Acetabular Fractures
The acetabulum is a socket of bone formed from the fusion of the ilium, ischium, and pubis at the triradiate cartilage. It articulates with the femoral head in a highly constrained joint. Judet and colleagues1 and Letournel2 defined the socket as being supported from the sciatic buttress by two columns of bone: the anterior column (made up of the ilium and pubis) and the posterior column (made up of the ischium) (Fig. 23.1). Fractures of the acetabulum that are displaced and result in a loss of congruence between the femoral head and the remaining intact portion of the superior articular surface typically have a poor prognosis. When such injuries are treated surgically, hip joint preservation and maintenance of hip function typically result if operative complications are avoided.3–6 Increased experience with the treatment of these types of injuries improves the treating physician′s ability to correctly evaluate radiographs, determine the appropriate surgical approach, perform adequate reductions, and understand the impact of associated injuries on treatment. Due to the relative rarity of acetabular fractures and their typically higher energy mechanisms, treatment of these injuries is ideally performed by surgeons with advanced training working at specialized hospitals that focus on the care of multiply injured patients. However, all orthopaedic surgeons should be comfortable with the diagnosis and initial management of these injuries. Because the initial management of ace-tabular fractures often impacts their definitive treatment, optimum initial treatment requires some knowledge of the eventual management of the injury as well.

The initial radiographic evaluation of an acetabular fracture typically includes an anteroposterior (AP) X-ray of the pelvis obtained in a patient complaining of inguinal (“groin”) or lateral hip pain following injury or as part of a trauma imaging protocol in a multiply injured or obtunded patient. From this initial radiograph, fractures involving the acetabulum are usually identified by evaluating the six radiographic “lines” (see text box) as described by Judet and colleagues and Letournel and Judet6 (Fig. 23.2). Although not specific anatomic structures, these lines represent areas of bone tangent to the radiographic beam and define the supporting columns or walls of the acetabulum. Thorough assessment of these lines is a critical step toward understanding the two-dimensional radiographic representation of the complex three-dimensional innominate bone. Additionally, the AP pelvis radiograph facilitates comparison with the contralateral normal hip to determine if there is a change in the relationship of the femoral head to the “radiographic roof.” When reviewing an AP radiograph of the pelvis, the coccyx and the pubic symphysis should align with one another on the intact side of the pelvis. If they do not, the image is malrotated, and this fact should be considered when assessing any deformity of the pelvis.

Although some fractures of the acetabulum are obvious and associated with wide displacement of the bone, subluxation, or dislocations of the femoral head, others are associated with less displacement evident on the AP pelvic radiograph. Oblique radiographs or Judet views, taken with the patient rolled 45 degrees in either direction, enable orthogonal evaluation of the innominate bone (Fig. 23.3). The easier of the views to obtain is the obturator oblique view because the patient is rotated off the affected side. Named because it profiles the obturator ring, this view enables evaluation of the anterior column, posterior wall, and ischial ramus. It is an important film in the evaluation of a patient with a high-energy mechanism, groin pain, and no obvious finding on the AP pelvic radiograph. It nicely depicts subtle fractures of the posterior wall, femoral neck, or femoral head. The opposite iliac oblique view is commonly inadequately rotated due to the need for positioning the patient partially on the injured side. This view is used to evaluate the posterior column, anterior wall, and iliac wing. Sufficient pain control is mandatory to obtain radiographs with adequate rotation that will provide reliable information. Adequate rotation is usually present on the radiographs when the medial extent of the femoral head meets the tip of the coccyx. When standard Judet views are inadequate or cannot be obtained, corresponding computed tomography (CT) reconstructed Judet images can be reconstructed from axial CT data.7

Classification
A systematic approach to evaluating the plain radiographs can reliably result in the appropriate diagnosis of the injury to the bone. The importance of this lies in the subsequent treatment decisions for the patient. Based on the radiographic analysis of cadaveric bone and injury films, Judet and colleagues1 and Letournel2 developed a classification system for fractures of the acetabulum. Their classification consists of five elementary and five associated fracture patterns (see text box), and accounts for transitional forms (Fig. 23.4).

The Letournel classification is not only descriptive in nature; its primary importance lies in its ability to direct the most appropriate surgical approach to the acetabulum.2–4,6 Accurate radiographic diagnosis of the injury will enable the surgeon to determine the best surgical approach and improve the chances of achieving an adequate reduction.
The Six Acetabular Lines Visible on an Anteroposterior Hip Radiograph
Iliopectineal line
Ilioischial line
Radiographic teardrop
Radiographic roof
Anterior wall
Posterior wall
The Acetabular Fracture Classification of Letournel and Judet
Elementary patterns
Posterior wall
Posterior column
Anterior wall
Anterior column
Transverse
Associated patterns
Posterior column/posterior wall
Transverse/posterior wall
T-shaped
Anterior column (wall)/posterior hemitransverse
Associated with both columns
This chapter assumes that the reader has a working knowledge of the Letournel classification, which is thoroughly discussed in the classic book by Letournel and Judet.6 A concise yet thorough description of the classification and surgical approaches has also been written by Letournel.2 However, the following fundamental aspects of the Letournel classification system are important to review6,8:
The five elementary acetabular fracture patterns are “elementary” secondary to the “purity” of the fracture line.
Classification of an acetabular fracture is relatively reproducible from one surgeon to another. However, there are transitional fractures that do not fall neatly into one category, particularly fractures that fall between a T-shaped, anterior column/posterior hemitransverse, and a both-column fracture.
Column fractures separate an entire column from the innominate bone, whereas wall fractures separate only a portion of the articular surface. Column fractures have a fracture line that enters the obturator foramen and a fracture in the ischiopubic (inferior) ramus.
Anterior column fractures can exit the anterior aspect of the innominate bone either at a high (iliac crest), intermediate (anterior superior iliac spine), low (psoas gutter at the level of the anterior inferior iliac spine), or very low pectineal eminence) position.
Anterior column fractures commonly involve a portion of the quadrilateral surface. This feature, combined with the typical external rotation of the anterior column, enables medialization of the femoral head to occur.
Transverse acetabular fractures involve both columns of the innominate bone. However, they are not described as both-column fractures, which is instead a term that applies to a specific type of associated fracture. Transverse acetabular fractures are an elementary fracture secondary to the purity of the fracture line. They separate a portion of the superior innominate bone with a portion of the dome from the lower ischiopubic segment. The ischiopubic segment rotates in two ways. First, it rotates around a vertical axis passing through the pubic symphysis, which makes the acetabulum appear to be displaced inward. Second, a rotation occurs about a horizontal axis from the posterior aspect of the fracture to the pubic symphysis. Transverse fractures can be classified further with regard to where they involve the articular surface of the dome: through the roof (transtectal), through the high point of the cotyloid fossa (juxtatectal), and through the cotyloid fossa and involving the inferior portions of the anterior and posterior walls (infratectal).
Fractures that involve the iliac crest are anterior column, anterior column/posterior hemitransverse fractures, and both-column fractures.
Anterior column/posterior hemitransverse fractures may be thought of as a combination of an anterior column fracture with the posterior half of a transverse fracture. The posterior column fracture tends to be low and minimally displaced. This is in distinction to posterior column involvement in associated both-column fractures.
Elderly patients with low-energy falls tend to have anterior column or anterior column/posterior hemitransverse acetabular fractures. Both fractures can have quadrilateral surface involvement (Fig. 23.5), medial articular dome impaction (“gull wing sign”) (Fig. 23.6), or posterior wall impaction.
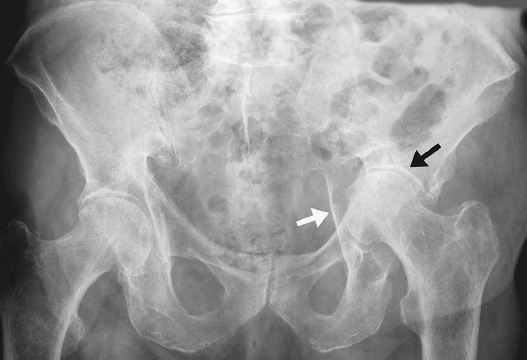
The associated both-column fracture has a distinguishing feature of having no portion of the articular dome in continuity with the intact ilium (Fig. 23.7). In addition, there is a fracture line separating the anterior column (which itself has been separated from the intact ilium) and the posterior column. The femoral head usually medializes, the anterior column externally rotates, and the posterior column internally rotates. The labrum usually remains intact to all the fragments, and thus the femoral head remains congruent to the acetabulum, which is termed secondary congruence. The radiographic “spur sign,” if present, is pathognomonic for an associated both-column fracture. It is best seen on the obturator oblique view and represents the outer aspect of the inferior aspect of the innominate bone, which is separated from the articular dome fragments.

Beaulé et al8 have confirmed that the Letournel classification has significant interobserver and intraobserver reliability among surgeons involved in a high volume of acetabular fracture surgeries per year (> 40 cases/year). CT scans have not proven helpful in determining the classification of the acetabular fracture. However, CT does provide valuable information regarding the number of fracture fragments (comminution), the orientation of the fracture lines, the displacement of the fracture, the direction and rotation of fracture displacement, and whether there is marginal impaction or incarcerated fragments in the hip joint. The CT scan is therefore essential for appropriate preoperative planning.
Whether a fracture line and its displacement may have an impact on the eventual outcome of the hip joint is likely determined by the fracture location, the amount of displacement, and its effect on hip joint stability. Initially it was recognized that fractures involving the superior articular surface had an increased risk of posttraumatic arthrosis. Matta et al9 subsequently attempted to define the superior articular surface using roof arc angles. These angles are defined by a vertical line drawn through the center of the femoral head and another from the center of the femoral head to the point where the fracture enters the articular surface on each of the three pelvic radiographs, with the leg out of traction (Fig. 23.8).

Measurement of roof arc angles requires that the femoral head is not subluxed, and these arcs cannot be used to evaluate either the both-column fracture pattern (because usually the acetabulum medializes along with the subluxed femoral head, referred to as secondary congruency) or posterior wall fractures (because these fractures rarely disrupt the superior articular surface on any view). Although the precise definition has changed since the initial publications, currently a fracture is deemed to be within the superior articular surface if it enters the joint at an angle less than 45 degrees. Using a mathematical model, this definition has been extrapolated to CT, where if a fracture line enters the articular surface in a CT cut less than 1 cm from the cranial subchondral condensation of the acetabulum, it involves the weight-bearing dome.10
Vrahas et al11 provided an objective measure of the fractures’ impact on stability using a cadaveric model. Fractures of the anterior column entering above the anterior inferior iliac spine (obturator oblique roof arc angle of ~ 30 degrees) and fractures of the posterior column entering above the ischial spine (iliac oblique roof arc of ~ 70 degrees) resulted in femoral head subluxation in a single-leg stance model. This possibly demonstrates a greater relative importance of the posterior column to stability. This is likely due to the inclination of the pelvis and the relatively posterior vector of force to the hip during simulated single-leg stance. This may have implications regarding fracture stability and safe hip range of motion arcs during subsequent treatment.
Fractures that involve the superior aspect of the articular dome have been shown in cadaveric testing to be associated with altered contact pressures in several situations.12 Step malreduction of a transtectal (high) transverse acetabular fracture resulted in increased peak contact pressures in the superior acetabular articular surface, as shown by pressure-sensitive film in cadaveric testing. Gap malreductions of a transtectal transverse fracture and gap and step malreductions of a juxtatectal transverse fracture did not result in increased contact pressures in the hip. This information, along with the amount of fracture displacement, may have clinical importance in determining the likelihood of arthritis in operatively or nonoperatively treated acetabular fractures.
Nonoperative Treatment
Nonoperative treatment of acetabular fractures is currently indicated for the following types:
Fractures that do not involve the weight-bearing articular surface as defined by roof arc angles on plain radiographs or by CT
Fractures that are displaced less than 2 mm within the superior articular surface and maintain congruence between the femoral head and acetabulum with the involved leg out of traction
Fractures of the posterior wall with less than 20% involvement of the articular surface and no incarcerated fragments
Fractures that have secondary congruence following an associated both-column fracture
Due to the changes in articular stress patterns seen with concentric both-column fractures and the associated medialization of the joint, it is recommended that the majority of both-column fractures should be surgically treated unless medically contraindicated. Fractures with minimal displacement are at times difficult to classify, but if the displacement is truly minimal and the femoral head is concentrically reduced, classification of the fracture serves little purpose. If possible, with respect to associated injuries, these patients should be mobilized with 30-lb (10- to 15-kg) weight bearing on the affected limb as soon as possible. The authors do not recommend routine stress evaluation of the acetabulum unless the injury pattern includes a marginal-size posterior wall fragment in a cephalad location or if the acetabular fracture is associated with a contiguous injury to the pelvic ring. Adherence to these selection criteria may enable successful nonoperative treatment of certain fractures. Additionally, a nonoperative course of treatment may be necessary if surgical treatment is contraindicated due to a patient′s medical condition, preexisting arthrosis within the joint, severe comminution, poor bone quality, skin lesions over the proposed incision, or infection.
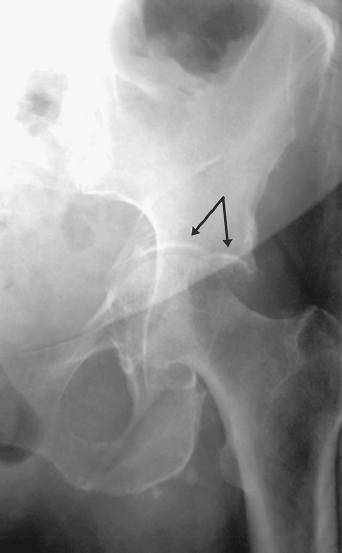
The surgeon must exercise caution when treating a posterior wall fracture nonoperatively. The location as well as the size of the fracture must be considered. Fractures involving less than 20% of the articular surface may still cause instability of the hip, especially if the fracture is involving the superior aspect of the posterior wall (Fig. 23.9). If a question remains regarding subtle instability of the hip joint following initial radiographic evaluation, dynamic stress views can be used to further evaluate. Tornetta13 described the use of dynamic stress views in fractures that met nonoperative criteria to demonstrate the ability of the femoral head to maintain congruence with the acetabulum prior to patient mobilization. He defined nonoperative criteria as roof arc measurements in all three acetabular views > 45 degrees, a subchondral CT arc of 10 mm, displacement of less than 50% of the posterior wall, and congruence on all three acetabular views. Forty-one patients with fractures underwent dynamic stress views to assess the loss of congruency between the femoral head and the acetabular roof. The mean displacement of the fractures was 7 mm. In 12 patients, the dynamic fluoroscopic stress views showed some movement of the displaced fragments, but the congruency was altered in only three (one transverse fracture—also with an associated pubic diastasis; two posterior wall fractures). These three patients underwent operative fixation, and the other 38 patients were treated nonoperatively. The results were good or excellent in 91% of the patients treated nonoperatively.

Surgical Treatment
Indications
Surgical treatment of acetabular fractures provides both short- and long-term benefits. The short-term benefits are associated with stable reconstruction of the joint to facilitate early mobilization of the patient. The long-term benefit is the avoidance or delayed onset of posttraumatic arthrosis, thereby preserving the function of the hip joint for many years to come. Such benefits are realized in the majority of surgically treated acetabulum fractures as long as complications can be avoided.3,4,14 Surgery is indicated for all acetabulum fractures that result in subluxation of the femoral head or loss of congruence with the acetabular articular surface. This can occur secondary to fracture displacement or retained fragments within the joint. If the hip remains concentric, but the fracture involves the superior articular surface and is displaced greater than 2 mm, surgical treatment should be strongly considered. In this circumstance, patient factors must be taken into account to individualize treatment. For example, surgery is more likely to be considered in a 20-year-old with an isolated injury than in a debilitated, minimally functional person of advanced age. If surgery on the acetabulum is contemplated, the fracture pattern and the impact that any associated injuries may have on treatment should be thoroughly understood. The surgeon must have sufficient experience in caring for this type of injury, an appropriate surgical team should be available, and the patient must be stable enough to undergo operative intervention. If any of these conditions are not met, then the surgery should be delayed or the patient should be transferred to a center that has surgeons with subspecialty training in this area.
Surviving the Night
Patients with an acetabular fracture associated with a femoral head dislocation should be urgently reduced within hours, as described in Chapter 22. This can either be done in the emergency room under conscious sedation or under general anesthesia in the operating room (depending on the institution). Occasionally, it may not be possible to obtain or maintain a reduction. Inability to obtain a closed reduction may be because the femoral head has button-holed through the posterior capsule or between the piriformis and obturator internus. It may also be because a posterior wall fracture fragment is blocking the reduction of the femoral head. Inability to maintain a closed reduction is most commonly due to a very large posterior wall fracture. If it is not possible to perform a closed reduction, an open reduction and internal fixation of the acetabular fracture/dislocation should be performed. There is some urgency to complete this within 6 to 18 hours of the injury. However, if the surgeon is not comfortable and familiar with acetabular fracture surgery, it is more prudent to wait until such a surgeon is available or the patient can be transferred to such a surgeon.
Not all acetabular fractures need to have skeletal traction placed through a distal femoral traction pin. Relatively clear-cut indications for skeletal traction include the following:
An anterior column, anterior column posterior hemitransverse, or an associated both-column fracture in which the femoral head is significantly medialized
A transverse, transverse with posterior wall, or T-type fracture in which the femoral head may be riding on the raw cancellous bone of the inferior portion of the intact ilium
A fracture in which there is an isolated osteochondral fragment between the superior aspect of the femoral head and the intact superior dome of the acetabulum
In addition, skeletal traction combined with leg abduction may be beneficial in patients with a large posterior wall acetabular fragment that renders the hip joint possibly unstable.
It is well recognized that pelvic fractures have the potential for significant blood loss. The surgeon on call must also be aware that acetabular fractures can also be associated with dramatic blood loss, and thus these patients should undergo aggressive fluid resuscitation and blood replacement therapy if necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree