and Sofia Gourtsoyianni2
(1)
UOC Radiologia BR, Azienda Ospedaliera Universitaria Integrata Verona, Verona, Italy
(2)
Imaging 2, Level 1, Lambeth Wing St Thomas’ Hospital, London, UK
Acute Pancreatitis
Acute pancreatitis is an acute inflammation of the pancreas with variable involvement of other regional tissues or remote organ systems. Mild acute pancreatitis is associated with minimal organ dysfunction, while severe acute pancreatitis is associated with pancreatic necrosis and may lead to organ failure and/or local complications. The most common causes of acute pancreatitis are biliary stones and alcohol abuse, which account for up to 80 % of the cases.
In 2007, the Working Group Classification defined interstitial edematous pancreatitis and necrotising pancreatitis, redefining the terms that should be used to describe the collections present in each phase of the disease.
Interstitial edematous pancreatitis is characterised by a localised or diffuse enlargement of the pancreas, with normal homogeneous enhancement or slightly heterogeneous enhancement due to oedema. There is also mistiness or mild stranding of the peripancreatic fat. The fluid collections present in the early phase are called acute peripancreatic fluid collections (APFC). If these persist longer than 4 weeks, these will become pseudocysts.
In necrotising pancreatitis, areas of pancreatic necrosis appear as hypoattenuating nonenhancing parenchyma. The necrosis can be parenchymal, peripancreatic or both parenchymal and peripancreatic. After 4 weeks, these necrotic collections will develop a wall and become walled–off necrosis (WON or WOPN).
The revised Atlanta classification has abandoned the terms pancreatic abscess and intrapancreatic pseudocyst, which should not be used anymore.
Adenocarcinoma of the Pancreas
Pancreatic adenocarcinoma (PAC) has a dismal prognosis, with a mortality rate similar to its incidence and an overall 5-year survival rate lower than 5 %. Early diagnosis and resection are the only potential cure, but only a minority (5–30 %) will be diagnosed when still resectable.
CT is the diagnostic procedure of choice in the suspicion of PAC and is a reliable technique for its diagnosis and staging. Ductal adenocarcinoma typically appears as an ill-defined mass, surrounded by extensive desmoplastic reaction. PAC enhances poorly compared to the adjacent normal pancreatic parenchyma, appearing hypodense on arterial phase in most cases (75–90 %: Fig. 1), and may become isodense on delayed imaging.
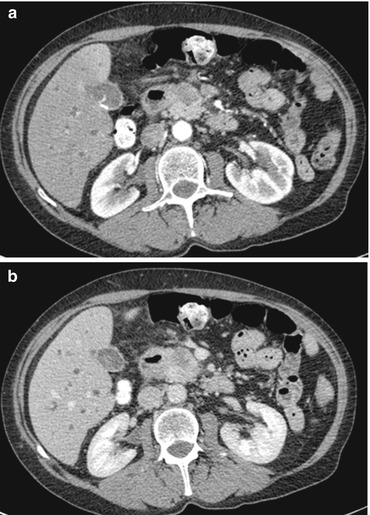
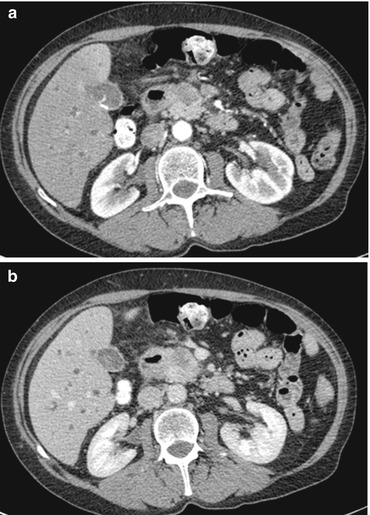
Fig. 1
Axial arterial phase (a) and portal-venous phase (b) CT images show a solid hypodense lesion in the ventral aspect of the pancreatic head, compatible with pancreatic carcinoma. The fat plane between the lesion and the superior mesenteric vein is preserved. Dilatation of the intrahepatic bile ducts is seen
CT correlates well with surgical findings in predicting unresectability (positive predictive value of 89–100%).
At MRI, PAC appears hypointense to the normal parenchyma on T1-weighted images, with or without fat suppression. On T2-weighted images, the tumour has variable appearance depending on the amount of desmoplastic reaction. After gadolinium administration, PAC usually shows less enhancement compared to the normal parenchyma in the arterial phase. MRI might visualise up to 79 % of the tumours that appear isodense at CT. Pancreatic carcinoma has a variable appearance on diffusion-weighted images; a high sensitivity and specificity have been reported for DWI in the detection of pancreatic adenocarcinomas.
Adenomyomatosis (Gallbladder)
Adenomyomatosis is a relatively common benign condition, identified in at least 5 % of cholecystectomy specimens. Most often an incidental finding, it frequently coexists with chronic cholecystitis. It is characterised by hypertrophy of the mucosa and muscularis propria and intraluminal cholesterol accumulation. Cholesterol crystals precipitate in the bile trapped in Rokitansky–Aschoff sinuses, intramural diverticula lined by mucosal epithelium. Gallbladder wall thickening and intramural diverticula containing bile with cholesterol crystals, sludge or calculi are the pathologic correlates of the imaging features of adenomyomatosis.
On CT the “rosary sign” has been described, formed by enhancing epithelium within intramural diverticula surrounded by the relatively unenhanced hypertrophied gallbladder muscularis.
On MRI gallbladder wall thickening and T2-w hyperintense, T1-w hypointense, nonenhancing intramural lesions in keeping with Rokitansky–Aschoff sinuses are demonstrated.
The pearl necklace sign is attributed to the characteristically curvilinear arrangement of multiple rounded hyperintense intraluminal cavities visualised at T2-weighted MR images. Diffuse, segmental and focal adenomyomatosis exist. Segmental or annular adenomyomatosis appears as limited circumferential gallbladder wall involvement with luminal narrowing, typically within the gallbladder body, which may produce a characteristic hourglass configuration. Focal or localised adenomyomatosis is most common, manifesting as crescentic to rounded gallbladder wall thickening, usually at the fundus. Focal adenomyomatosis may appear as a discrete mass, known as an adenomyoma.
Ampullary Tumours
These are tumours that arise from the glandular epithelium of the ampulla of Vater. The ampulla of Vater consists of the bile duct, the main pancreatic duct, the ampulla and the major duodenal papilla surrounded by the sphincter of Oddi.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree