This chapter will review the basics of abusive head and spinal trauma, focus on common questions that arise when interpreting imaging studies of children with inflicted injuries of the central nervous system, and discuss the pros and cons of various imaging approaches. This chapter is written in a question-and-answer format.
Abusive Head Trauma
Demographics, Clinical Presentation, and Outcomes
What Is Abusive Head Trauma?
Various definitions of abusive head trauma (AHT) are found in the medical literature. The Centers for Disease Control and Prevention defines AHT as injury to the skull or intracranial contents of an infant or young child (<5 years of age) due to inflicted blunt impact and/or violent shaking.
How Common Is AHT?
The incidence of AHT in the United States is estimated at approximately 25-40 cases per 100,000 children younger than 1 year of age. The incidence of AHT then decreases over the next four years of life.
What Are the Classic Features of AHT?
Intracranial subdural hematomas (SDHs), retinal hemorrhages (RHs), and encephalopathy are the classic features of AHT. These findings are often observed in the absence of external signs of injury.
Which Signs and Symptoms May Be Observed in a Child with AHT?
Signs and symptoms that may be observed in a child with AHT include a decreased level of consciousness, such as irritablility or lethargy, recurrent vomiting (especially in the absence of fever or diarrhea), respiratory difficulties, seizures, and facial and scalp bruising and/or swelling. In a severe case of AHT, a child may present in a coma with respiratory difficulties or cardiopulmonary arrest.
Are There Certain “Red Flags” That Should Alert the Clinician to the Possibility of Abuse in a Child With Neurological Deficits?
Causes for concern include unexplained injuries (such as scalp swelling; bruising of the face, ears, neck, and torso, burns, and frenulum tears), inconsistencies or changes in the history provided by the caretaker, and unexplained delays in seeking medical care for an injured child. In addition, the mechanism of injury provided by the caretaker should adequately explain the pattern of injuries observed on the clinical and imaging examinations.
What Other Causes of Traumatic Head Injury Are There in Very Young Children Other Than Abuse?
Head injury can also be caused by accidental trauma, trauma related to recent birth, and trauma arising from neglectful or inadequate supervision. The CDC does not include head injury arising from gunshot wounds, stab wounds, or penetrating trauma in the definition of AHT.
What Are the Proposed Mechanisms of Injury in Cases of AHT?
Mechanisms of injury include: (1) impulsive loading arising from rigorous and repetitive shaking of a child that may or may not terminate with blunt impact; (2) impact loading from blunt force (e.g., a child is thrown, dropped, punched, or hit in the head or the head is manually compressed; and (3) strangulation or suffocation. More than one mechanism may be contributory. Knowledge of these mechanisms of injury is derived from witnessed accounts of traumatic events and admissions by caretakers and is inferred based on known injury patterns with well-described causal accidental mechanisms.
Are There Certain Triggers That May Contribute to a Caretaker Intentionally Injuring a Child?
Commonly described triggers that can lead to a caretaker injuring a child are frustration and stress, which can occur or intensify when a child cries or has been crying for a period of time. Because a child will often stop crying when the brain is injured, the act of shaking may be reinforced.
Is There a Specific Age Range or Type of Child That Is at Increased Risk for AHT?
Most cases of AHT occur within the first year of life, with a peak incidence observed at approximately 10 to 13 weeks of age and then decrease in incidence thereafter. Children at greater risk for being abused are those with perinatal complications, those born prematurely or with major birth defects, “colicky” infants, and male infants. Additional risk factors include young parents, unstable family situations, families living at or below the poverty level, and caretakers with tendencies toward aggressive behavior and those with poor coping mechanisms regarding stress and impulse control. Substance abuse often plays a role in AHT. Despite these risk factors, abuse happens in families of all demographics, race, and economic circumstances.
When AHT Is Missed by a Healthcare Professional, What Are the Most Common Alternatively Entertained Diagnoses?
Accidental head trauma, viral gastroenteritis, influenza, and sepsis, amongst others.
How Often Is AHT Misdiagnosed by Healthcare Professionals?
In an important study by Jenny C. et al. (1999) the authors found that the diagnosis of AHT was not recognized in approximately one third of children with abusive head injuries who were seen by a physician. Approximately one third of those children sustained additional injuries after the missed diagnosis.
How Is the Nature of Injury Established in Cases of Suspected AHT?
Most commonly, a child with AHT is carefully examined and evaluated by a multidisciplinary team of professionals that work together in a coordinated and collaborative manner to determine whether abusive injury has occured. Occasionally the abuse is witnessed or the caretaker responsible for the inflicted injuries confesses to injuring the child. More commonly, however, the caretaker is not truthful about the inciting event. Evaluation of the cause of injury typically involves gathering information from the caretaker, family members, first responders, emergency department (ED) physicians, pediatricians, neurologists, ophthalmologists, neurosurgeons, radiologists, social workers, nurses, psychologists, psychiatrists, and law enforcement officers as appropriate and analyzing data provided by the physical examination, laboratory tests, imaging studies, and the scene investigation.
What Is the Composition of a Multidisciplinary Child Protection Team?
Depending on resources and geography, hospitals may have a multidisciplinary child protection team (CPT). CPTs typically consist of pediatricians whose clinical focus is child abuse (one or more of these pediatricians may be board-certified in the subspecialty of Child Abuse Pediatrics), social workers, nurses, psychologists, psychiatrists, and occasionally, attorneys. Team compositions may vary.
What Is the Role of the Radiologist in Evaluating Children With Suspected AHT?
The radiologist plays a critical role in the assessment of a child with head injury who may have been abused. First, the radiologist must attempt to determine whether the imaging abnormalities have been caused by trauma or by a medical condition or by both. A child with a medical condition may also have been abused and in fact, children with medical conditions are at greater risk for being abused than otherwise healthy children. Second, if it appears that the head findings are traumatic in nature, the radiologist should search for additional imaging abnormalities that may support or exclude abuse as the basis of the imaging abnormalities.
Based on the imaging abnormalities, it is helpful for the radiologist to provide recommendations for supplemental and/or follow-up imaging examinations that may further clarify and characterize the nature of the imaging findings. For example, if a radiologist identifies a SDH, on a head CT that is not explained by the medical condition of the child or by the history provided by the caretaker, the radiologist should discuss with the careteam whether obtaining a brain MRI as a next step would be helpful.
It is often informative for a radiologist to perform a comprehensive review of all imaging studies obtained during a care episode of a child being assessed for abuse to assess the evolution of imaging abnormalties on serial studies which often results in increased insight into the character of findings.
What Are the Potential Clinical Outcomes for Children With AHT?
An estimated 18 to 25% of children with AHT may not survive the traumatic incident, and it is estimated that 50% to 80% of survivors suffer significant long-term morbidity. Neurological outcomes include delayed psychomotor developent, behavioral disorders, learning and language/speech difficulties, hemi- and quadriparesis, epilepsy, visual impairment, severe physical and mental disabilities and a persistant vegetative state.
Imaging of AHT
Are There Imaging Patterns That Are Considered Particularly Suggestive of AHT?
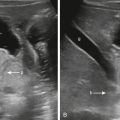
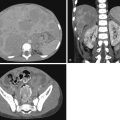
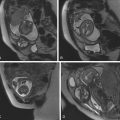
Imaging abnormalities vary based on the severity of the head injury. Findings include unilateral or bilateral SDHs, typically thin and extensive and located over the convexities and/or within the interhemispheric fissure, unilateral or bilateral parenchymal brain injury, typically hypoxic ischemic in nature, and retinal hemorrhages, which can be unilateral or bilateral ( Fig. 20.1 ). Bridging vein injury with partial or complete disruption of the bridging vein and cortical vein thrombosis may be apparent. A thin but extensive SDH with midline shift that is disproportionately greater than the width of the SDH (reflecting additional mass effect from ipsilateral brain swelling/injury) is particularly suggestive of AHT ( Fig. 20.2 ) and warrants further investigation for possible abuse. An unexplained intracranial SDH as an isolated imaging finding is nonspecific, but raises the possibility of AHT. The medical team will attempt to determine the underlying cause of the SDH (e.g., abusive injury, accidental trauma, benign enlargement of the subarachnoid space [BESS], coagulopathy, metabolic disorder and other conditions) and assess the child for signs of possible inflicted injury.


Skull fractures are present in approximately 25% of cases of AHT and provide evidence of impact/impulse injury. The incidence of skull fractures in AHT is greater in autopsy series and lower in children with AHT without neurological deficits. As approximately 75% of children with AHT will NOT have a skull fracture, identification of an occult skeletal fracture on a SS provides additional data supporting a history of trauma.
Skull Fractures
What Is the Most Common Type of Skull Fracture in AHT?
linear parietal skull fracture is the most common type of skull fracture seen in AHT ( Fig. 20.3 ). However, it is also the most common type of skull fracture observed in cases of accidental head trauma. Complex skull fractures (e.g., depressed, comminuted, diastatic, multiple, bilateral, and suture-crossing) without appropriate history are more suggestive of abusive injury ( Fig. 20.4 ).


Subdural and Epidural Hematomas
Please note that in this chapter a “subdural” hematoma/collection is referred to as blood and/or fluid located between the dura and the arachnoid membrane. On histologic examination these hematomas/collections are identified within the dura, within a cleavage plane in the dural border cell layer.
What Causes Subdural Hematomas in Children With AHT?
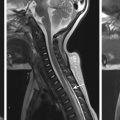
The most widely cited cause of SDHs in children with AHT is partial or complete tearing of bridging veins at the vertex. In AHT secondary to accelearation and deceleration forces, bridging veins are subjected to tension and stretching, which in turn can lead to tearing of a bridging vein and bleeding into the subdural and subarachnoid spaces ( Fig. 20.5 ). Occasionally a torn bridging vein with contracted clot at the point of disruption is observed on axial and/or coronal MRI as a discontinuous vein with an ovoid-, tadpole-, or comma-shaped configuration at the point of injury ( Fig. 20.6 ). There have been other alternative proposed theories for causes of subdural hemorrhage in AHT which have not been supported in the peer review literature.


What Is the Typical Appearance of a Subdural Hematoma in a Child With AHT?
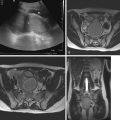
In children with AHT, SDHs are usually thin, unilateral or bilateral, heterogeneous in attenuation, and located over the convexities and/or within the interhemispheric fissure (see Figs. 20.1–20.3 and 20.6 ). SDHs may also be observed within the posterior fossa along the squamosal portions of the occipital bones and along the clivus (retroclival) (see Fig. 20.5 ). Posterior fossa SDHs are often small, best appreciated on MRI, and are easily overlooked on CT, especially as CT images may be hampered by streak artifact and volume averaging between subdural blood and the occipital bones. A SDH may contain a fluid–fluid level ( Figs. 20.7–20.9 ), which reflects the separation of blood components within the collection; sediment layers dependently and supernatant layers in a non dependent fashion. Fluid–fluid levels within SDHs are also observed in cases of accidental head trauma. Typically, fluid–fluid levels resolve on follow-up imaging due to mixing and redistribution of blood products within the subdural space (see Fig. 20.8 ).


How Do Hematohygromas Form?
The most widely held theory on the etiology of hematohygromas in children with AHT is that the trauma causes a tear or rent in the arachnoid membrane that allows cerebrospinal fluid (CSF) to flow from the subarachnoid space into the subdural space. If the subdural space also contains blood, a hematohygroma is formed. If blood is not present within the subdural space, a hy groma is formed. Additional theories posit that subdural hematohygromas arise from SDHs that accumulate CSF either through diffusion or effusion of CSF from the subarachnoid space into the subdural space, or that fluid accumulates within the subdural space from surrounding vessels. A hematohygroma may be indistinguishable from a hygroma based on the variable proportions of blood relative to CSF/fluid within the subdural space ( Fig. 20.10 ). Along these lines, a hematohygroma that contains a low concentration of CSF/fluid resembles a SDH. Serial imaging of children with AHT in the first week to week and a half after the onset of symptoms may show an increase in the size of a subdural collection (see Figs. 20.8 and 20.9 ), which can be caused by ongoing bleeding and/or influx or accumulation of CSF/fluid in the subdural space.