, Maria Custódia Machado Ribeiro2 and Bruno Beber Machado3
(1)
Hospital da Criança de Brasília – Jose Alencar, Clínica Vila Rica, Brazília, Brazil
(2)
Hospital da Criança de Brasília – Jose Alencar, Hospital de Base do Distrito Federal, Brasília, Brazil
(3)
Clínica Radiológica Med Imagem, Unimed Sul Capixaba, Santa Casa de Misericordia de, Cachoeiro de Itapemirim, Brazil
Abstract
The notion that children are not small adults is proverbial in medicine. This is also valid for osteoarticular trauma, as the immature musculoskeletal system responds to traumatic injuries differently from the adult organism. Lesions due to acute high-energy trauma, which are discussed in this chapter, differ from those caused by overuse/anomalous stress, such as the sports-related injuries studied in Chap. 10. Special emphasis will be put on articular injuries, although some extraarticular lesions typical of the pediatric age group are also described. In addition to accidental traumatic injuries, this chapter will also cover non-accidental trauma, given the importance of imaging as an objective evidence of child abuse. A concise approach will be used in the following topics, highlighting the imaging appearance of the most frequent lesions. Pediatric trauma is an extensive and complex issue and an in-depth study of it is beyond the scope of this brief review.
9.1 Introduction
The notion that children are not small adults is proverbial in medicine. This is also valid for osteoarticular trauma, as the immature musculoskeletal system responds to traumatic injuries differently from the adult organism. Lesions due to acute high-energy trauma, which are discussed in this chapter, differ from those caused by overuse/anomalous stress, such as the sports-related injuries studied in Chap. 10. Special emphasis will be put on articular injuries, although some extraarticular lesions typical of the pediatric age group are also described. In addition to accidental traumatic injuries, this chapter will also cover non-accidental trauma, given the importance of imaging as an objective evidence of child abuse. A concise approach will be used in the following topics, highlighting the imaging appearance of the most frequent lesions. Pediatric trauma is an extensive and complex issue and an in-depth study of it is beyond the scope of this brief review.
9.2 Peculiar Aspects of the Fractures of the Immature Skeleton
The most important difference between the immature skeleton and the adult organism is the presence of the physis, a specialized region located in the transition between the metaphysis and the epiphysis (see Chap. 2), which is most vulnerable in the provisional calcification zone. Because of its high collagen content, the immature bone is weaker than the adjacent ligaments and tendons, and traumatic lesions that would lead only to ligament injuries in adults may cause fractures in children. Nonetheless, the bones of children are more elastic than the undeformable bones of adults, so that pediatric fractures are less prone to propagation/comminution. As the periosteum is thicker, more active, and more resistant in children than in adults, there is speedy callus formation and prompt healing of fractures in the former.
Radiographs are indispensable in the initial assessment of a suspected fracture, and at least two orthogonal views are mandatory in order to describe the affected bone segments, the extent and the orientation of the fracture line, and the occasional presence of comminution, diastasis, angulation, or displacement (Figs. 9.1 and 9.2). The joints above and below the region of interest must be included in the radiographs, aiming to demonstrate physeal/intra-articular compromise or concomitant dislocation, which often go unnoticed. Indirect radiographic signs of fracture include displacement of periarticular fat planes (an indicator of joint effusion), irregularity of bone surfaces, abnormal alignment between the epiphysis, and the metaphysis and focal physeal widening (Fig. 9.3).




Fig. 9.1
Anteroposterior view (left) and lateral view (right) of the right ankle of a child with triplanar fracture. The first image shows a vertical fracture affecting the lateral portion of the distal epiphysis of the tibia and lateral physeal widening, which could be taken as a Salter-Harris fracture type III. Nonetheless, there is a bone fragment projected posterior and lateral to the distal metaphysis of the tibia, better seen in the lateral view, which demonstrates a coronal fracture of the metaphysis. Complex fractures like this one require CT for proper evaluation

Fig. 9.2
Lateral view of the left ankle demonstrating a type II fracture of the distal tibia with anterior displacement of the epiphysis and of the metaphyseal fragment. Marked osteoporosis is also present

Fig. 9.3
Radiographs of the left elbow of a child with supracondylar fracture of the humerus. Although the fracture line is quite subtle in the anteroposterior view, additional markers seen on the lateral view include displacement of the anterior and posterior fat planes and absent intersection between the anterior humeral line and the central portion of the distal epiphysis
Computed tomography (CT), magnetic resonance imaging (MRI), and ultrasonography (US) are usually electively performed, as a second line of investigation. CT is very useful in diagnosing and staging fractures, especially in patients with inconclusive radiographs or in regions of complex anatomy, being also helpful in the assessment of late complications (Fig. 9.4). MRI is very suitable to evaluate soft-tissue structures and to evidence the presence of bone marrow edema pattern, a reliable marker of bone alterations that may herald “hidden” fractures (Figs. 9.5 and 9.6). Because of its appropriateness for the study of the non-ossified cartilage, MRI is also valuable in the evaluation of physeal fractures and in the assessment of joint dislocations in small children (Fig. 9.7). Bone scintigraphy has high sensitivity in the detection of fractures, being able to evaluate the whole skeleton in a single study; the latter feature is especially useful in the screening of fractures, such as those found in polytraumatized or physically abused children. However, because of its low specificity and limited spatial resolution, most areas of abnormal uptake demand additional investigation in order to determine their real nature. US is more adequate for the assessment of soft-tissue abnormalities associated with fractures, such as joint effusion, periosteal detachment, and periarticular fluid collections. In addition, fractures of the non-ossified portions of the ossification centers (which are undetectable on radiographs) may be diagnosed with US (Fig. 9.8).


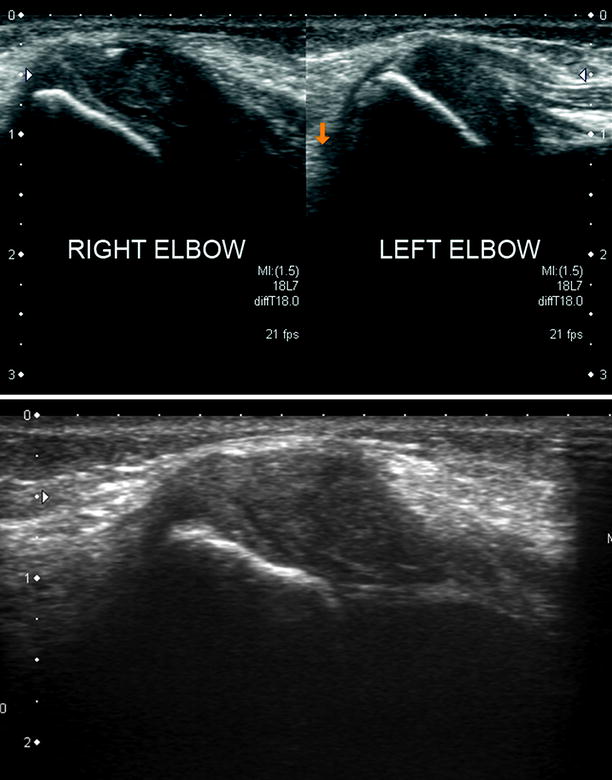
Fig. 9.4
Reformatted CT images in the coronal (a) and sagittal (b) planes of the distal humerus of a 9-year-old child show a healed transphyseal fracture (type IV) of the lateral condyle. There is a bony bridge between the humeral metaphysis and the anteromedial portion of the capitulum, more evident in (b). Premature osteoarthritis is also present

Fig. 9.5
In (a), sagittal fat sat T2-WI of the ankles (right, upper row; left, lower row) allows for clear demonstration of widening and increased signal intensity of the left tibial physis, as well as homolateral periphyseal edema. This acute, non-displaced Salter-Harris type I fracture would be difficult to detect with other imaging methods. Although similar findings are present in (b) (coronal fat sat PD-WI (left) and sagittal T1-WI (right) of the right knee of a 12-year-old child), bone marrow edema is less prominent and physeal widening is more evident, as this is a subacute lesion

Fig. 9.6
T1-WI (left) and fat sat T2-WI (right) of the left knee show subtle lateral displacement of the proximal epiphysis of the fibula, more evident in the coronal images (Salter-Harris lesion type I), with bone marrow edema pattern centered at the physis. There is also extensive edema in the adjacent muscles and a subperiosteal hematoma along the proximal metadiaphysis of the fibula
Fig. 9.7
In (a), radiographs of the left elbow demonstrate a fracture line involving the lateral condyle of the humerus, extending from the lateral cortex of the metaphysis to the physis, medial to the ossification center of the capitulum, which is already mineralized. Nonetheless, radiographs do not allow proper assessment of the extension of the fracture into the non-ossified portion of the epiphysis. Coronal T1-WI (b) is also limited to demonstrate the real extent of the fracture, which is clearly shown on fat sat PD-WI (c) (Salter-Harris fracture type IV). Joint effusion and marked edema of the periarticular soft tissues are also present
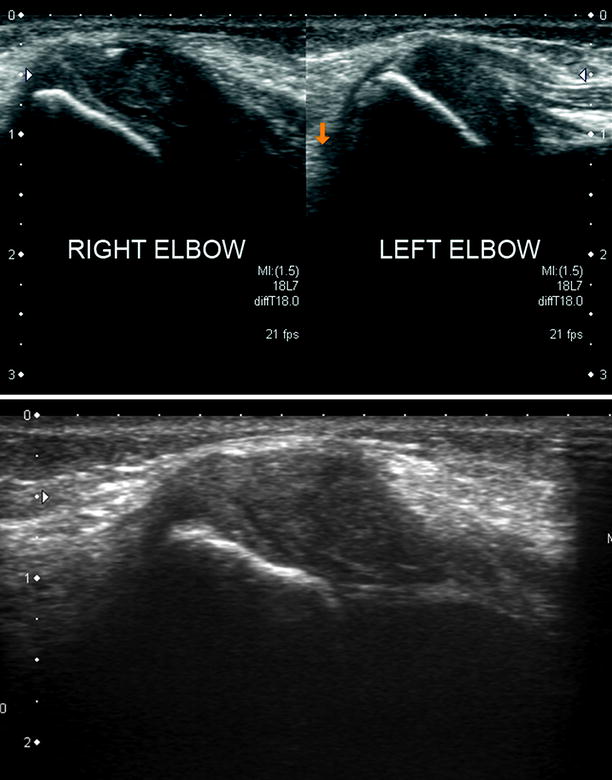
Fig. 9.8
US of a very young child with right-sided avulsion fracture of the non-ossified medial epicondyle of the humerus. The upper image shows caudal displacement of the avulsed epicondyle, with hypoechogenic fluid interposed between the fragment and the host cartilage (compare with the normal appearance of the left medial epicondyle). In addition to the above-described avulsion fracture, the lower image also discloses a subtle zigzag hypoechogenic fracture line coursing transversely through the cartilaginous fragment
Pediatric fractures may be divided in physeal and non-physeal. Physeal fractures, the main subject of this topic, only occur in the immature skeleton, accounting for 10–30 % of all fractures in children; they raise particular interest because of its potential to cause joint damage and abnormal bone growth. The Salter-Harris classification system is the most widely used, dividing the fractures into five groups according to their location and type of damage to the growth plate, each one of them with distinct prognostic and therapeutic implications (Fig. 9.9). Type I fractures course transversely through the growth cartilage, with no epiphyseal or metaphyseal extension, leading to physeal widening or epiphyseal dislocation (Figs. 9.5, 9.6, and 9.10). Type II fractures are the most common (75 % of all cases), involving the peripheral portion of the metaphysis and part of the growth plate, creating a bone fragment that includes the whole epiphysis and a portion of the metaphysis (Figs. 9.2 and 9.11). Type III lesions are intra-articular fractures that involve the epiphysis and the physis: the fracture line begins in the articular surface, crosses the epiphysis, and presents a transverse component coursing through the peripheral portion of the physis, creating an epiphyseal fragment without connection with the metaphysis (Figs. 9.12 and 9.13). Type IV lesions cross the metaphysis and the epiphysis, transecting the physis and the joint surface, therefore producing a bone fragment that includes epiphyseal and metaphyseal components (Fig. 9.7). Type V lesions are the rarest of all (approximately 1 %) and are difficult to diagnose, being caused by axial compressive forces that lead to crushing injury of the physis, without obvious epiphyseal or metaphyseal fractures; radiographs are usually normal or display subtle physeal narrowing. Diagnosis of type V lesions is most often late and retrospective, made after the appearance of complications, such as growth arrest. Generally speaking, type I and type II lesions present good evolution because they do not involve the joint surfaces (Fig. 9.14), while intra-articular lesions (types III and IV) have worse prognosis, with increased risk of secondary osteoarthritis and functional limitation (Figs. 9.4, 9.15, 9.16, and 9.17). Fractures that involve the physis may lead to development of transphyseal bone bridges and/or early physeal closure (Figs. 9.4, 9.16, 9.17, and 9.18). Both MRI and CT are useful in the demonstration of physeal bridges (Fig. 9.4): when centrally located, they tend to cause limb-length discrepancy, while peripheral bridges cause localized growth arrest and angular deformities. In addition to limb shortening, bone bridges may cause damage to the adjacent joints, as well as bowing of the forearm or of the leg if only one of the paired bones is affected (Fig. 9.16). Growth recovery lines that are angled or obliquely oriented – instead of parallel – relative to the physis are indicative of disturbed bone growth related to the presence of bone bars (Fig. 9.16).
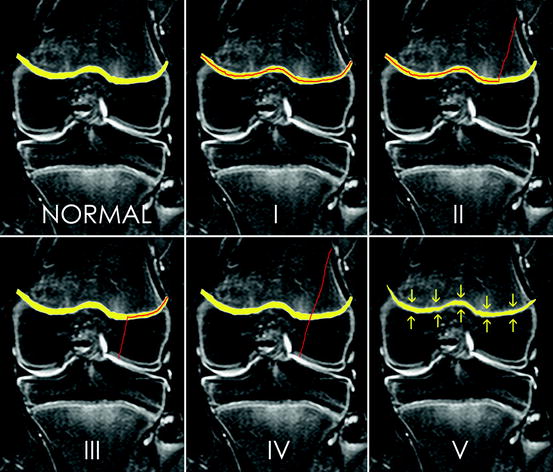
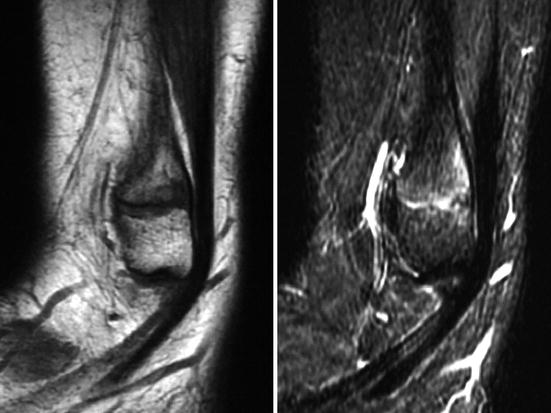


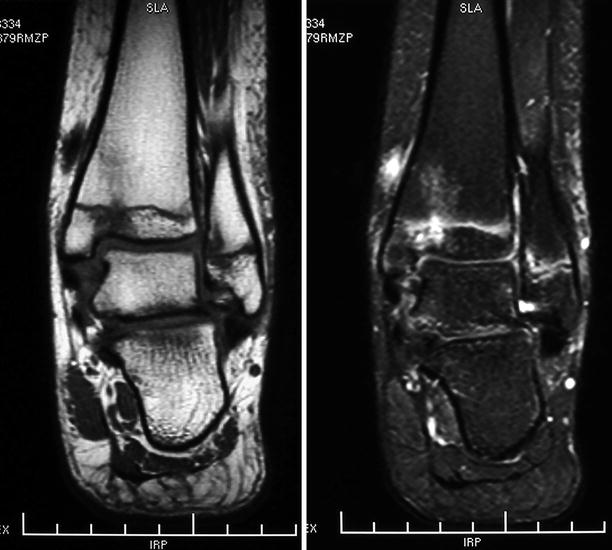




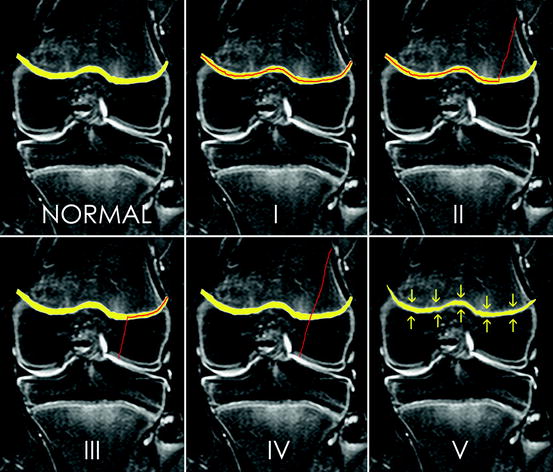
Fig. 9.9
Schematic representation of the Salter-Harris classification for physeal fractures. The physis is represented in yellow and the fracture lines appear in red. While types I and II are physeal and physeal/metaphyseal, respectively, types III and IV are associated with epiphyseal involvement and extend to the joint surface. Type V fracture is a compressive physeal lesion, resulting from the action of axial forces
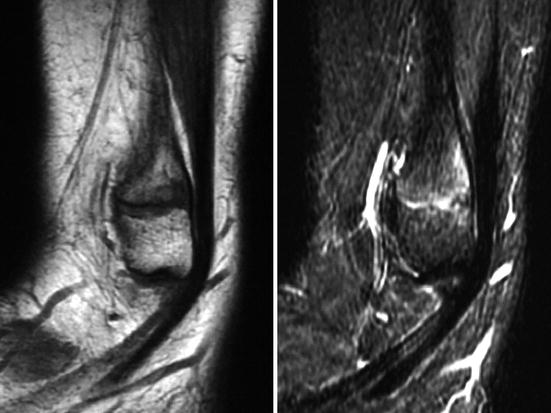
Fig. 9.10
Sagittal T1-WI (left) and fat sat T2-WI (right) of the right ankle. There is widening of the physis of the distal fibula, more evident on T1-WI, with edematous changes of the physis itself and of the adjacent bone marrow on fat sat T2-WI (Salter-Harris fracture type I)

Fig. 9.11
Lateral (left image) and oblique (right image) views of the wrist disclosing a physeal/metaphyseal fracture of the distal radius, with dorsal angulation and displacement of the epiphysis and of the metaphyseal fragment

Fig. 9.12
Type III fracture of the base of the proximal phalanx of the thumb in a 14-year-old male. Radiograph (a), coronal T1-WI (b, upper row), and sagittal fat sat PD-WI (b, lower row) show a mildly displaced physeal/epiphyseal fracture leading to discontinuity of the joint surface
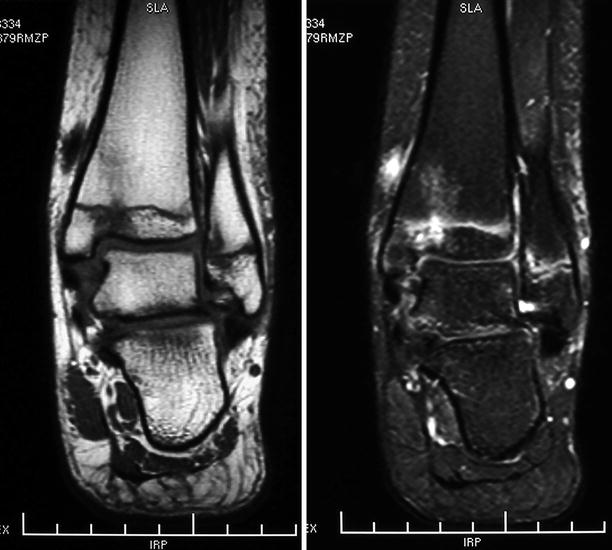
Fig. 9.13
Coronal T1-WI (left) and fat sat PD-WI (right) of the left ankle of a 12-year-old female demonstrate periphyseal bone marrow edema in the tibia and in the fibula, with a vertical fracture line extending to the joint surface in the medial portion of the tibial epiphysis, also surrounded by marrow edema. These findings are compatible with Salter-Harris fractures type III in the tibia and type I in the fibula

Fig. 9.14
Evolution a type II fracture of the distal femur treated with surgical fixation. Formation of bone callus and progressive healing of the fracture are evident in serial radiographs, with gradual onset of osteoporosis
Fig. 9.15
Radiographs (a), sagittal reformatted CT images (b), and volume-rendered reconstructions (c) of an adolescent with sequelae of a surgically corrected elbow fracture. There is irregularity of the joint surfaces, with early-onset osteoarthritis and flexion deformity

Fig. 9.16
In the left image, radiograph of the wrist and of the forearm of a skeletally immature patient demonstrates bowing and residual deformity of the radius and of the ulna, with orthopedic plate and screws in the distal ulna. A peripheral transphyseal bone bridge is seen in the distal radius (to which growth recovery lines converge), as well as incongruity of the radiocarpal joint. At right, radiograph of a young adult with sequelae from an old healed fracture of the distal forearm reveals radial shortening (growth arrest related to physeal injury) and premature osteoarthritis of the wrist, as well as deformity of the distal ulna

Fig. 9.17
Old gunshot injury in the head of the fourth metacarpal bone associated with physeal lesion. There is deformity of the metacarpal head and premature physeal closure leading to bone shortening

Fig. 9.18
Radiographs of the right wrist and distal forearm of a child with old healed fractures of the homolateral radius and ulna. There is discrepancy in the length of the forearm bones due to early closure of the ulnar physis and, as a consequence, ulnar shortening. Secondary deformity of the distal radius is also present
Some incomplete non-physeal fractures – more frequently found in the distal third of the forearm – will be briefly described as they are typical of the pediatric group. The greenstick fracture is characterized by an incomplete cortical break in the convex edge of the bone and cortical bowing in the concave border, with periosteal apposition that creates a hinge-like effect (Figs. 9.19 and 9.20). Almost one-third of the patients with greenstick fractures will present refractures (which may occur in other types of fracture as well) due to incomplete and/or asymmetric healing (Fig. 9.21). Buckle (torus) fractures present as a subtle cortical irregularity with bulging of the bone surface, typically located adjacent to the metaphyses (Fig. 9.22). The plastic deformation is just an accentuation of the physiological bowing of the affected bone, with no discernible fracture line on radiographs (Figs. 9.21 and 9.23); it is not infrequent for plastic deformation to be associated with other fractures (Fig. 9.21).