Normal Anatomy and Common Variants
Normal Intracranial Anatomy
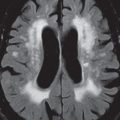
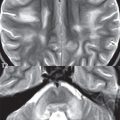
The frontal lobe is demarcated posteriorly from the parietal lobe by the central sulcus ( Fig. 1.1 ). On axial magnetic resonance (MR) images near the vertex, the central sulcus is readily identified. It is the major sulcus just behind the “L,” the intersection of two sulci formed in part by the superior frontal sulcus. The precentral gyrus lies just anterior to the central sulcus and the postcentral gyrus just posteriorly. As a generalization, the primary motor area (Brodmann area 4) is located in the precentral gyrus, and the primary somatesthetic (body′s sensations) area (Brodmann areas 1, 2, and 3) in the postcentral gyrus. The parietal lobe is demarcated from the occipital lobe posteriorly by the parieto-occipital sulcus (fissure). The anatomy of the nuclei and white matter tracts is beyond the scope of this book, but see Fig. 1.2 . The reader is referred to the many computer-based atlases, including The Human Brain in 1969 Pieces by Wieslaw Nowinski.



The pituitary gland is divided into anterior and posterior lobes. The anterior pituitary is referred to as the adenohypophysis and the posterior pituitary as the neurohypophysis. The normal pituitary is less than 10 mm in height, and demonstrates intense enhancement following intravenous contrast administration, due to the lack of a blood–brain barrier. A common variant in appearance of the pituitary is a slight upward convex superior margin, which can be seen in young women. On T1-weighted scans, the posterior pituitary is seen to be hyperintense in up to half of the normal patient population, a finding that is more common in younger patients (but not in the elderly).
The internal auditory canal (IAC) is a bony foramen within the petrous portion of the temporal bone. It contains the 7th (facial) and 8th (vestibulocochlear) nerve complexes. The 7th nerve lies in the anterior superior quadrant of the IAC, when viewed in cross-section, and runs laterally to the geniculate ganglion. The cochlear division of the 8th nerve lies in the anterior inferior quadrant. The superior and inferior vestibular nerves, also divisions of the 8th nerve, which supply information concerning equilibrium, lie in the superior and inferior posterior quadrants. As visualized in the axial plane, the cochlea is anterior and the vestibule posterior. There are three semicircular canals: the lateral (which has a horizontal orientation), superior, and posterior. The fluid (endolymph) within the cochlea, vestibule, and semicircular canals is normally isointense to cerebrospinal fluid (CSF) on MR.
Normal Arterial Anatomy
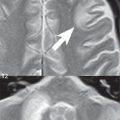
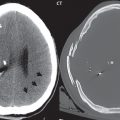
Three major arteries supply the cerebral hemispheres ( Fig. 1.3 ). The anterior cerebral artery (ACA) supplies the anterior two-thirds of the medial cerebral surface and 1 cm of superior medial brain over the convexity. The recurrent artery of Heubner, which originates from the A1 or A2 segment of the ACA, supplies the caudate head, anterior limb of the internal capsule, and part of the putamen. The posterior limb of the internal capsule, portions of the thalamus, the caudate, the globus pallidus, and the cerebral peduncle are supplied by the anterior choroidal artery, which arises from the supraclinoid internal carotid artery. The middle cerebral artery (MCA) supplies the lateral portion of the cerebral hemispheres, the insula, and the anterior and lateral temporal lobes. The lenticulostriate arteries, which originate from the M1 segment of the MCA, supply the lentiform nucleus (globus pallidus and putamen) and the anterior limb of the internal capsule. The posterior cerebral artery (PCA) supplies the occipital lobe and the medial temporal lobe. The thalamoperforating and thalamogeniculate branches supply the medial portion of the thalami and the walls of the third ventricle. These small perforating branches arise from the P1 segment of the PCA with similar branches arising from the posterior communicating artery ( Fig. 1.4 ).


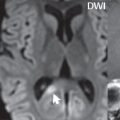
Three major but smaller vessels supply the cerebellum ( Fig. 1.5 ). The largest is the posterior inferior cerebellar artery (PICA), which supplies the tonsil, the inferior vermis, and the inferior cerebellum (with the exception of its most anterior extent). The anterior inferior cerebellar artery (AICA) supplies the anterior inferior portion of the cerebellum and is the smallest of the three vessels. It is commonly stated that the distribution of AICA is in continuum with PICA, with at times the distribution slightly larger or smaller. The superior cerebellar artery supplies the superior half of the cerebellum.

The circle of Willis is complete in only one quarter of the population. Variants include the following. A fetal origin of the posterior cerebral artery, with its origin from the internal carotid artery instead of the basilar artery, is seen in about one in five patients. The P1 segment of the posterior cerebral artery, which is the portion from the tip of the basilar artery to the junction with the posterior communicating artery (PCOM), is usually also hypoplastic in this circumstance. The PCOM is hypoplastic in one-third of patients. The anterior communicating artery (ACOM), which connects the two anterior cerebral arteries, is hypoplastic in 15%. The A1 segment of the anterior cerebral artery, which begins at the carotid terminus and continues to the juncture with the ACOM, is hypoplastic in 10%.
The external carotid artery is the smaller of the two terminal branches of the common carotid artery. It arises anterior and medial to the internal carotid artery, then courses posterior laterally. There are many muscular branches, with the early branching of the external carotid artery allowing rapid recognition of this vessel in distinction to the internal carotid artery.
The internal carotid artery was traditionally divided into four major segments: the cervical, the petrous (horizontal), the cavernous (juxtasellar), and the intracranial (supraclinoid) portions. Today, there are seven recognized segments (C1 to C7): the cervical, petrous, lacerum, cavernous, clinoid, ophthalmic, and communicating (terminal) segments. At its origin, the internal carotid artery is somewhat dilated, forming the carotid bulb. The petrous segment, C2, of the internal carotid artery has three sections: the ascending (vertical), the genu (bend), and the horizontal portions. The lacerum segment, C3, is still extradural. The cavernous segment, C4, is surrounded by the cavernous sinus. The meningohypophyseal artery arises from C4. The clinoid segment, C5, is very short, and begins after the artery exits from the cavernous sinus. C5 extends from the proximal dural ring to the distal dural ring. C6, the ophthalmic segment, extends from the distal dural ring (with this portion of the internal carotid artery thus considered intradural) to the origin of the PCOM. The ophthalmic artery arises from C6. C7 is that segment of the artery extending from the origin of the posterior communicating artery to the carotid terminus, where the vessel divides into the anterior and middle cerebral arteries. C6 and C7 together constitute the supraclinoid internal carotid artery.
There are many extracranial–intracranial vascular anastomoses. Two of these involve the ophthalmic artery. There are also multiple internal carotid–vertebral artery anastomoses, which represent persistent embryonic circulatory patterns. One of these is seen not uncommonly, as a normal variant, and is the persistent trigeminal artery ( Fig. 1.6 ). Pial–leptomeningeal anastomoses are also present, and are an important potential source of collateral blood flow in occlusive vascular disease.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree