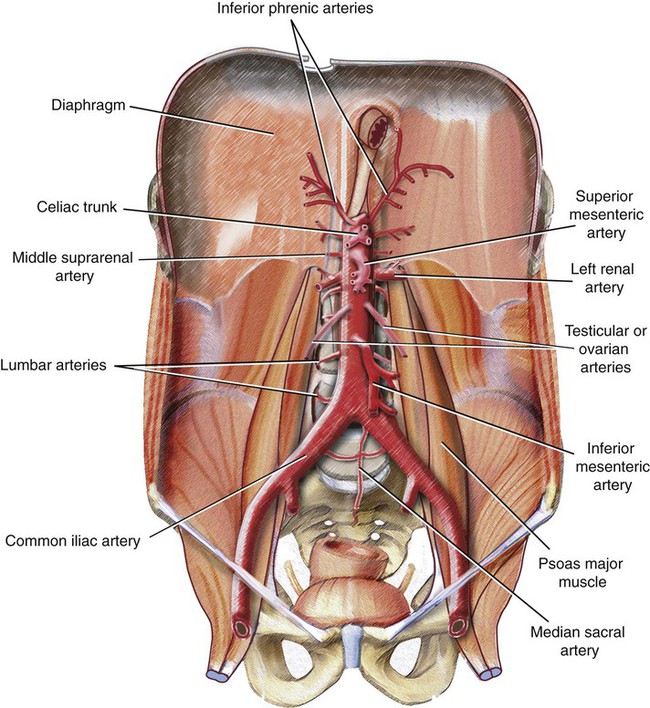
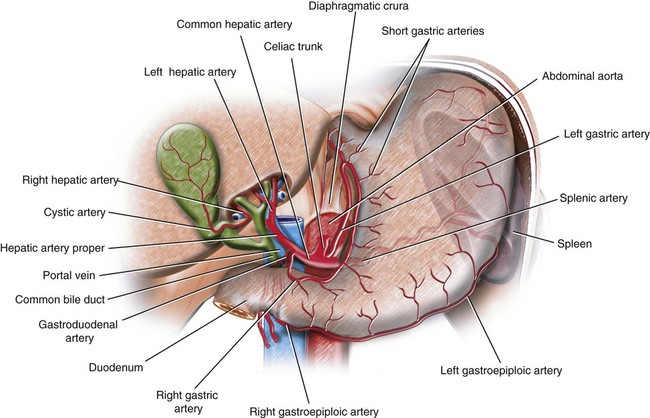
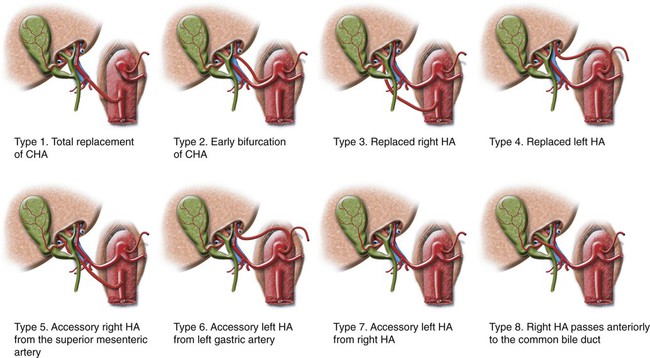
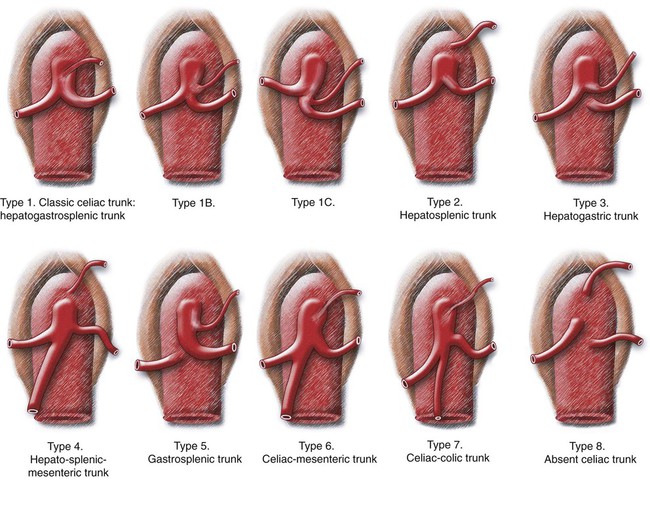
Chapter 46 Amber Jones and Monica Smith Pearl Imaging of the abdominal aorta may be accomplished by ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI). Ultrasound is widely available, portable, and lacks ionizing radiation, but it is heavily operator dependent and thus its reproducibility is variable.1 Other challenges arise when there is excess bowel gas and obesity. Multidetector CT is a noninvasive imaging technique that allows for rapid image acquisition and high spatial resolution, including nearly isotropic submillimeter resolution in the X, Y, and Z planes.2 Other advantages of multidetector CT include widespread availability, detailed evaluation of the aortic wall and lining mural thrombus, detection of unsuspected extraluminal abnormalities, and multiplanar postprocessing for interventional planning.2 MRI is another noninvasive imaging modality that has the potential to illustrate the arterial anatomy of the abdominal aorta and its branches. Time-of-flight (TOF) and phase-contrast (PC) magnetic resonance angiography (MRA) are two well-known techniques that rely on flowing blood to image the arterial system. These techniques, however, are prone to artifacts related to disruptions or variations in blood flow, as seen with pulsatile and turbulent flow.3 Gadolinium (Gd)-enhanced three-dimensional (3D) MRA, introduced in the early 1990s, relies on the T1 shortening effects of circulating Gd-chelate contrast media instead of on flowing blood. The technique is quick, easy to perform, and provides high-resolution 3D images with minimal artifacts related to spin saturation, slow flow, or turbulent flow associated with TOF.3 As the aorta descends through the abdominal cavity, it gives off anterior, lateral, and posterior branches. Anterior branches include the celiac trunk, superior mesenteric artery, and inferior mesenteric artery, which supply the gastrointestinal viscera, as well as the phrenic and gonadal arteries (Fig. 46-1). The celiac trunk is the first wide anterior branch of the abdominal aorta; it arises just below the diaphragmatic hiatus and anterior to the superior part of the first lumbar vertebra. It supplies the foregut, which includes the abdominal esophagus, stomach, duodenum superior to its major papilla, liver, pancreas, and gallbladder. Blood supply to the spleen also develops in relation to that of the foregut region (Fig. 46-2). (See Chapter 52 for further discussion of the celiac trunk and its branches.) Eight different types of variations have been described, the most common being replacement of either the right hepatic artery from the superior mesenteric artery (type 3) or the left hepatic artery from the left gastric artery (type 4). Other replaced variants include the common hepatic artery from the superior mesenteric artery (type 1). Accessory variants include an accessory right hepatic artery from the superior mesenteric artery (type 5) and an accessory left hepatic artery from either the left gastric artery (type 6) or the right hepatic artery (type 7). A type 2 variant involves early bifurcation of a short common hepatic artery or separate origins of the right and left hepatic arteries from the celiac trunk, with the gastroduodenal artery arising from the right hepatic artery. Additionally, variant anatomy may involve the pathway of the artery, with a type 8 variant involving the right hepatic artery passing anterior to the common hepatic duct instead of posteriorly. These variants can occur in isolation or together (Fig. 46-3). The gastroduodenal artery is a short but large branch of the common hepatic artery that descends near the pylorus between the superior part of the duodenum and the pancreatic neck. (See Chapter 52 for further discussion of the gastroduodenal artery.) The superior pancreaticoduodenal artery divides into anterior and posterior branches as it descends between the duodenum and pancreatic head, and supplies these structures. (See Chapter 52 for further discussion of the superior pancreaticoduodenal artery.) The pancreaticoduodenal arteries enlarge and provide important collateral pathways between the celiac trunk and superior mesenteric artery in the case of stenosis or occlusion of either aortic branch. Classic celiac trunk anatomy is present in up to only 70% of individuals; a wide range of variants may exist. Awareness of these variations is essential for visceral vascular imaging. Couinaud described eight different types of variations of the celiac trunk (Fig. 46-4). Type 1 involves a classic configuration of the celiac trunk, with all three branches arising as a trunk from the abdominal aorta. The variation exists in the possible subtypes: a hepatosplenic trunk, with the left gastric artery arising from the trunk; a hepatogastrosplenic trunk, with the three arteries arising simultaneously in a trifurcation; or a gastrosplenic trunk in which the splenic artery is dominant and the hepatic artery arises from the splenic artery. Another variant described involves a common trunk for two arteries, the hepatic and splenic arteries for type 2 and the hepatic and left gastric arteries for type 3, whereas the third artery, the left gastric artery in type 2 and the splenic artery in type 3, arises directly from the aorta. Alternatively, the splenic artery in type 3 may arise from the superior mesenteric artery. Similar to a type 2 variant is type 4, in which the left gastric artery arises directly from the aorta; however, the common trunk comprises the hepatic, splenic, and superior mesenteric arteries. The most complex configuration is type 5, in which the left gastric and splenic arteries form a common trunk, and the common hepatic artery, when present, may arise from the aorta or superior mesenteric artery. When the hepatic artery does not exist, it is replaced by the right, left, or both hepatic arteries at the same time. Types 6 and 7 involve additional arteries arising from the celiac trunk, including the superior mesenteric artery in type 6 and the left colic or middle colic arteries in type 7. Additionally, the three main arteries may arise directly from the aorta as in type 8. The superior mesenteric artery is the anterior branch of the abdominal aorta supplying the midgut, which includes the entire small bowel from the duodenum inferior to its major duodenal papilla, the cecum, the appendix, the ascending colon, and the right two thirds of the transverse colon. (See Chapter 52 for further discussion of the superior mesenteric artery and its branches, including the inferior pancreaticoduodenal artery, jejunal and ileal arteries, and middle colic, right colic, and ileocolic arteries.) The inferior mesenteric artery supplies the hindgut, which includes the left third of the transverse colon, the descending colon, the sigmoid colon, the rectum, and the upper part of the anal canal. It is the smallest of the three anterior branches of the abdominal aorta and arises anterior to the body of the third lumbar vertebra a few centimeters above the aortic bifurcation into the common iliac arteries. (See Chapter 52 for further discussion of the inferior mesenteric artery and its branches, including the left colic artery, sigmoid arteries, and superior hemorrhoidal [rectal] artery.)
Abdominal Aorta and the Inferior Vena Cava
Abdominal Aorta
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine