Ultrasonography is low in cost, noninvasive, and highly portable, and it allows real-time imaging in multiple operator-controlled planes. As a result, it is the most widely used cross-sectional imaging modality worldwide. The principal challenge with ultrasonography is greater user-dependence than computed tomography (CT) or magnetic resonance imaging (MRI).
Basic Physics
Definition
Humans can hear sound that vibrates from 20 Hertz (Hz) to 20,000 Hz. Ultrasound is the term given to describe sound at frequencies above 20,000 Hz, beyond the range of human hearing. Frequencies of 3 to 7 megahertz (MHz) are commonly used for abdominal ultrasound.
Properties of Ultrasound
Ultrasound waves propagate as longitudinal waves in soft tissues. Acoustic impedance is an intrinsic physical property of a medium defined as the density of the medium multiplied by the velocity of ultrasound wave propagation in the medium. Acoustic interfaces exist between materials that have different acoustic impedances. Reflection, refraction, and scatter occur when ultrasound waves meet an acoustic interface. The greater the acoustic impedance difference between two sides of the interface, the greater is the ultrasound energy that will be reflected.
The relationship among frequency (f), velocity (c), and wavelength (λ) is λ = c/f. The higher the frequency, the shorter is the wavelength. In theory, the distance that can be measured by ultrasound is ![]() λ. The shorter the wavelength, the better the resolution will be. With the wavelength shortened, the attenuation will be greater. So a low-frequency probe should generally be selected to examine the deep organs of the abdomen (e.g., liver, kidney, pancreas), and high-frequency probes should be selected to examine superficial tissues (e.g., abdominal wall, appendix) ( Figures 3-1 and 3-2 ).
λ. The shorter the wavelength, the better the resolution will be. With the wavelength shortened, the attenuation will be greater. So a low-frequency probe should generally be selected to examine the deep organs of the abdomen (e.g., liver, kidney, pancreas), and high-frequency probes should be selected to examine superficial tissues (e.g., abdominal wall, appendix) ( Figures 3-1 and 3-2 ).


The velocity of ultrasound is affected by the density and elasticity of the material it traverses; as a result, ultrasound travels at varying velocities through different tissues. Current commercially available ultrasound machines cannot determine which tissues underlie the transducer and instead assume an average tissue velocity of 1540 m/s in their image reconstruction algorithms. The value is obtained from averaging the velocity in normal soft tissue ( Figure 3-3 ).

Safety
The American Institute of Ultrasound in Medicine has addressed ultrasound safety and bioeffects, as follows: “No independently confirmed adverse effects caused by exposure from present diagnostic ultrasound instruments have been reported in human patients in the absence of contrast agents.” Biological effects (such as localized pulmonary bleeding) have been reported in mammalian systems at diagnostically relevant exposures, but the clinical significance of such effects is not known. Ultrasound should be used by qualified health professionals to provide medical benefit to the patient. Ultrasound exposures during examinations should be as low as reasonably achievable.
Instrumentation
A diagnostic ultrasound machine is commonly composed of a transducer (probe) and main body. An electronic transducer is composed of a large number of piezoelectric materials. Ultrasound is produced from piezoelectric material that vibrates in response to the application of electrical energy. Piezoelectric material can be arranged on a plane (linear transducer) or a curved surface (curved transducer). Linear high-frequency transducers are typically used for superficial tissue imaging—for example, appendix, abdominal wall, and scrotum. Low-frequency curved array transducers are typically used for abdominal and obstetric/gynecologic imaging, in which the curvature of the array and penetration depth facilitate large field of view imaging.
When ultrasound travels through tissues, reflection, refraction, and scatter will occur at acoustic interfaces. The reflected and/or scatted ultrasound waves are detected by the transducer and analyzed. Each echo is displayed at a point in the image that corresponds to the relative position of its origin within the body. The brightness of each point in the image is related to the strength of the echo. This form of ultrasound imaging is termed B-mode (brightness mode) sonography and is often colloquially termed “gray scale” sonography or “conventional” sonography.
General Abdominal Ultrasonography
Ultrasonography can be used to visualize solid structures in the abdomen, the abdominal wall, and some gastrointestinal lesions. The vasculature within these organs can be evaluated by color Doppler, power Doppler, or spectral modes. Body markers or anatomic labels are used to illustrate the position of the patients and transducer. A basic glossary of ultrasound terms is listed in Table 3-1 .
| Term | Description | Example |
|---|---|---|
| Anechoic | Without echoes; displayed as black in the image | Normal urine and bile |
| Hypoechoic | Tissues that create dimmer echoes than adjacent tissues | Cortex of lymph nodes, some tumors |
| Hyperechoic | Tissues that create brighter echoes than adjacent tissues | Air, bone, perinephric fat |
| Acoustic shadow | The decreased echogenicity of tissues that lie behind a structure that causes marked attenuation or reflection of the ultrasound waves | Typically deep to solid structures (stones, bone) or air |
| Acoustic window | A tissue or structure that offers little obstruction to the ultrasound waves and can therefore be used as a route to obtain images of a deeper structure | Bladder full of urine, gallbladder full of bile |
| Cystic | A fluid-filled structure (mass) with thin or thick walls, with or without strong back wall reflections and enhancement of the echoes behind the cyst | Liver, renal cysts common |
| Solid | Tissue that does not include fluid spaces; will be multiple internal echoes and moderate attenuation of the ultrasound | Solid tumor, liver, muscle |
Equipment
An ultrasound machine capable of real-time imaging should be used to examine the abdominal organs. The equipment should be adjusted to obtain acceptable resolution. For adults, a curved probe with frequencies between 2 and 5 MHz is most commonly used. A linear probe with frequencies between 5 and 7 MHz is most commonly used when the abdominal wall and appendix are examined. Image quality should be optimized while keeping total ultrasound energy exposure as low as reasonably achievable.
Preparation for Examination
The patient should not eat or drink for 8 hours before the abdominal ultrasound. If fluid is essential to prevent dehydration or take medicine, only water should be given. When the bladder needs to be examined, 400 to 600 mL water should be taken orally 2 hours before examination to ensure there is enough urine in the bladder. Emergency ultrasonography can be performed at any time, but the image quality may be affected by air in stomach and bowel.
General Abdominal Ultrasonography
Ultrasonography can be used to visualize solid structures in the abdomen, the abdominal wall, and some gastrointestinal lesions. The vasculature within these organs can be evaluated by color Doppler, power Doppler, or spectral modes. Body markers or anatomic labels are used to illustrate the position of the patients and transducer. A basic glossary of ultrasound terms is listed in Table 3-1 .
| Term | Description | Example |
|---|---|---|
| Anechoic | Without echoes; displayed as black in the image | Normal urine and bile |
| Hypoechoic | Tissues that create dimmer echoes than adjacent tissues | Cortex of lymph nodes, some tumors |
| Hyperechoic | Tissues that create brighter echoes than adjacent tissues | Air, bone, perinephric fat |
| Acoustic shadow | The decreased echogenicity of tissues that lie behind a structure that causes marked attenuation or reflection of the ultrasound waves | Typically deep to solid structures (stones, bone) or air |
| Acoustic window | A tissue or structure that offers little obstruction to the ultrasound waves and can therefore be used as a route to obtain images of a deeper structure | Bladder full of urine, gallbladder full of bile |
| Cystic | A fluid-filled structure (mass) with thin or thick walls, with or without strong back wall reflections and enhancement of the echoes behind the cyst | Liver, renal cysts common |
| Solid | Tissue that does not include fluid spaces; will be multiple internal echoes and moderate attenuation of the ultrasound | Solid tumor, liver, muscle |
Equipment
An ultrasound machine capable of real-time imaging should be used to examine the abdominal organs. The equipment should be adjusted to obtain acceptable resolution. For adults, a curved probe with frequencies between 2 and 5 MHz is most commonly used. A linear probe with frequencies between 5 and 7 MHz is most commonly used when the abdominal wall and appendix are examined. Image quality should be optimized while keeping total ultrasound energy exposure as low as reasonably achievable.
Preparation for Examination
The patient should not eat or drink for 8 hours before the abdominal ultrasound. If fluid is essential to prevent dehydration or take medicine, only water should be given. When the bladder needs to be examined, 400 to 600 mL water should be taken orally 2 hours before examination to ensure there is enough urine in the bladder. Emergency ultrasonography can be performed at any time, but the image quality may be affected by air in stomach and bowel.
Normal Ultrasound Image
Liver
The normal liver parenchyma appears homogeneous, interrupted by the portal vein, hepatic vein, and their branches. The echogenicity of the liver should be compared with that of the right kidney. The liver can be similar or more echogenic than normal kidney. The hepatic veins, the main portal vein, and the right and left branches of the portal vein should be seen clearly ( Figure 3-4 ).
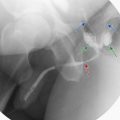
Gallbladder and Bile Duct
On the longitudinal scan, the gallbladder will appear as an anechoic, pear-shaped structure. It is variable in position, size, and shape, but the normal gallbladder is seldom more than 40 mm wide. The thickness of normal gallbladder wall is no more the 3 mm ( Figure 3-5 ). The intrahepatic bile ducts usually are located above the corresponding portal branches. The common bile duct (CBD) is located anterior the portal vein. The normal diameter of the CBD is less than 6 mm. Ultrasonography has limited capacity to detect small lesions within the distal CBD. Sometimes, tiny stones in the CBD can be detected ( Figure 3-6 ).