med. 1982;24:71.
- Palestro CJ, Love C, Tronco GG, et al. Role of radionuclide imaging in diagnosis of postoperative infection. RadioGraphics. 2000;20:1649–1660.
- Paterson DC. Acute suppurative arthritis in infancy and childhood. J Bone Joint Surg. 1970;52B:474–482.
- Peh WCG, Brockwell J, Chau MT, et al. Imaging features of dissecting neuropathic joints. Aust Radiol. 1995;39:249–253.
- Peterson JJ, Bancroft LW, Kransdorf MJ. Wooden foreign bodies: imaging appearance. Am J Roentgenol. 2002;178: 557–562.
- Pritchard DJ. Granulomatous infections of bones and joints. Orthop Clin North Am. 1975;6:1029–1047.
- Rafii M, Firooznia H, Galimbu C, et al. Hematogenous osteomyelitis with fat-fluid level shown by CT. Radiology. 1984;153:493–494.
- Rahmouni A, Chosedow O, Mathieu D, et al. MR imaging of acute infectious cellulitis. Radiology. 1994;192:493–496.
- Raptopoulos V, Doherty PW, Gross TP. Acute osteomyelitis. Advantage of white cell scans for early detection. Am J Roentgenol. 1982;139:1077–1082.
- Resnick D. Pyarthrosis complicating rheumatoid arthritis. Roentgenographic evaluation of 5 patients and a review of the literature. Radiology. 1975;114:581–586.
- Resnick D, Kransdorf MJ. Bone and Joint Imaging. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2005.
- Reynolds FW, Wasserman H. Destructive osseous lesions in early syphilis. Arch Intern Med. 1942;69:263–276.
- Rhangos WC, Check EW. Mycotic infections in bone. South Med J. 1964;57:664–674.
- Rosenthall L, Lisbona R, Hernandez M. 99mTc-PP and 67Gallium citrate imaging following insertion of orthopedic appliances. Radiology. 1979;133:717–721.
- Rudolph AJ, Singleton EB, Rosenberg HS, et al. Osseous manifestations of congenital rubella syndrome. Am J Dis Child. 1965;110:428–433.
- Sarto LA. The infected implant. Clin Podiatr. 1984;1:199–209.
- Sartoris DJ, Devine S, Resnick D, et al. Plantar compartmental infection in the diabetic foot. The role of computed tomography. Invest Radiol. 1985;20:772–784.
- Schauwecker DS. The scinitygraphic diagnosis of osteomyelitis. Am J Roentgenol. 1992;158:9–18.
- Schiesser M, Stumpe KDM, Trentz O, et al. Detection of metallic implant associated infections with FDG PET in patients with trauma: correlation with microbiological results. Radiology. 2003;226:391–398.
- Schiller M, Donnelly PJ, Melo JC, et al. Clostridium perfringens septic arthritis. Clin Orthop. 1979;139:92–95.
- Schmid MR, Kossmann T, Duewell S. Differentiation of necrotizing fasciitis and cellulitis using MR imaging. Am J Roentgenol. 1998;170:615–620.
- Schweitzer ME, Daffner RH, Weissman BN, et al. ACR appropriateness criteria on suspected osteomyelitis in patients with diabetes mellitus. J Am Coll Radiol. 2008;5:881–886.
- Scoles PV, Hilty MD, Sfakianadeis GN. Bone scan patterns in acute osteomyelitis. Clin Orthop. 1980;153:210–217.
- Seldin DW, Heiken JP, Feldman F, Alderson PO. Effect of soft tissue pathology on detection of pedal osteomyelitis. J Nucl Med. 1985;26:988–993.
- Sfakianakis G, Al-sherkh W, Spolecinsky E. Correlation of In-111–WBC, gallium-67 scintigraphy, computed tomography, ultrasonography and plain radiography in diagnosis of focal infection. J Nucl Med. 1983;24:P38.
- Shapiro SE, Spurling DC, Cavaliere R. Infections following implant arthroplasties of the forefoot. Clin Podiatr Med Surg. 1996;13:767–791.
- Shukla PC. Plantar cellulitis. Pediatr Emerg Care. 1994;10: 23–25.
- Sofka CM, Adler RS. Ultrasound-guided interventions in the foot and ankle. Semin Musculoskeletal Radiol. 2002;6:163–168.
- Specht EE. Hemoglobinopathies with salmonella osteomyelitis: orthopedic aspects. Clin Orthop. 1971;79:110–118.
- Steed DL, Donohoe D, Webster MW, et al. Effect of extensive debridement and treatment of healing diabetic foot ulcers. diabetic Ulcer Study Group. J Am Coll Surg. 1996;183:61–64.
- Sugarman B, Hawes S, Musher DM, et al. Osteomyelitis beneath pressure sores. Arch Intern Med. 1983;143:683–688.
- Termaat MF, Jaijmakers PGHM, Scholten HJ, et al. The accuracy of diagnostic imaging for the assessment of chronic osteomyelitis: a systematic review and meta-analysis. J Bone Joint Surg. 2005;87A:2464–2471.
- Toohey JS. Pseudomonas osteomyelitis following puncture wounds of the foot. Kans Med. 1993;94:325–326.
- Trueta J. Three types of acute hematogenous osteomyelitis. A clinical and vascular study. J Bone Joint Surg. 1959; 41B:671–680.
- Varnell RM, Flint DW, Dalley KW, et al. Myocutaneous flap failure. Early detection with Gd-DTPA-enhanced MR imaging. Radiology. 1989;173:755–758.
- Vartanians VM, Karchmer AW, Giurini JM, et al. Is there a role for imaging in the management of patients with diabetic foot? Skeletal Radiol. 2009;38:633–636.
- Waldvogel FA, Medoff G, Schwartz MN. Osteomyelitis. A review of the clinical features, therapeutic conditions, and unusual aspects. N Engl J Med. 1978;282:198–206.
- Waldvogel FA, Popageogion PS. Osteomyelitis. The past decade. N Engl J Med. 1980;303:306–370.
- Weber EJ. Plantar puncture wounds. A survey to determine the incidence of infection. J. Accid Emerg Med. 1996;13: 274–277.
- Whitehouse WM, Smith WS. Osteomyelitis in the feet. Semin Roentgenol. 1970;5:367–377.
- Wing VW, Jeffrey RB, Federle MP, et al. Chronic osteomyelitis examined by CT. Radiology. 1985; 154:171–174.
- Wood MB, Cooney WP III. Vascularized bone segment transfers for management of chronic osteomyelitis. Orthop Clin North Am. 1984;15:401–472.
- Wysoki MG, Santora TA, Shah RM, et al. Necrotizing fasciitis: CT characteristics. Radiology. 1997;203:859–863.
- Yuh WTC, Sato Y, El-Khoury GY, et al. Osteomyelitis of the foot in diabetics: evaluation with plain film, 99mTc-MDP bone scintigraphy and MR imaging. Am J Roentgenol. 1989;152:795–800.
- Zlatkin MB, Pathria M, Sartoris DJ, et al. The diabetic foot. Radiol Clin North Am. 1987;25:1095–1105.
CHAPTER 8
Bone and Soft Tissue Ischemia
Thomas H. Berquist and Anthony B. Adelson
- Introduction
- Osteonecrosis
- Etiology of Ischemic Necrosis in Bone
- Histologic and Imaging Features of Bone Necrosis
- Specific Sites and Problems in the Foot and Ankle
- Treatment
- Complications of Osteonecrosis
- Etiology of Ischemic Necrosis in Bone
- Soft Tissue Ischemia
- Vasoplastic Disorders
- Erythromelalgia
- Arterial Occlusive Diseases
- Diagnostic Techniques
- Treatment
- Vasospastic Diseases
- Vasoplastic Disorders
- References
INTRODUCTION
Ischemic necrosis is a common problem in the foot, particularly in diabetic patients and patients with other vascular diseases. Necrosis of bone and that of soft tissues are considered separately because their underlying causes, imaging evaluation, and management differ considerably.
OSTEONECROSIS
The terms applied to ischemic bone disease can be confusing. Osteonecrosis is used to describe death of bone and marrow cell components [186]. Although originally (in the 19th century) the cause was considered to be infectious, no organisms could be cultured. The lack of evidence for infection coupled with the loss of blood supply as identified histologically led to the terms ischemic necrosis and aseptic necrosis to describe this condition [22,97,186,197]. Today, two distinct terms are applied to osteonecrosis based on the area of bone involved. Avascular necrosis is the term applied to ischemic necrosis involving the epiphyseal region. Osteonecrosis in the diaphysometaphyseal portion of bone is termed a bone infarct [186].
Osteochondrosis is a loosely used term that generally applies to ischemic disease in the apophysis of the immature skeleton. Osteochondritis and apophysitis or epiphysitis are also frequently used interchangeably to describe clinical symptoms involving these sites in children [186,187]. Certain of these conditions are most likely ischemic, whereas others simply represent normal variations in ossification [29,172,186].
For purposes of this section, the pathogenesis of osteonecrosis and its associated radiographic features are reviewed. Other common conditions in the foot and ankle considered in the “osteochondroses” category are also discussed.
Etiology of Ischemic Necrosis in Bone
The etiology of osteonecrosis is not always clear (Table 8-1). However, several mechanisms are implicated in reduced blood flow. Vascular supply to a region may be reduced by traumatic disruption of the blood supply, vascular occlusion (thrombosis or sludging), vascular compression, or prolonged vasospasm [26,103,133,186]. The type of vessels involved and the anatomic site (epiphysis, metaphysis, or diaphysis) are important. Arterial collateral vessels serve a protective function, whereas sinusoids are more susceptible to occlusion, especially in patients with sickle cell disease or other hemoglobinopathies. The epiphyses have fewer collateral vessels, especially before growth plate closure. The surface area of articular cartilage is a significant factor in the tarsal bones because this reduces the available penetration area for vessels. The talus, for example, has an extensive articular surface reducing entrance points for blood supply resulting in increased susceptibility to osteonecrosis [174,176]. The articular cartilage receives much of its nutrients from synovial fluid, a feature that excludes this area from the ischemic process [34,90,186].
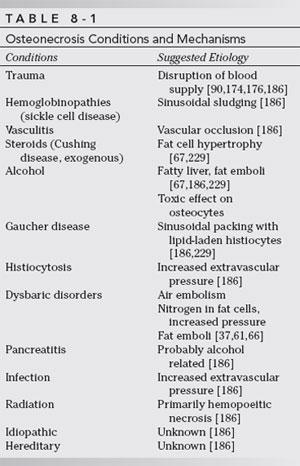
Certain clinical conditions and mechanisms are well accepted as causes of osteonecrosis (see Table 8-1). Traumatic transsection of vessels and intraluminal thrombosis are well documented. In certain situations, the pathogenesis is more controversial. Dysbaric osteonecrosis has increased because of space exploration, expansion of offshore oil exploration, and deep-sea exploration. Osteonecrosis occurs because of rapid changes in pressure resulting in release of gases, primarily nitrogen (nitrogen narcosis) into the blood and soft tissues. Microgas emboli result in ischemic changes in the affected area, including bone. Nitrogen appears to have a propensity for accumulation in fat and marrow. Thus, vascular insult may be direct (gas emboli) or indirect (accumulation in fat cells). Disruption of fat cells with associated fat emboli has also been implicated [37,61,66]. The incidence of dysbaric osteonecrosis is higher in obese patients, in patients with repeated exposures to pressure changes, and in patients with rapid, high-pressure exposures. The incidence of dysbaric osteonecrosis in deep-sea divers maybe approaches 10% to 20% [41]. The most common sites of necrosis are the humerus and femur. Foot and ankle involvement is rare [37,41,61,66,176].
Marrow cell packing and other extravascular diseases (see Table 8-1) increase pressure in the marrow compartment causing extrinsic vascular compromise. These conditions affect the femoral head much more frequently than the bones of the foot and ankle [47,50,67,186,229].
Cushing disease and iatrogenic steroid administration are commonly associated with avascular necrosis. The exact cause is unclear. However, fat cell hypertrophy and fatty liver with fat embolization (see Table 8-1) have been implicated [67,186,229]. Steroid-induced osteonecrosis is most common in the hips, shoulders, and knees. The foot and ankle are involved less frequently.
Certain diseases affect the vessel walls, leading to ischemic changes. These conditions include lupus erythematosus, arteriosclerosis, and rheumatoid arthritis [50,176,187]. Resnick et al. [187] reported widespread osteonecrosis of the foot in systemic lupus erythematosus. Soft tissue ischemia is more common in the foot and ankle in patients with arteriosclerosis and other vascular diseases. Other potential causes and mechanisms of osteonecrosis are summarized in Table 8-1.
Histologic and Imaging Features of Bone Necrosis
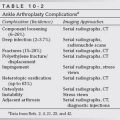
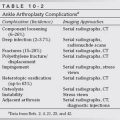
A predictable histologic response occurs regardless of the underlying cause of bone necrosis. The stages are progressive, but overlap is considerable, so a clear definition between each phase may not be distinguishable. Most data, including that presented later, are based on histologic studies of the hip (Table 8-2); however, similar changes occur in other areas of the skeleton. Image features vary with location, stage of necrosis, and the imaging modality applied [22,26,53,100].
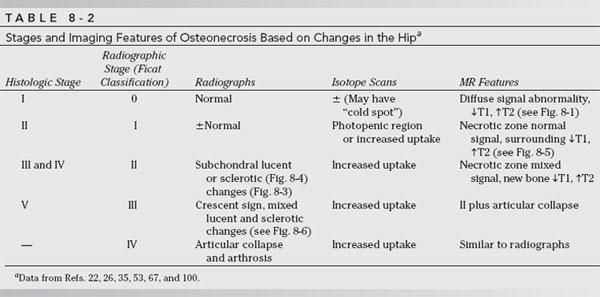
Stage I
Cell death occurs in stages, beginning with alterations in cellular enzyme systems [26,103,186]. If ischemic changes persist, the enzymatic abnormalities lead to cessation of metabolic processes resulting in cell necrosis. These effects occur at different times depending on the cell type. Hematopoietic cells undergo necrotic change 6 to 12 hours after blood supply is interrupted. Necrosis takes 12 to 48 hours to develop in osteocytes, osteoblasts, and osteoclasts and 2 to 5 days in fat cells [103,186,229].
Histologic changes of cell necrosis are not evident for 48 to 72 hours using conventional light microscopy. Therefore, it is not surprising that radiographs are entirely normal during the earliest phases of osteonecrosis (see Table 8-2) [22,67,100]. Radionuclide scans may be positive early. Both increased uptake of radiotracer and photopenic regions (“cold spots”) have been described with avascular necrosis [22,53,81,82]. Magnetic resonance imaging has become the technique of choice for detection of early bone necrosis and to differentiate avascular necrosis from other causes of bone or joint pain [24,103,186]. Theoretically, MR imaging can detect abnormalities as early as 2 to 5 days after insult resulting from fat necrosis and edema [16]. Imaging changes are primarily due to inflammatory or hyperemic changes that lead to decreased signal on T1-weighted images and increased signal on T2-weighted or STIR images (Fig. 8-1) [22,191].