Acquired Disease of the Thoracic Aorta and Great Vessels
QUESTIONS
1 What is the most common cause of an ascending thoracic aortic aneurysm?
A. Atherosclerosis
B. Aortitis
C. Marfan syndrome
D. Aortic stenosis
View Answer
1 Answer A. Most common cause of aortic aneurysm is atherosclerosis and accounts for approximately 70% of cases. The other answer choices are all less common causes of ascending thoracic aortic aneurysm.
Reference: Agarwal PP, Chughtai A, Matzinger FR, et al. Multidetector CT of thoracic aortic aneurysms. Radiographics 2009;29(2):537-552. doi: 10.1148/rg.292075080. Review. PubMed PMID: 19325064.
A. Atherosclerosis
B. Marfan syndrome
C. Bicuspid aortopathy
D. Hypertension
View Answer
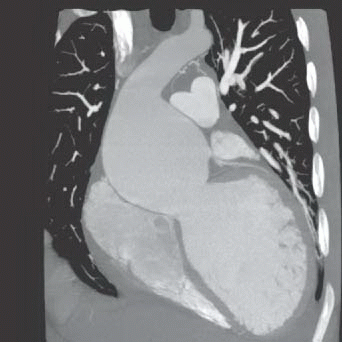
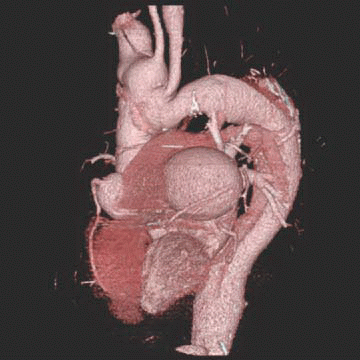
2a Answer B. Coronal reformatted image shows annuloaortic ectasia (effacement of the sinotubular junction with dilated aortic root). Some have described this as a “pear-shaped/tulip bulb” appearance of the aorta. While atherosclerosis is the most common cause of aortic aneurysm, there does not appear to be atherosclerosis in this young patient. Bicuspid aortopathy can also cause aneurysm but does not typically give this classic appearance of annuloaortic ectasia. The appearance of aortic aneurysm caused by hypertension will also typically not involve annuloaortic ectasia.
References: Agarwal PP, Chughtai A, Matzinger FR, et al. Multidetector CT of thoracic aortic aneurysms. Radiographics 2009;29(2):537-552. doi: 10.1148/rg.292075080. Review. PubMed PMID: 19325064.
Ha HI, Seo JB, Lee SH, et al. Imaging of Marfan syndrome: multisystemic manifestations. Radiographics 2007;27(4):989-1004. Review. PubMed PMID: 17620463.
2b In patients with Marfan syndrome, what associated valvular abnormality can be seen?
A. Tricuspid stenosis
B. Tricuspid valve prolapse
C. Mitral stenosis
D. Mitral valve prolapse
View Answer
2b Answer D. Mitral valve prolapse can be seen with Marfan syndrome. The other valvular abnormalities listed are not associated with Marfan syndrome.
References: Agarwal PP, Chughtai A, Matzinger FR, et al. Multidetector CT of thoracic aortic aneurysms. Radiographics 2009;29(2):537-552. doi: 10.1148/rg.292075080. Review. PubMed PMID: 19325064.
Ha HI, Seo JB, Lee SH, et al. Imaging of Marfan syndrome: multisystemic manifestations. Radiographics 2007;27(4):989-1004. Review. PubMed PMID: 17620463.
A. Aortic wall outer continuity
B. Smooth margins
C. Location at aortic isthmus
D. Intimal flap
E. Calcification
View Answer
3 Answer D. Classic ductus diverticulum features include smooth margins and gently sloping shoulders. It should form obtuse angles with the preserved aortic wall. There should not be an intimal flap; that would favor traumatic pseudoaneurysm. They can both be located at the aortic isthmus so that will not be a differentiating feature. Calcification can also occur in both chronic pseudoaneurysm and ductus diverticulum.
Reference: Steenburg SD, Ravenel JG, Ikonomidis JS, et al. Acute traumatic aortic injury: imaging evaluation and management. Radiology 2008;248(3):748-762. doi: 10.1148/radiol.2483071416. Review. PubMed PMID: 18710974.
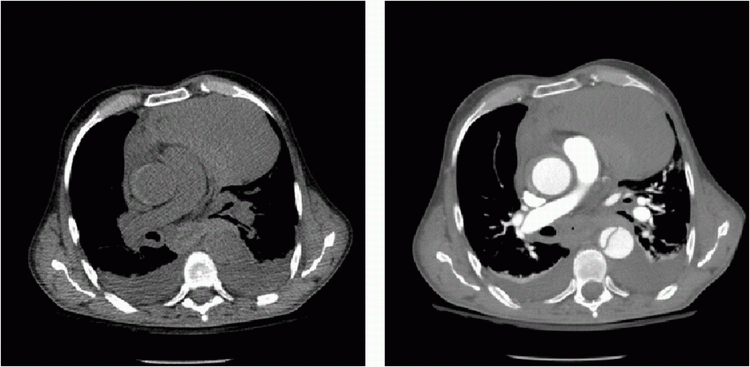
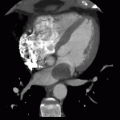
4 A 57-year-old female presents with chest pain. These images were obtained 4 months apart. What is the most likely cause of this aneurysm?
|
A. Atherosclerotic
B. Takayasu aortitis
C. Posttraumatic
D. Mycotic
View Answer
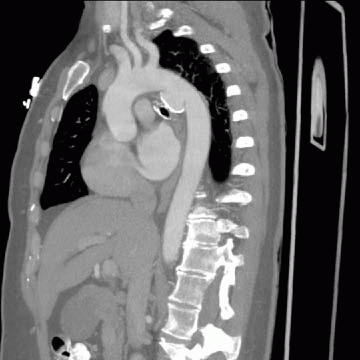
4 Answer D. The rapid progression of the aneurysm is most consistent with mycotic aneurysm. Atherosclerosis would not be this rapid in course. Saccular type of aneurysm seen here is also more common in mycotic aneurysms. Takayasu arteritis typically causes narrowing but can also cause aneurysm; in this case, it could be in the differential but is considered a less likely cause. Posttraumatic aneurysm is also possible, but the rapid enlargement and irregular borders are more consistent with mycotic than posttraumatic aneurysm.
References: Agarwal PP, Chughtai A, Matzinger FR, et al. Multidetector CT of thoracic aortic aneurysms. Radiographics 2009;29(2):537-552. doi: 10.1148/rg.292075080. Review. PubMed PMID: 19325064.
Macedo TA, Stanson AW, Oderich GS, et al. Infected aortic aneurysms: imaging findings. Radiology 2004;231(1):250-257. Erratum in: Radiology 2006;238(3):1078. PubMed PMID: 15068950.
A. Medical treatment
B. Gated CTA chest
C. Immediate surgery
D. Endovascular treatment
View Answer
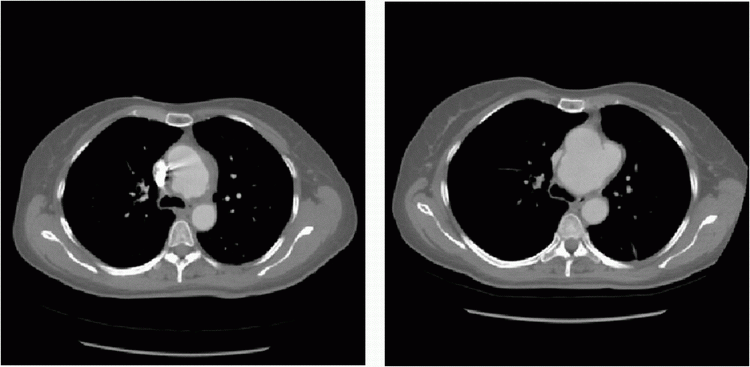
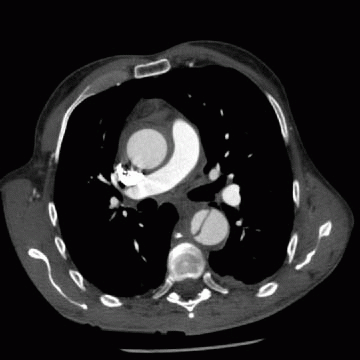
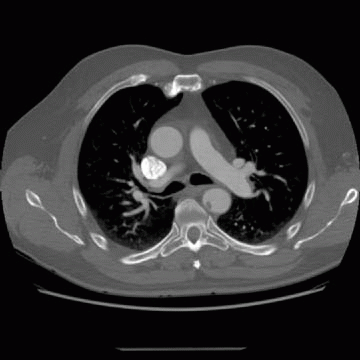
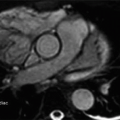
5a Answer B. Single-axial image shows a type B dissection in the descending thoracic aorta. There is suggestion of wall thickening at the aortic root, but this may be due to motion artifacts. The best next step would be a gated CTA chest to assess the aortic root better. Medical treatment would be fine if this were only an isolated descending thoracic dissection. Immediate surgery would be indicated if a type A dissection is confirmed (difficult to be certain given this may be motion artifacts on a nongated image). Endovascular treatment is not indicated given that there is no evidence for aneurysm and there is no role for endovascular treatment in type A dissections.
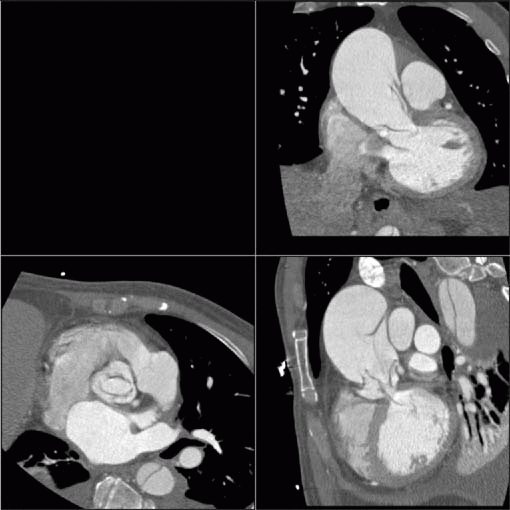
5b A gated CTA is then obtained. What other type of imaging would be most helpful to determine the diagnosis?
|
A. Left anterior oblique reformat of the thoracic aorta
B. Another cardiac phase in the gated CTA
C. Noncontrast images
D. Delayed images
View Answer
5b Answer C. Gated CTA confirms wall thickening/fluid surrounding the ascending aorta. This is concerning for a type A dissection/intramural hematoma. Blood can be confirmed with a noncontrast sequence, which should show high attenuating fluid in the aortic wall. Left anterior oblique reformat can visualize the aorta in its entirety but would not be helpful to determine the attenuation value of the wall. Another phase in the cardiac cycle will also not help determine if there is blood. Delay images can potentially be helpful by showing the wall better with less luminal contrast but will not be as good as the noncontrast images.
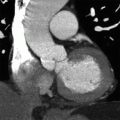
5c This is the patient re-imaged a few hours later. What is the best next step in the management of this patient?
|
A. Medical management
B. Immediate surgery
C. Endovascular
D. Additional imaging
View Answer
5c Answer B. The noncontrast image confirms high density surrounding the ascending aorta, which makes this a type A dissection equivalent with intramural hematoma versus retrograde extension of the dissection down the ascending thoracic aorta. The best next step is immediate surgery.
References: Karmy-Jones R, Aldea G, Boyle EM Jr. The continuing evolution in the management of thoracic aortic dissection. Chest 2000;117(5):1221-1223. PubMed PMID: 10807801.
Mészáros I, Mórocz J, Szlávi J, et al. Epidemiology and clinicopathology of aortic dissection. Chest 2000;117(5):1271-1278. PubMed PMID: 10807810.
6 Annuloaortic ectasia is most commonly associated with Marfan syndrome. What other condition can also produce similar findings?
A. Syphilis
B. Bicuspid aortic valve
C. Takayasu arteritis
D. Ehlers-Danlos syndrome
View Answer
6 Answer D. Annuloaortic ectasia is classically associated with Marfan syndrome. Other causes include Ehlers-Danlos syndrome, homocystinuria, and osteogenesis imperfecta. It can also be idiopathic without underlying genetic abnormality. Syphilitic aneurysm does not often involve the aortic root. Bicuspid aortopathy does not typically dilate the sinotubular junction. Takayasu arteritis tends to narrow the aorta.
Reference: Agarwal PP, Chughtai A, Matzinger FR, et al. Multidetector CT of thoracic aortic aneurysms. Radiographics 2009;29(2):537-552. doi: 10.1148/rg.292075080. Review. PubMed PMID: 19325064.
7 In aortic dissection, what is the most diseased portion of the aorta?
A. Intima
B. Media
C. Adventitia
D. Vasa vasorum
View Answer
7 Answer B. Aortic dissection is defined by the disruption of the aortic intima with blood dissecting into the media of the aortic wall. The most diseased portion is therefore the media, which is disrupted. The intima can be mostly intact with an entry tear. If the adventitia is disrupted, there would be aortic rupture. The vasa vasorum is involved in intramural hematoma.
Reference: McMahon MA, Squirrell CA. Multidetector CT of aortic dissection: a pictorial review. Radiographics 2010;30(2):445-460. doi: 10.1148/rg.302095104. Review. PubMed PMID: 20228328.
8 Dissection at the aortic arch is considered what type of dissection using the Stanford classification?
A. Type A
B. Type B
C. Type C
View Answer
8 Answer B. Dissection at the arch is considered a type B Stanford dissection. Type A involves the ascending aorta. Type B is any other type of dissection that does not involve the ascending aorta. There is no Stanford type C dissection.
Reference: McMahon MA, Squirrell CA. Multidetector CT of aortic dissection: a pictorial review. Radiographics 2010;30(2):445-460. doi: 10.1148/rg.302095104. Review. PubMed PMID: 20228328.
9 What is the most common risk factor for aortic dissection?
A. Hypertension
B. Cystic medial degeneration
C. Marfan syndrome
D. Aortic aneurysm
View Answer
9 Answer A. Hypertension is the most common risk factor for aortic dissection, occurring in a majority of patients with dissection. All of the other answer choices are less common risk factors for dissection.
Reference: McMahon MA, Squirrell CA. Multidetector CT of aortic dissection: a pictorial review. Radiographics 2010;30(2):445-460. doi: 10.1148/rg.302095104. Review. PubMed PMID: 20228328.
A. Aortic regurgitation
B. Aortic stenosis
C. Aortic valve endocarditis
D. Aortic rupture
View Answer
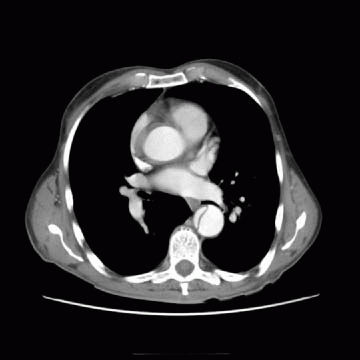
10 Answer A. Reformatted images at the aortic root show type A dissection with the dissection flaps prolapsing into the aortic root during diastole causing aortic regurgitation.
Reference: McMahon MA, Squirrell CA. Multidetector CT of aortic dissection: a pictorial review. Radiographics 2010;30(2):445-460. doi: 10.1148/rg.302095104. Review. PubMed PMID: 20228328.
A. Intima
B. Media
C. Adventitia
View Answer
11a Answer C. An outpouching is seen in the descending thoracic aorta, which is consistent with a penetrating aortic ulcer (PAU). In a penetrating aortic ulcer, there is disruption of the inner layer (intima) by the penetrating ulcer with subsequent bleed in the medial layer. In this case, there is focal dilation of the aorta at the site of PAU. The adventitial/outer layer is intact or else there would be aortic rupture.
Reference: Castañer E, Andreu M, Gallardo X, et al. CT in nontraumatic acute thoracic aortic disease: typical and atypical features and complications. Radiographics 2003;23:S93-S110. Review. PubMed PMID: 14557505.
11b The patient remains asymptomatic, what is the next step?
A. Medical therapy
B. Surgery
C. Endovascular stenting
View Answer
11b Answer A. Penetrating aortic ulcers typically occur in the descending aorta and is considered a type B aortic dissection equivalent. The most appropriate treatment in an asymptomatic patient is medical therapy (control blood pressure). It is only in patients who have aortic rupture/hemodynamic instability that surgery is considered. Endovascular treatment can be performed particularly given the high risk of surgical repair. Indications for treatment include symptomatic patients or if there is rapid enlargement of the ulcerating aneurysm.
Reference: Castañer E, Andreu M, Gallardo X, et al. CT in nontraumatic acute thoracic aortic disease: typical and atypical features and complications. Radiographics 2003;23:S93-S110. Review. PubMed PMID: 14557505.
A. Premature atherosclerosis
B. Marfan syndrome
C. Takayasu arteritis
D. Prior syphilis infection
View Answer
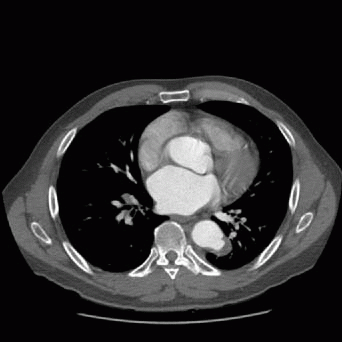
12 Answer B. This is a patient with Marfan syndrome who had a Bentall composite aortic root replacement that developed large coronary button aneurysms. Note the dissection in the descending thoracic aorta. Due to the underlying aortic wall abnormality in Marfan patients, the reimplanted contrary buttons can be prone to aneurysm formation. While Takayasu and prior syphilis infection can give rise to aneurysms, they are not associated with coronary button aneurysms.
References: Bruschi G, Cannata A, Botta L, et al. Giant true aneurysm of the right coronary artery button long after aortic root replacement. Eur J Cardiothorac Surg 2013;43(5):e139-e140. doi: 10.1093/ejcts/ezt057. Epub 2013 Feb 20. PubMed PMID: 23425675.
Prescott-Focht JA, Martinez-Jimenez S, Hurwitz LM, et al. Ascending thoracic aorta: postoperative imaging evaluation. Radiographics 2013;33(1):73-85. doi: 10.1148/rg.331125090. Review. PubMed PMID: 23322828.