Fig. 28.1
Abdominal x-ray (a) shows features of small bowel obstruction with grossly distended gas filled small bowel loops. The expanded panel (b) shows valvulae conniventes (white arrows) traversing the full width of the bowel loops confirming it as small bowel
Distended air-filled loops may lay in a tiered or stepladder pattern on upright or lateral decubitus views as the air rises to form a series of short air-fluid levels. When these air-fluid levels are horizontally or obliquely oriented, it is known as the “string of pearls” sign (Fig. 28.2). Air- fluid levels see at differing heights within the same bowel loop (“Stepladder” air fluid levels) on upright positioning indicate small bowel obstruction, particularly in the early stages. In a high-grade, prolonged small bowel obstruction there may not be differential air-fluid levels or any air filled loops at all as the bowel becomes filled with fluid (Fig. 28.3). Variable amounts of air are present in the colon, depending on level, grade and duration of the obstruction. If the small bowel is distended and fluid-filled while the colon is collapsed small bowel obstruction must be suspected. Upright or lateral decubitus radiographic views are essential when evaluating for obstruction because distended small bowel loops containing mostly fluid are not well visualized on supine radiograph.
Fig. 28.2
Erect abdominal x-ray shows multiple air-fluid levels in the central abdomen aligned in a linear fashion (see e expanded panel) – the “string of pearls” sign if small bowel obstruction
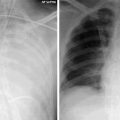
Fig. 28.3
Featureless abdomen with paucity of bowel gas resulting from fluid-filled distended small bowel loops in a patient with high-grade, prolonged small bowel obstruction
Ultrasound is not commonly used for SBO because air reflects sound waves creating a “dirty shadowing” that obscures the view of adjacent bowel loops. Repositioning the patient on their side and imaging from a more dependent portion of the abdomen may help identify fluid filled loops because air rises and the probe will be closer to the fluid-containing portion of the bowel. When the bowel is near completely fluid filled a small bowel obstruction can be diagnosed because of the number and size of fluid filled bowel loops (Fig. 28.4). Ultrasound is limited in determining the cause of obstruction. Adhesions, the most common cause of mechanical SBO, are not detected with this method.
Fig. 28.4
Abdominal ultrasound in a patient with multiple markedly distended anechoic small bowel loops (note valvulae connavientes) in a patient with small bowel (asterix) obstruction
The main CT finding in small bowel obstruction is markedly distended fluid and sometimes gas filled loops proximal to the point of obstruction as compared to the nondilated bowel distal to the obstruction (Fig. 28.5a, b). A potential pitfall is the normal appearance of a collapsed descending colon, even in a patient with adynamic ileus. Bowel obstruction should not be diagnosed in this setting unless an obstructing lesion is visualized at the splenic flexure or there is distension throughout the bowel proximal to the splenic flexure. The “small bowel feces” sign is a definitive CT finding for small bowel obstruction. It is seen when a slowly transiting succus entericus becomes overgrown with bacteria and partially dehydrated creating the appearance of feculent contents mixed with gas bubbles within dilated small bowel (Fig. 28.6).
Fig. 28.5
Selected CT images show markedly distended fluid filled small bowel loops (asterix) (a, b) in contrast to the more normal caliber ascending colon (arrowhead) (b) in keeping with small bowel obstruction
Fig. 28.6
CT image shows mottled gas admixed with fluid in the small bowel (arrow) – the “small bowel feces” sign – is a definitive CT finding for small bowel obstruction
Contrast-enhanced, multidetector CT imaging is the method of choice to evaluate for complications of obstruction such as intestinal ischemia or contained perforation. Oral contrast is optional and is often discouraged as the fluid naturally accumulating in the bowel makes the loops easy to visualize. Giving oral contrast to patients with bowel obstruction may lead to vomiting and aspiration. The appearance of the bowel wall on i.v. contrast-enhanced CT changes as it progresses from ischemia to infarction. When obstruction is complicated by strangulation and ischemia, CT demonstrates circumferential thickening of the bowel wall (>3 mm) and may contain a target or halo appearance.
The target sign (Fig. 28.7) describes three concentric rings of high and low attenuation of the bowel wall. It is seen when an ischemic injury starts at the mucosa and extends progressively through the wall to the serosa and is formed by inner and outer layers of high attenuation surrounding an edematous central area of decreased attenuation. It is best visualized during a late arterial or early portal venous phase of IV contrast enhancement. Poor enhancement of the bowel wall along its mesenteric border suggests ischemia whereas poor or absent mucosal enhancement with thinning of the bowel wall provides evidence of bowel infarction. Most strangulated obstructions, such as incarcerated hernias or volvulus, are closed loop obstructions where both afferent and efferent limbs are involved. They have a U-shaped or C-shaped configuration on axial CT with a “beak” sign at the site of torsion seen as fusiform tapering of a dilated bowel loop (Fig. 28.8a, b).
Fig. 28.7




CT images obtained during intravenous contrast enhancement show concentric rings of high and low attenuation of the bowel wall – the target sign – a feature seen in ischemic bowel
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree