and Clarisse Dromain2
(1)
Department of Radiology, San Giovanni Hospital, Roma, Italy
(2)
Department of Radiology, Institut de Cancerologie Gustav Roussy, VilleJuif – Paris, France
Abstract
Abdominal angina or chronic mesenteric ischemia is a form of intermittent mesenteric ischemia in severe arterial stenosis with inadequate bowel perfusion triggered by food ingestion. Postprandial pain when blood flow goes away from the intestine due to the so-called gastric steal. Patients present typically with weight loss and clinical signs of malabsorption.
Abdominal Angina
Abdominal angina or chronic mesenteric ischemia is a form of intermittent mesenteric ischemia in severe arterial stenosis with inadequate bowel perfusion triggered by food ingestion.
Postprandial pain when blood flow goes away from the intestine due to the so-called gastric steal. Patients present typically with weight loss and clinical signs of malabsorption.
Duplex US can depict celiac trunk occlusion; a peak systolic velocity >160 cm/s in the celiac trunk during fasting has an SE of 57 % and SP of 100 % for 50 % stenosis.
CT enterography (or CT enteroclysis) is a powerful diagnostic tool in the identification of both splanchnic vessel strictures and bowel wall changes.
Biphasic scan is required in CT enterography by acquiring and arterial phase scan similar to CTA (CT angiography) and a delayed scan (enteric phase). CT enterography owing to contrast medium injection similar to CTA (CT angiography) with accurate post-processing (MIP, MPR, 3D VR) can easily depict with high accuracy strictures of the celiac trunk, SMA, and IMA showing also peripheric splanchnic vessels while the “enteric phase” (70 s after contrast medium injection) allows optimal evaluation of bowel wall changes.
CT enterography is able to depict chronic ischemic bowel wall changes in patients with abdominal angina such as bowel wall thinning, mucosal fold flattening, and long and smooth bowel strictures. Diagnostic information similar to those of CT enterography can be reached also using MR enterography or MR enteroclysis.
Abdominopelvic Incoordination
Abdominopelvic incoordination (pelvic floor incoordination) is a condition characterized by impaired coordination between pelvic floor (e.g., puborectal muscle) relaxation and abdominal wall motion leading to chronic constipation and obstructed defecation syndrome.
MR defecography is a valid tool to diagnose the abdominopelvic incoordination and to differentiate it from other possible causes of obstructed defecation syndrome such as descending perineum, rectal prolapse, and rectocele. This differential diagnosis is essential in treatment planning of obstructed defecation. In case of abdominopelvic incoordination, the clue sign at MR defecography is represented by paradox contraction of the puborectal muscle during defecation with missing anorectal angle opening leading to impaired evacuation.
“Accordion” Sign
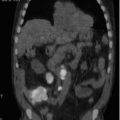
Accordion sign is a pattern of large bowel wall thickening suggesting acute inflammatory changes (acute infective colitis or pseudomembranous colitis). Marked thickening of haustral fold due to submucosa edema mimics an accordion appearance (Fig. 1).

Fig. 1
The marked and diffuse colonic fold thickening at the level of the transverse colon in this patient suffering from pseudomembranous colitis mimics an accordion appearance. This finding represents the so-called accordion sign: a sign of acute inflammatory colonic wall changes
Acute Mesenteric Ischemia
Etiology of acute mesenteric ischemia is represented by reduced blood flow to the bowel through mesenteric vessels due to occlusive embolus (occlusive mesenteric infarction) or SMA thrombosis or due to systemic low flow (hypovolemia, cardiac failure, intraoperative hypotension) in preexisting atherosclerosis of SMA (nonocclusive mesenteric ischemia).
Acute mesenteric ischemia may be present also in case of venous thrombosis (SMV, IMV, or portal vein) or may complicate bowel obstruction in case of strangulation by adhesion, volvulus, incarcerated hernia, or intussusception. Finally acute intestinal ischemia may be the manifestation of intestinal vasculitis or inflammatory abdominal process such as pancreatitis or peritonitis.
In case of occlusive mesenteric ischemia, usually occlusion is due to an embolus at the level of SMA bifurcation; if the embolus is located distal to the middle colic artery, no compensatory collateral vessel is available leading to mesenteric infarction.
Increased WBC is a common finding in case of acute mesenteric ischemia. Abdominal pain and gross rectal bleeding represent symptoms. Ischemia may involve any tract of the small bowel; concerning the colon, the distal transverse colon and cecum are the most common location. Consequence of acute mesenteric ischemia is represented by transmural infarction with perforation in case of irreversible ischemia or by restitution of bowel wall due to collaterals with fibrosis of the bowel with possible stricture formation.
Contrast-enhanced CT of the abdomen represents the imaging test of choice. Unenhanced CT scan followed by CTA of splanchnic vessels with dedicated post-processing acquiring also a delayed “enteric” CT phase (70 s) represents the winning CT protocol. Using such protocol detailed vascular information as well as direct assessment of bowel wall ischemic changes are easily detected.
Ischemic bowel wall changes are represented by bowel wall thickening with target appearance (alternating layers of high and low attenuation). In case of severe ischemia, reduced bowel wall enhancement is expected as well as wall thinning. The bowel wall usually is dilated and distended by fluid. Increased wall enhancement and delayed enhancement are possible due to venous congestion secondary to stasis. Intestinal pneumatosis is a sign of irreversible disease.
Adenomatous Polyp
An adenomatous polyp is a benign neoplastic growth with variable malignant potential, representing proliferation of glandular epithelium in the lumen of the colon–rectum. Several histopathology subtypes are described: the tubular, tubulovillous, villous, and sessile serrated. Malignant potential is associated with the degree of dysplasia, the histopathological subtype of polyp (5 % risk of cancer for tubular, 20 % for tubulovillous, and 40 % for villous), and the size of polyp (from <1 % for polyp <1 cm to 15 % for polyp ≥2 cm).
Although most adenomatous polyp is sporadic, it also is lined to some inherited disorders including the familial adenomatous polyposis, the Gardner syndrome, and the Lynch syndrome (HNPCC).
There are usually no symptoms. When present, symptoms may include rectal bleeding and bloody stools.
Screening plays an important role to prevent the transformation of polyp into cancer. People over age 50 should consider having screening test. Screening tests are represented by fecal occult blood test (FOBT), optical colonoscopy (that allows polypectomy), and virtual colonoscopy. People with a family history of colon cancer or colon polyps may need to be screened by colonoscopy at an earlier age (40 years).
When a polyp has been removed, follow-up colonoscopy is usually recommended 1–10 years later, depending on the age, the number of polyps depicted on the previous colonoscopy, and the size and pathology subtype; usually a 5-year follow-up is recommended.
Adenomatous Polyposis, Familial
Familial adenomatous polyposis (FAP) is an inherited condition resulting more often from mutations in the APC gene (autosomal dominant), less frequently from mutations in the MUTYH gene (autosomal recessive) that predispose to colorectal cancers. Hundreds or thousands of premalignant adenomatous colonic polyps appear around the age of 16 years old (from 7 to 36). Unless the colon is removed, these polyps will become malignant and most of patients will develop colon cancer by the age of 40. Less severe form, called attenuated familial adenomatous polyposis, is characterized with a lower number of polyp (mean 30), a location of polyps predominant in the proximal colon, and an average age of colorectal cancer of 55 years.
Extracolic signs may also suggest the diagnosis of FAP: pigmented lesions of the retina, jaw cysts, sebaceous cysts, and osteoma. The combination of FAP, osteomas of the skull, thyroid cancer, fibromas, and epidermoid cysts as well as the occurrence of desmoid tumors in approximately 15 % is termed Gardner syndrome. The combination of FAP with brain tumors, glioblastomas, astrocytomas, or medulloblastomas is termed Turcot syndrome.
Adhesive Intestinal Band
Adhesive intestinal band is a band of scar tissue in the abdominal cavity binding the intestinal loop one with each other or to other abdominal organ or to the abdominal wall. Adhesive band may be thin sheets or thick fibrous band.< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree