PART VIII Pediatrie Vascular Interventions
CASE 56
Case Description
Clinical Presentation
A 5-month-old boy has a history of cardiac failure since birth, which has been controlled sufficiently with diuretics, and he is feeding well orally. MRI is performed. His psychomotor development is normal on follow-up visits, and he is now scheduled for angiography and embolization. His physical and neurologic examination findings at admission are normal.
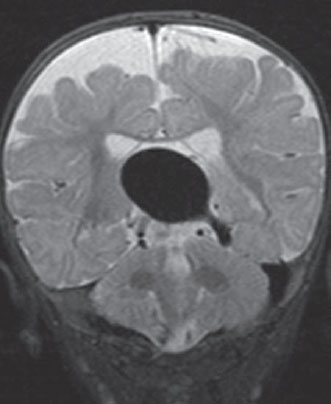
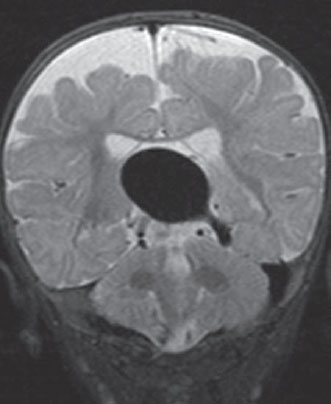
Fig. 56.1 Coronal T2-weighted MRI reveals a midline dilated vascular structure at the vein of Galen region.
Radiologie Studies
MRI
The MRI study showed a midline dilated flow void at the vein of Galen region, representing a vascular structure. The brain parenchymal signal appeared normal. A slightly low-lying position of the cerebellar tonsils was observed (Fig. 56.1). Normal myelination was perceived, no abnormal diffusion-weighted changes were seen, and there were no signs of calcifications or brain atrophy.
DSA
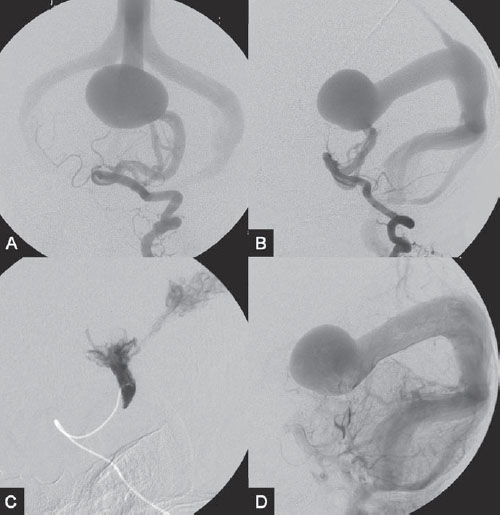
Because there is no role for diagnostic angiography without embolization, DSA was performed immediately before embolization. DSA revealed a high-flow arteriovenous shunt fed from a left posterior choroidal artery branch and draining into the dilated median vein of the prosencephalon (the forerunner of the vein of Galen; Fig. 56.2 A,B). There were additional collaterals from smaller medial posterior choroidal branches. A falcine sinus was present, with absence of the straight sinus. Medial occipital and marginal sinuses were also observed. The posterior fossa veins were poorly visualized, suggestive of venous congestion at the level of the posterior fossa structures (which also explained the slightly low-lying tonsils). Internal carotid artery (ICA) injections showed drainage of the cerebral hemispheres through the cavernous sinuses bilaterally (cavernous capture).
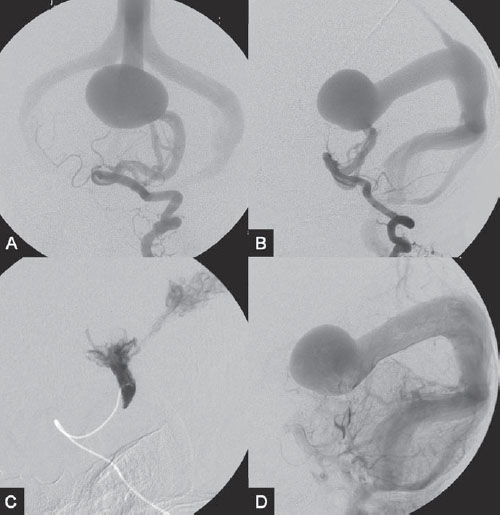
Fig. 56.2 DSA. Left VA angiogram in (A) AP and (B) lateral views. (C) DSA after embolization demonstrates a “mushroom” configuration of the glue cast with minimal penetration into the proximal venous pouch. (D) On left VA angiogram in lateral view after embolization, improved visualization of the posterior fossa veins suggests regression of venous congestion.
Diagnosis
Mural type of vein of Galen aneurysmal malformation Treatment
Treatment
EQUIPMENT
- Standard 4F access (puncture needle, 4F vascular sheath)
- Standard 4F multipurpose catheter (Cook Medical, Bloomington, IN) with continuous slow drip and a 0.035-in hydrophilic guidewire (Terumo, Somerset, NJ)
- A 0.018-in flow-directed microcatheter (BALTACCI; Balt International, Montmorency, France) with a steam-shaped 90-degree curve
- A 10% glucose solution
- Histoacryl/Lipiodol/tantalum powder (2 mL/0.1 mL/1 vial)
- Contrast material (maximum number of milliliters, 4 × body weight in kilograms)
DESCRIPTION
Following diagnostic angiography (one vessel, 6 mL of contrast), a 4F multipurpose catheter was advanced into the left vertebral artery (VA), with the tip placed at the C3-4 level. A flow-related microcatheter was introduced into the left posterior choroidal branch originating from the left posterior cerebral artery (PCA). The tip was placed against the wall of the arterial feeder with a 1-cm margin to the shunt zone. A control run was done via hand injection through the microcatheter (2 mL) to verify the position. The microcatheter was then flushed with glucose solution, followed by the rapid injection of pure glue to close the fistula and obtain a “mushroom” configuration of the glue cast with only minimal venous penetration. The microcatheter was removed, and a control angio-gram performed via the guiding catheter revealed obliteration of the posterior choroidal feeder and significantly reduced flow through the shunt. Visualization of the posterior fossa veins was improved, indicating improvement of the posterior fossa venous drainage (Fig. 56.2 C,D). The child had no new neurologic deficits following embolization. He is to be followed with psychomotor neuropediatric assessments every 3 months (including head circumference measurements) and MRI every 6 months. The next embolization session, if no psychomotor retardation occurs, is planned for 1 year after the first embolization.
Discussion
Background
Vein of Galen aneurysmal malformations are arteriovenous malformations of the choroidal system that develop in the early embryonic stage. They account for ~30% of all vascular malformations in the pediatric population. Cardiac failure, the most common presentation in neonates, may progress to multiple-organ failure if left untreated and is probably related to the lower cardiovascular volume of these patients. A clinical presentation with hydrodynamic disorders, such as hydrocephalus and macrocrania, is more commonly seen in older infants. Only rarely is this disorder diagnosed in older children, who are more likely to present with neurologic symptoms such as seizures, neurologic deficits, and even intracranial hemorrhage. These cases are associated with a poor outcome, which is likely related to the degree of brain damage caused by the vein of Galen aneurysmal malformation. Certain angioarchitectural characteristics are specific for vein of Galen aneurysmal malformations. The arterial supply always involves the choroidal arteries, including the anterior choroidal artery, posterior choroidal artery, and subforniceal artery (anterior cerebral artery [ACA] branch). The subependymal arteries and limbic arterial arch (between the PCA and ACA branches) constitute the remainder of the supply. Secondary supply from transcerebral branches of the middle cerebral artery (MCA) typically represents sump effect and arterial steal. Two types of nidi are seen in vein of Galen aneurysmal malformations: a mural type, consisting of direct arteriovenous fistulae within the wall of the median vein of the prosencephalon, and a choroidal type, which corresponds to a more primitive condition. In the choroidal type, a network is interposed between the nidus and the opening into the large venous pouch. Venous drainage is toward the dilated median vein of the prosencephalon, which is the forerunner of the vein of Galen. Although it has been previously reported that no communication between this vein and the deep venous system exists, many case reports have actually documented a connection, typically at the posterior aspect of the dilated venous segment. Several embryonic sinuses often persist in vein of Galen aneurysmal malformations, including a falcine sinus, which may occur with absence of the straight sinus and of the medial occipital and marginal sinuses.
Noninvasive Imaging Workup
CLINICAL EXAMINATION
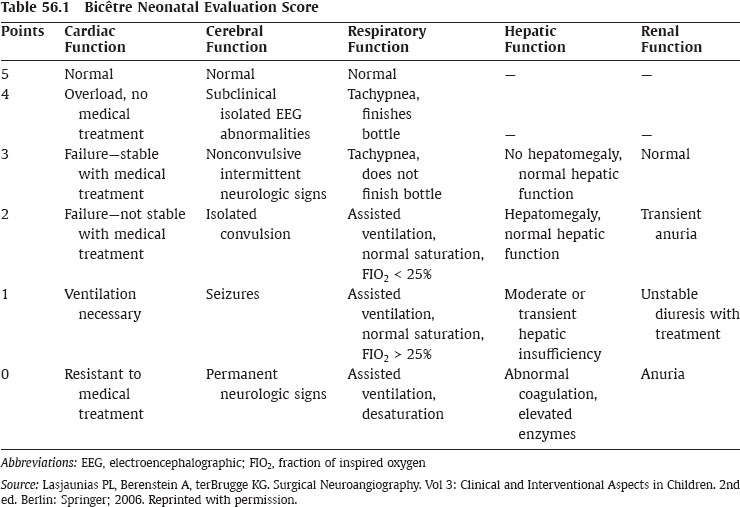
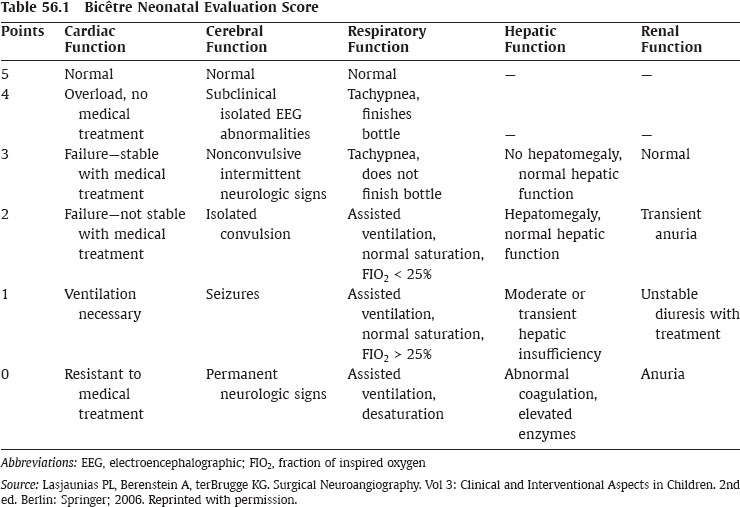
- The Bicétre score is used in most centers to evaluate children in whom a vein of Galen malformation is diagnosed (Table 56.1). In this system, cardiac, cerebral, respiratory, hepatic, and renal function is evaluated and scored accordingly.
- The following strategy is adopted after scoring: Patients whose score is higher than 12 receive medical treatment (see below) until the age of 4 to 5 months or until a complication occurs; patients whose score is 8 to 11 receive emergency embolization; a score below 8 is an indication for therapeutic abstention. Emergency embolization is also considered if a child has medically refractory heart failure, exhibits an increase in the cranial perimeter, or is not feeding well (no weight gain).
- The Denver scoring system may be employed to evaluate whether developmental milestones have been reached.
- The ocular fundus may be investigated to assess venous congestion.
- Bluish discoloration of the skin is generally a good sign because it means that the brain has “captured” the cavernous sinuses for drainage.
PRENATAL ULTRASOUND
- A dilated median vein of the prosencephalon is seen as an anechoic tubular midline structure located superior to the cerebellum. Increased flow on color Doppler images helps to confirm the diagnosis.
- Prenatal ultrasound is most sensitive for the detection of vein of Galen aneurysmal malformations after the 26th week of gestation.
CT/MRI
- MRI is the best imaging modality for the evaluation of vein of Galen aneurysmal malformations and can also be done prenatally to assess the brain parenchyma.
- A dilated midline venous pouch, representing a dilated median vein of the prosencephalon, can be seen on CT scan and as a flow-void structure on MRI.
- Parenchymal changes are best seen on FLAIR images and T2-weighted MR sequences and can be classified as focal encephalomalacia or diffuse loss of brain volume.
- Focal encephalomalacia is more likely related to the presence of arterial steal, which is a result of the high-flow sump effect of the vein of Galen aneurysmal malformation. It is characterized by leptomeningeal collateralization of the cortical branches of the MCA or the ACA to the PCA territories, further contributing to the arteriovenous shunt of the vein of Galen aneurysmal malformation, and is best seen on contrast-enhanced CT or as flow-void structures on T2-weighted MRI.
- Diffuse loss of brain volume is usually associated with hydrocephalus and may be reversible following treatment.
- Hydrodynamic disorders caused by vein of Galen aneurysmal malformations include macrocrania, hydrocephalus, and venous congestion.
- Acute venous congestion can result in brain edema, seen as hypodensity on CT or T2 hyperintensity on MRI, and in tonsillar prolapse infratentorially. Chronic venous congestion usually results in parenchymal calcifications, which are better seen on unenhanced CT than on gradient-echo MRI.
- Diffusion-weighted abnormalities tend to indicate a poor prognosis, and therapeutic abstention may be chosen if the diffusion-weighted imaging changes are rapidly progressive.
CTA/MRA
- Early filling of the dilated median vein of the prosencephalon with enlargement of the arterial feeders can be seen on both CTA and MRA. These techniques are able to determine whether a mural or choroidal type of shunt is present.
- CTV and MRV may be helpful in the evaluation of the venous outflow restrictions, usually caused by dysmaturation or stenosis of the jugular bulb, and to evaluate whether cavernous capture has taken place (bulging of the cavernous sinuses).
Invasive Imaging Workup
- Angiography is the gold standard for the detailed evaluation of the angioarchitecture of a vein of Galen aneurysmal malformation and must be done within the same session as the endovascular treatment to avoid multiple punctures to the femoral arteries.
- In neonates, the restricted amount of contrast (maximum, 4 mL/kg) is a major limitation for a complete study.
- One VA and one ICA are evaluated to identify the major feeder and determine how the normal brain drains.
Treatment Options
CONSERVATIVE OR MEDICAL MANAGEMENT
- The therapeutic strategy is to ensure normal development; therefore, the cardiac overload and venous congestion must be reduced, and oral feeding has to be ensured.
- The initial management of a neonate with a vein of Galen aneurysmal malformation and congestive heart failure consists of medical stabilization of the heart failure, typically with digoxin (increase inotropy), diuretics (decrease preload), dopamine (increase cardiac output), mechanical ventilation (less oxygen needed), or inhaled nitric oxide. These therapies are aimed at allowing the baby to feed orally so that he or she gains weight. If medical therapies fail, endovascular therapies are indicated.
- The best position for the baby is a 20- or 30-degree head-up position in the bed to optimize venous drainage without kinking of the jugular veins.
SURGICAL TREATMENT
- Surgical removal of the lesion is no longer advised because of the hemodynamic instability of these patients and the deep location of the lesion, which result in a high mortality rate.
- Ventricular shunting should be avoided because it does not treat the hydrovenous disorder responsible for the ventricular enlargement. In fact, ventricular shunting frequently worsens the size of a vein of Galen aneurysmal malformation and leads to subcortical calcifications.
- Surgery is reserved for the evacuation of intracranial hematomas in rare cases that bleed and the treatment of severe hydrocephalus that does not decrease after embolization.
ENDOVASCULAR TREATMENT
- Transarterial embolization is the treatment of choice for vein of Galen aneurysmal malformations, and the optimal timing of embolization is at 4 to 5 months of age; this waiting period is not long enough for permanent brain damage to develop yet offers enough benefit concerning arterial access and contrast limitation problems. More urgent treatment may be considered for patients with a Bicétreneonatal score of 8 to 11, deteriorating or severe congestive heart failure, evidence of arterial steal, and/or progressive occlusion of the venous outflow without permanent brain damage on MRI or CT.
- A femoral arterial access is routinely used in our practice; however, in a newborn up to 3 days of age, an umbilical artery access may be used.
- In the authors’ experience, pure glue (2 mL of Histoacryl/0.1 mL of Lipiodol with tantalum powder) is the preferred embolic material for high-flow, muraltype fistulae. The microcatheter is placed against the wall of the feeding artery, and the pure glue is rapidly injected to produce a “mushroom” appearance of the glue cast, which minimally penetrates the proximal venous pouch. A more diluted concentration of glue or other liquid embolic materials, such as Onyx, may be considered with the choroidal type of nidi but tend to be associated with prolonged injection times and radiation exposure, which is a strong concern in pediatric patients.
- Multiple arterial feeders are often encountered; the largest are usually embolized first to allow normal cardiac and neurologic development. Multiple sessions may be required to achieve the desired clinical effect. The goal of the treatment is a child who can develop normally rather than an impaired child who is cured. Progressive thrombosis of a vein of Galen aneurysmal malformation is not infrequent, even after partial treatment with some glue penetration into the venous pouch.
- A transvenous route may also be used but carries a higher risk for complications, including venous perforation and occlusion of the deep venous drainage with fatal brain hemorrhage. It has also proved to be much less efficient than transarterial glue embolization in reversing high-output cardiac failure.
Possible Complications
- Puncture site complications with thrombosis or dissection of the artery and, in the worst case scenario, loss of the lower limb
- Pulmonary emboli
- Migration of the embolic agent into the posterior aspect of the dilated venous pouch, causing occlusion of the deep venous drainage with subsequent venous infarctions/hemorrhage
- Perforation of the arterial feeders
- Re flux of the glue into normal arteries, resulting in ischemic stroke
Published Literature on Treatment Options
Before the advent of embolization, patients with vein of Galen aneurysmal malformations had a dismal prognosis. In the early surgical series, the mortality rate was 99 to 100%. Outcomes improved with advances in endovascular embolization techniques and neonatal care, which led to a 0 to 50% mortality rate (with a 28–68% overall poor outcome). Although the outcome of patients has been improving over the years, the overall outcome was still considered poor in up to 50% of patients in the larger series published by Lasjaunias et al. Approximately 10 to 20% of patients with vein of Galen aneurysmal malformations were considered to be in too poor condition to be treated or expired before treatment. In the largest series reported so far by Lasjaunias et al, in 2006, ~60% of the 233 patients who were treated with endovascular embolization had a good outcome. In their total cohort of 317 patients, spontaneous thrombosis of the shunt occurred in 2.5% (8/317). In a recent series of the Toronto experience by Geibprasert et al, 47% of the patients treated had a good outcome, and 5 of 6 patients in a subgroup of carefully selected patients had a good outcome with conservative management and close follow-up. The criteria for the selection of these patients were as follows: (1) a high neonatal score (> 17); (2) clinical symptoms of only mild congestive heart failure well controlled with medication and no neurologic symptoms; (3) imaging findings indicating no parenchymal loss, calcifications, hydrocephalus, tonsillar herniation, or evidence of arterial steal; and (4) angioarchitectural findings of low-flow shunts (i.e., two or fewer enlarged arterial feeder groups, lack of deep venous drainage, lack of jugular bulb stenosis). The management of patients with a vein of Galen aneurysmal malformation remains challenging and should be based on an assessment of the individual patient and the operator’s personal experience.
PEARLS AND PITFALLS__________________________________________________
- Vein of Galen aneurysmal malformations are choroidal arteriovenous malformations that develop during the early embryonic stage and drain into the median vein of the prosencephalon, which is the precursor of the vein of Galen.
- Factors associated with a poor outcome are the following: neurologic symptoms at presentation, a Bicétre neonatal score of less than 12 of 21, a very poor score of less than 2 of 5 in one (or more) categories, focal parenchymal changes, calcifications, tonsillar herniation, arterial steal, and multiple arterial feeders.
- The management decision is challenging and must be made on an individual basis. The optimal treatment time is at 4 to 5 months of age; however, urgent treatment should be considered for those who have deteriorating congestive heart failure or evidence of arterial steal or progressive occlusion of the venous outflow without evidence of permanent brain damage on CT or MRI.
Further Reading
Alvarez H, Garcia Monaco R, Rodesch G, Sachet M, Krings T, Lasjaunias P. Vein of Galen aneurysmal malformations. Neuroimaging Clin N Am 2007;17(2):189–206
Geibprasert S, Krings T, Armstrong D, Terbrugge KG, Raybaud CA. Predicting factors for the follow-up outcome and management decisions in vein of Galen aneurysmal malformations. Childs Nerv Syst 2010;26(1):35–46
Lasjaunias PL, Berenstein A, terBrugge KG. Surgical Neuroangiography. Vol 3: Clinical and Interventional Aspects in Children. 2nd ed. New York, NY: Springer; 2006
Lasjaunias PL, Chng SM, Sachet M, Alvarez H, Rodesch G, Garcia-Monaco R. The management of vein of Galen aneurysmal malformations. Neurosurgery 2006;59(5 Suppl 3):S184–S194, discussion S3–S13
CASE 57
Case Description
Clinical Presentation
A 7-year-old previously healthy boy has had significant headaches over the past 2 weeks. His parents confirm that he has never had any headaches before. Outside CT has demonstrated dilated vessels, and he is referred to our institution for further workup.
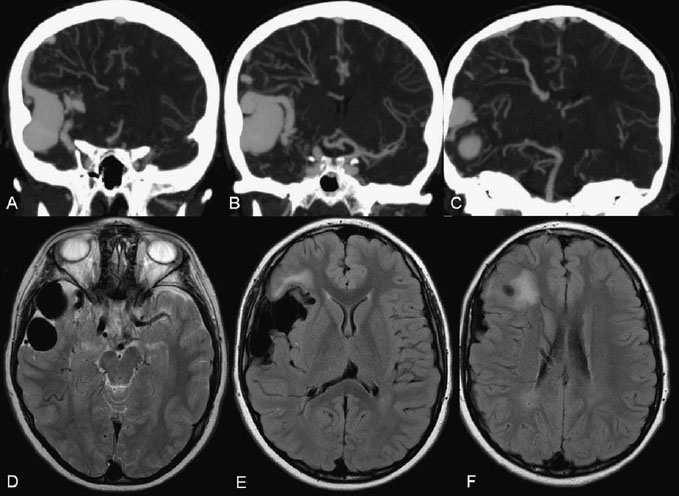
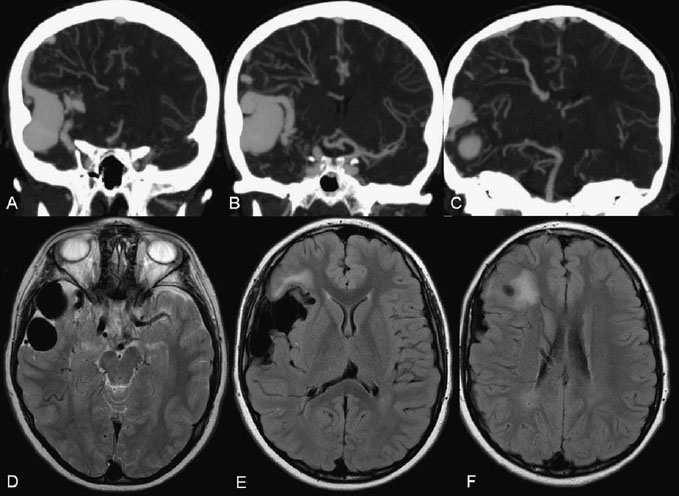
Fig. 57.1 (A–C)
Only gold members can continue reading.
Log In or
Register to continue
![]()