Dementia and Degenerative Disease
Alzheimer Disease
Alzheimer disease is today the most common diagnosed cause of dementia. Histology is nonspecific. CT and MR imaging signs are nonspecific, with generalized brain atrophy seen in advanced cases. Accentuated temporal lobe atrophy may be present.
Frontotemporal Dementia
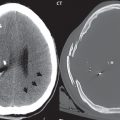
This heterogeneous group of disorders is characterized by selective frontal and temporal lobe atrophy ( Fig. 1.71 ). Less common than Alzheimer disease, it also has a younger mean age of onset. The term Pick disease is today used for a distinct neurodegenerative disease within this group, defined by the presence of Pick bodies (dark staining aggregates of proteins on histopathology).

Multisystem Atrophy
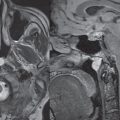
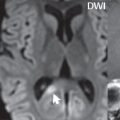
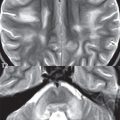
The most accepted classification of multisystem atrophy (MSA) considers symptomatology a key for diagnosis. The disease is designated as MSA-P if parkinsonism is the main symptom, whether associated or not with autonomic dysfunction. Striatonigral degeneration is the old term for the same disease. On the other hand, if cerebellar ataxia is the main symptom, once again whether associated or not with autonomic dysfunction, it is designated as MSA-C. Olivopontocerebellar atrophy/degeneration is the old term for this disease. MR imaging in Parkinson disease reveals loss of the substantia nigra pars compacta, with reduced width in a lateral to medial gradient (most prominently of the more lateral portion), best evaluated on dedicated inversion recovery T1-weighted sequences. In MSA-C, there is atrophy of the pons, middle cerebellar peduncles, olives (which lie along and form the anterolateral margin of the medulla), and cerebellar hemispheres. The “hot cross bun” sign is also described in MSA-C, with cruciform high T2 signal intensity on axial imaging within the pons, reflecting selected loss of myelinated transverse fibers and neurons in the pontine raphe ( Fig. 1.72 ). MR findings may appear many years after clinical findings, and alone cannot confirm the diagnosis.

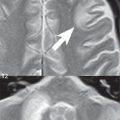
Atrophy of the vermis, most commonly, but often including the cerebellar hemispheres also occurs in up to 40% of chronic alcoholics. It is irreversible. Cerebellar atrophy is known as well to be associated with the chronic use of Dilantin (phenytoin) for treatment of seizures ( Fig. 1.73 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree