Acquired Metabolic, Systemic, and Toxic Disorders
Acute Hypertensive Encephalopathy
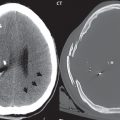
This entity, also known by the term posterior reversible encephalopathy syndrome (PRES), is caused by acute severe hypertension. There is a predilection for involvement of the parietooccipital regions (the posterior circulation), with bilateral, symmetric abnormal high signal intensity (vasogenic edema) on fluid attenuated inversion recovery (FLAIR) involving the cortex and subcortical white matter in a nonvascular distribution ( Fig. 1.34 ). In prominent disease, the involvement of the cerebral hemispheres may be more extensive. Diffusion is usually not restricted. There may be accompanying involvement of the basal ganglia.

Wernicke Encephalopathy
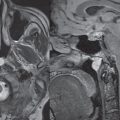
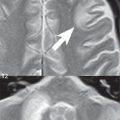
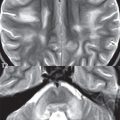
This entity is caused by thiamine deficiency, and is seen in severe malnutrition, in particular with alcohol abuse. On FLAIR, in extensive disease, abnormal bilateral hyperintensity can be noted in the mamillary bodies, around the third ventricle, and in the medial thalami, tectal plate, and periaqueductal area ( Fig. 1.35 ). Involvement of the mamillary bodies is a distinctive feature. The mamillary bodies can also have abnormal contrast enhancement, as can occur in the other involved areas.

Hepatic Encephalopathy
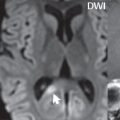
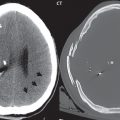
This entity can occur with either acute or chronic liver disease, and is characterized on MR imaging by high signal intensity bilaterally within the globus pallidus on T1-weighted images ( Fig. 1.36 ). The signal intensity characteristics are thought to reflect manganese deposition. Similar findings can be seen with hyperalimentation.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree