8
Abdominal and Pelvic Malignancies
Sushmita Ghoshal, Bhavana Rai, and Raviteja Miriyala
INTRODUCTION
Radiation oncologists have long understood the potential benefit of radiation therapy (RT) in palliating the distressing symptoms of advanced abdominal and pelvic cancers. Often, the role of external beam radiation therapy (EBRT) or brachytherapy in controlling bleeding or obstructive symptoms finds only a passing reference1 and most palliative medicine texts are silent on this important topic. Apprehension of radiation-induced toxicities may be one reason for this omission. This argument is not entirely valid, as various short course palliative radiation schedules are planned such that treatment-related acute toxicity is minimal. Because the majority of patients treated with palliative intent have limited life expectancies, treatment-related late toxicity is seldom a major concern; moreover, it is important to weigh the potential toxicity against the efficacy and improvement in a patient’s quality of life (QoL).
Carcinomas arising in intra-abdominal organs are generally not treated with curative intent with RT alone due to a lack of therapeutic benefit. However, patients with advanced, inoperable disease may obtain symptom relief when treated by a short course of radiation. Intraluminal brachytherapy has been used for palliating obstructive symptoms of biliary tract cancers2 and is a safe procedure with minimal morbidity.3 Palliative RT achieves hemostasis in patients with unresectable gastric carcinoma not fit for systemic chemotherapy4 and is associated with a statistically significant rise in their hemoglobin levels. Several other studies have confirmed this benefit though the doses of radiation varied from a single fraction of 8 to 50 Gy in 25 fractions. All dose schemes have benefits in symptom control, with no statistically significant differences between patients who received a biologically effective dose (BED) less or more than 39 Gy, assuming the alpha-beta ratio to be 10.5
EBRT is an integral part of multimodality treatment for carcinoma of the rectum and anal canal and provides relief to patients with locally advanced or recurrent disease not amenable to surgical excision.6 Pelvis masses can cause pain, obstruction, tenesmus, bleeding, and discharge. Though most studies are retrospective without patient-reported QoL, they consistently demonstrate symptom relief and improved QoL with palliative pelvic RT. No statistically significant dose–response relationship has been established. James et al. reported a similar median duration of response in patients receiving <15 Gy or more.7 In the systematic review of palliative RT by Cameron et al8 in incurable primary and recurrent rectal cancer by palliative EBRT, all of the 27 studies reported good relief of pain, bleeding, and mass effect with acceptable toxicities. None of these studies had patient reported outcomes and various dose-fractionations were used. Most of these studies were retrospective chart reviews of patients treated more than two decades ago, with incomplete follow up. Despite these inherent shortcomings, the pooled response to palliative pelvic EBRT ranged from 71% to 81%. It was not possible to calculate the BED for comparison of different dose schedules. There is a need for prospective studies using modern RT techniques and uniform endpoints, to provide robust evidence about the risk–benefit ratio of palliative pelvic RT in advanced rectal carcinoma. In patients with locally advanced and metastatic rectal cancer,35 a hypofractionated radiation therapy course can limit the need for palliative colostomy to 33%. This regimen was associated with an 82% local control rate with less than 10% mild acute toxicity and no late toxicity.
Patients with locally advanced or metastatic bladder cancer may benefit from palliative RT to the pelvis. Fossa and Hosbach reported on their experience treating all symptomatic patients above age 80 and younger patients with distant metastasis with palliative pelvic RT.9 Using a moderate dose of 30 Gy in 10 fractions over 2 weeks, patients experienced a significant reduction in hematuria. In a retrospective review of 94 patients, Salminen reported complete and partial relief of symptoms, 43% and 29% respectively, with 30 Gy in 6 fractions over 3 weeks.10 Eight out of 17 patients did not need the indwelling catheter after radiation. The estimated median survival was 9.6 months. There was a local control rate of 40% which was associated with longer survival. In a systematic overview article, Widmark et al. reported that it is possible to decrease tumor-induced bladder symptoms rapidly and effectively with palliative EBRT.11 Also, a hypofractionated 1-week regimen was as effective as a 2-week daily treatment in doing this.
RT has been used for symptom relief in gynecological malignancies for many years. Both brachytherapy and EBRT have been used successfully to obtain hemostasis in carcinoma cervix. Boulware et al., from the MD Anderson Cancer Center, published their experience using hypofractionated radiation 10 Gy once a month for 3 months.12 After 3 fractions, vaginal bleeding was controlled in all patients. However, care must be taken to not to use very high doses per fraction radiation for patients with potentially curable disease and long anticipated survival. In addition to bleeding, radiation palliates pain, obstructive symptoms, and vaginal discharge. Sklirenko and Barnes reported overall symptom response rates of 45% to 100% for bleeding, 0% to 83% for pain, 39% to 49% for discharge, and 19% to 100% for obstructive symptoms.13 The RTOG 7905 trial was based on the MD Anderson experience and added concurrent Misonidazole, a hypoxic cell sensitizer, to the radiation. This trial closed prematurely due to excessive gastrointestinal complications and a different hypofractionated regimen was designed.14 RTOG 8502, used twice a day radiation for 2 days, 3.7 Gy/fraction, a regimen now known as the QUAD shot. The cycle was repeated monthly up to a maximum of three times or maximum dose of 44.4 Gy.15,16 This led to a significant decrease in early and late toxicities. At Princess Margaret Hospital (PMH), 7 Gy/fraction is delivered on a weekly basis for 3 weeks.17 In their 10-year experience, vaginal bleeding was controlled in 92% patients and the regimen was comparable to the other hypofractionated regimens in terms of efficacy and toxicity.
Two centers in India who routinely use monthly palliative pelvic radiation for advanced carcinoma cervix published their experience of using parallel opposed megavoltage radiation. Mishra et al. used 10 Gy/fraction18 with additional brachytherapy in five patients while Rai et al.19 used 8 Gy/fraction. Both studies reported good control of symptoms like vaginal bleeding, discharge, and pain. Carcinoma of the cervix is a common disease within developing countries, where many patients report late to the hospital with incurable disease. A short course of hypofractionated radiation can control their distressing symptoms, improve QoL, and reduce hospitalization with minimal treatment-related toxicity.
It is unlikely that prolonged fractionation can produce more effective or durable palliation as compared to short, hypofractionated ones. Since higher radiation doses per fraction have a higher potential for late toxicity, which generally occurs 9 months after completion of treatment. Therefore, it is important to carefully select patients for hypofractionation. In patients with limited life expectancies, a short but effective dose of palliative pelvic radiation will produce adequate symptom relief without increasing the burden for patients and caregivers.
TREATMENT PLANNING BY SITE
The aim of palliative RT is to improve the QoL of patients with incurable disease, by providing maximum symptom relief, while minimizing treatment-related acute toxicities and durations of hospital stays. This can be achieved by minimizing the field sizes and number of fractions while maintaining the therapeutic index.
With proper patient selection, delayed toxicities are seldom of concern while planning palliative RT, thereby allowing a wider freedom in choosing the field sizes and target volumes for various sites. Hence, it becomes impractical to have stringent practice guidelines for planning palliative RT. Treatment planning recommendations for typical case scenarios encountered in clinical practice are given in the following section. However, treatment volumes and field sizes should be selected appropriately on a patient-by-patient basis, considering various factors like life expectancy, performance status, disease burden, severity of symptoms, comorbidities, goals of therapy, and departmental logistics.
Most often, conventional planning based on bony landmarks is adequate for treatment planning, especially in developing countries with limited resources. In centers where conventional simulators have been superseded by CT simulators, virtual simulation is used for treatment planning.
The following cases illustrate the role of palliative-radiation therapy in the treatment of bladder cancer, vaginal bleeding, rectal cancer, vulvar cancer, and liver metastasis. Further discussion of the role of palliative radiation therapy for liver tumors can be found in Chapter 9.
Case 8.1: Palliative Treatment of the Bladder
A 75-year-old patient of carcinoma of the urinary bladder, with widespread bone and lung metastases, presents with dysuria and pelvic pain. He had coronary artery disease and a poor performance status. Being unsuitable for systemic chemotherapy, he was planned for palliative pelvic RT.
Simulation for such patients is done in the supine position, preferably with an empty bladder. Parallel opposed antero-posterior fields are generally used. The upper border is placed at L5–S1 interface; lower border at the level of ischial tuberosities; lateral borders are placed 2-cm lateral to the widest part of the pelvic brim (Figure 8.1).
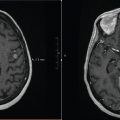
If virtual simulation is planned, a noncontrast CT scan is taken in supine position with empty bladder. Gross tumor along with the entire urinary bladder and prostatic urethra is delineated and a margin (2–2.5 cm) is given to account for internal motion and set up uncertainties. Conformal radiation with two or three fields is delivered using multileaf collimation (Figure 8.2).

FIGURE 8.1 Palliative RT portal for antero-posterior fields, urinary bladder cancer.

FIGURE 8.2 Conformal radiation plan for urinary bladder cancer.
Case 8.2: Palliative Radiation for Vaginal Bleeding
A 68-year-old female presented with foul smelling discharge and bleeding per vaginum; examination revealed a large ulcero-proliferative growth replacing the entire cervix and extending to the lateral pelvic walls, with a frozen pelvis. After further evaluation she was diagnosed with poorly differentiated squamous cell cancer of the cervix, with extensive para-aortic and supraclavicular nodal metastases, and bilateral gross hydro-uretero-nephrosis and deranged renal function. She was planned for palliative pelvic radiation.
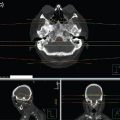
For such patients, a four-field box technique or a simpler two-field technique is adequate for palliation. Simulation is done in supine position with an empty bladder. Simple positioning devices like knee wedges may be used. The upper margin of the field is generally placed at L4–L5 interface; however, it can be brought down to L5–S1 interface in certain cases if field size is too large. Lateral margins are placed 2-cm lateral to the widest part of the pelvic brim. Lower margin should be placed at least 2 cm beyond the lower extent of the disease, and inferior margin of the obturator foramen is an adequate bony landmark for most cases (Figure 8.3). However, if there is extension of growth into the lower vagina, the patient should be simulated in a frog-leg position with antero-posterior fields, and lower border placed to cover the introitus. For patients without lower vaginal extension, two lateral fields can be added by placing the anterior border at the anterior cortex of pubic symphysis and posterior border to cover the sacral hollow (Figure 8.4). Virtual simulation and conformal planning may be used in selected cases and fields with differential weightage can be used for improved dose distribution.

FIGURE 8.3 Antero-posterior portals for palliative RT of cervical cancer.

FIGURE 8.4 Lateral fields for palliative RT of cervical cancer.
Case 8.3: Palliative Radiation Therapy for Rectal Cancer
A 65-year-old patient with adenocarcinoma of the rectum underwent abdomino-perineal resection and adjuvant chemotherapy 7 years ago. Now he presented with multiple liver metastases, along with local recurrence, causing pelvic pain. He did not respond to second-line chemotherapy, and was offered palliative pelvic RT.
Simulation for patients of rectal cancer is generally done in the prone position for better reproducibility, unless patients have an existing colostomy. Antero-posterior fields or four-field box technique is generally used, similar to patients of cervical cancer; however, the upper margins are usually placed at L5–S1 interface. For lateral fields, the anterior margins are placed at the posterior cortex of symphysis pubis, and posterior border is generally placed 1.5 cm behind the anterior sacral margin (Figure 8.5). For conformal radiation, gross primary tumor along with adequate margins on either side is delineated and a margin is given for set up errors. Generally, uninvolved nodal regions are not included in palliative radiation.

FIGURE 8.5 Lateral portals for four-field box technique, rectal cancer.
Case 8.4: Palliative Radiation Therapy for Vulvar Cancer
A 73-year-old female presented with a large ulcero-proliferative growth over her external genitalia, and was diagnosed as a case of vulval cancer, extending into the lower third of vagina and urethra. Due to multiple comorbidities and poor performance status, she was considered for palliative RT.
Simulation for such patients of vulval cancer is preferably done in frogleg position, and antero-posterior fields are adequate. Tissue equivalent bolus material is generally placed during treatment to increase the superficial dose. Upper border is placed at midsacroiliac joint and lower border should flash the entire perineum and the gross disease with adequate margin. Lateral borders are placed 2-cm lateral to the pelvic inlet. If there is gross inguinal nodal enlargement, fields may be extended laterally. Alternatively, a single incident field may be used by rotating the couch and gantry for treating the gross disease in appropriately selected patients (Figure 8.6).

FIGURE 8.6 Single-field technique with couch and gantry rotation for palliation of vulval cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree