ACUTE AND SUBACUTE SINUSITIS
KEY POINTS
- Imaging should be used only in a small fraction of patients who have a clinical diagnosis of acute sinusitis.
- Imaging can identify underlying causative or alternative conditions that may significantly affect medical and surgical decision making.
- Imaging is critical in identifying and excluding orbital and intracranial complications of acute bacterial sinusitis when there is a reasonable clinical suspicion of those conditions, although imaging can never exclude meningitis.
INTRODUCTION
Etiology
Sinusitis is an inflammation of the paranasal sinus mucoperiosteal lining. Rhinosinusitis is currently the preferred term for this condition because the nasal mucosa is almost always simultaneously involved when sinusitis occurs.1 Rhinosinusitis is acute when symptoms last <3 weeks. Subacute rhinosinusitis has symptoms lasting between 21 and 60 days, and those of chronic rhinosinusitis last more than 90 days.
Rhinosinusitis is also classified anatomically as maxillary, ethmoidal, frontal, and sphenoidal as well as by infecting organism as viral, bacterial, or fungal. Fungal sinonasal infection is discussed separately in Chapter 86 because of its most often disparate clinical setting, occurring mainly in immune-compromised rather than otherwise healthy patients, and its difference in pathophysiology and spread patterns from the more common bacterial and viral infections that cause rhinosinusitis.
Other considerations in classification include whether there are orbital or intracranial complications present and if there are associated factors such as nasal polyposis or an immune-compromised state.
Prevalence and Epidemiology
Rhinosinusitis affects many millions of children and adults per year in the United States and worldwide. About 14% of adults will have an episode of rhinosinusitis each year, and it is a very common diagnosis for which antibiotics are prescribed. Approximately 0.5% to 2.0% of viral rhinosinusitis cases are complicated by bacterial superinfection. Acute bacterial rhinosinusitis is commonly overdiagnosed, with that diagnosis being correct less than half the time when made by a primary care physician.2 A typical rhinovirus infection lasts from 1 to 33, with about a quarter of the patients having symptoms that last longer than 14 days.3 Acute fungal sinusitis occurs almost exclusively in immune-compromised patients; that disease is discussed in Chapter 86. Orbital and intracranial complications of bacterial sinusitis are infrequent but can be devastating, even leading to death.
Patients with a history of allergy, occupational or vasomotor rhinitis, and anatomic obstruction such as septal deviation or nasal polyps will be predisposed to infections. Rhinosinusitis is more common in patients with deficiencies of humoral immunity and ciliary motility such as transplant patients, immune-deficient patients, and those with cystic fibrosis or Kartagener syndrome, respectively.
Clinical Presentation
Patients with uncomplicated rhinosinusitis can have rhinorrhea, nasal congestion, facial pressure and pain, diminished sense of smell, and perhaps fever.
Acute bacterial rhinosinusitis becomes much more likely when symptoms of a viral upper respiratory infection fail to improve after 10 days or worsen after 5 to 7 days. A change in the color or characteristic of the nasal discharge is not a specific sign of bacterial rhinosinusitis. Acute rhinosinusitis will cause often unilateral facial pain or pressure, maxillary dental pain, and ear fullness/pressure. On physical examination, there can be purulent nasal secretions disease, mucosal erythema, tenderness overlying sinuses, fever, and periorbital edema even in the absence of orbital complications.
PATHOPHYSIOLOGY
Anatomy
The sinuses are divided into anterior and posterior groups that drain into the middle meatus anteriorly and into the sphenoethmoidal recess and superior meatus posteriorly. The anatomy is discussed in detail in Chapter 78, and the physiology of sinonasal mucous clearance related to this anatomy is considered in the following material and also in Chapter 83 on endoscopic sinus surgery.
The paranasal sinuses are lined with a pseudostratified columnar (respiratory) epithelium that is continuous with the nasal mucosa. The mucoperiosteal sinus and nasal lining produces mucous secretions that trap bacteria, and both the mucus and bacteria are transported along a mucous blanket through the sinus ostia to be swallowed or expectorated. This is a normal process in sinuses that are air filled and communicate with the nasal passages through patent ostia.
Pathology and Patterns of Disease
The vast majority of rhinosinusitis episodes are caused by viruses. Most viral upper respiratory infections are caused by rhinovirus, but many other types are possible. Almost all patients with upper respiratory infections have imaging findings of sinus mucoperiosteal thickening, but only 0.5% to 2.0% of viral rhinosinusitis infections are complicated by bacterial infection.3
The system of sinonasal mucociliary transport is supported by the coordination of the ciliated columnar epithelial cells that move the sinus contents toward the natural sinus ostia. Disruption of the ciliary function results in accumulation of sinus secretions and potentially infectious agents within the sinus. Ciliary function can be disrupted by the loss of ciliated epithelial cells, high airflow and cold air, toxins produced by micro-organisms, or environmental mediators of the inflammatory response. Mechanical factors with the potential to impede transport of the mucosal blanket include contact between two mucosal surfaces and scarring. Primary ciliary dyskinesia may occur in conditions such as Kartagener syndrome. Secondary ciliary dysfunction can occur with other conditions such as chronic infections and secondhand smoke exposure. The mucous blanket contains mucoglycoproteins, immunoglobulins, and inflammatory cells. Alterations in the water content of the mucous blanket can impair ciliary mobility, as in cystic fibrosis. Overproduction of mucus can overwhelm the mucociliary clearance system, resulting in retained secretions within the sinuses.
Rhinosinusitis results in obstruction of sinus drainage pathways, ciliary impairment, and mucus quantity and quality. When the natural sinus ostia become obstructed, normal mucus drainage is impeded. Aside from the edema and inflammation caused by the initial infecting agent, polyps, scarring, anatomic variants such as nasal septal deviation, and therapeutic interventions such as a nasogastric tube can further obstruct the sinus ostia. The obstructed sinus environment becomes hypoxic and causes ciliary dysfunction and changes in mucus production—all of this further reducing normal mucus clearance.
Uncomplicated acute bacterial sinusitis should be considered akin to an abscess or empyema since it is essentially a collection of pus under pressure. It is this fundamental situation that creates a potential for the orbital and intracranial complications. The intrasinus pressure encourages a retrograde thrombophlebitic spread of pus that is one mechanism causing the complications discussed subsequently. It likely contributes to the pathophysiology of bone erosion and direct spread of disease beyond the bony sinus limits as well. Relieving this pressure by draining the causative sinus is a strategy aimed at the prevention and treatment of such complications. Such drainage also promotes the restoration of normal sinonasal mucociliary drainage by reversing some of the elements, discussed previously, causing that dysfunction.
Complications
The pathophysiology of the orbital and intracranial complications that occasionally are secondary to sinonasal infectious disease is described in general in Chapters 13 (Figs. 13.15 and 13.16), 14, and 62. Localized osteomyelitis is an uncommon complication of advanced pyogenic frontal sinuses disease. It is a common finding in acute and subacute fungal sinusitis (Chapter 86). These complications occur both by direct extension and thrombophlebitic spread.
Orbital Complications
Orbital involvement is the most common complication of sinusitis. The most common of these is preseptal (Chapter 70) and postseptal (Chapter 62) orbital cellulitis. Subperiosteal abscess and intraorbital abscess (Chapter 62) are less common (Figs. 62.2–62.6 and 84.1). Orbital complications (Figs. 62.2–62.6 and Chapter 62) may be direct through dehiscent zones in the usually thin bone of the medial orbital wall or through neurovascular foramina. There may be septic thrombophlebitis of the valveless superior and inferior ophthalmic veins that have communication with the nose, the ethmoids, and the cavernous sinus. The orbital periosteum is a strong soft tissue boundary barrier between the sinuses and the orbit.
Cavernous Sinus Thrombosis
Most cases of cavernous sinus thrombosis (Figs. 72.1–72.5 and Chapter 72) are caused by infections of the middle one third of the face including the sinonasal region (Fig. 84.2). The ophthalmic veins are valveless and provide a direct route of infection to the cavernous sinus. Major dural sinus thrombosis from pyogenic sinusitis may spread via the cavernous sinuses or other venous pathways to also involve the superior sagittal sinus, clival plexus, and petrosal sinuses or even spread to more distant venous drainage pathways (Figs. 72.1–72.5).
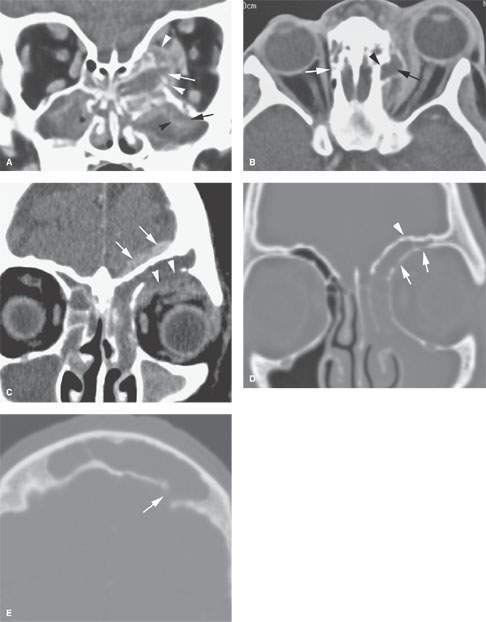
FIGURE 84.1. Contrast-enhanced computed tomography studies of two patients with acute sinusitis with associated complications. A, B: Patient 1. In (A), the basic pathophysiology of sinus disease is shown by mucosal enhancement (black arrowhead) and submucosal edema (black arrow) in the maxillary sinus. Luminal secretions accumulate within the bounds of the enhancing sinus mucosa. The ethmoid infected contents have broken through the medial wall of the orbit (white arrow) and displaced the periorbita (white arrowheads), laterally creating an early subperiosteal abscess and related phlegmon. This is an example of direct extension of sinus disease into an adjacent area. In (B), an axial section shows the postseptal subperiosteal abscess (black arrow). Notice that the central point of extension into the orbit is erosion of bone at the expected position of the ethmoid artery (black arrowhead) compared to the normal appearance of the anterior ethmoid canal on the right (white arrow). The area of the ethmoid artery represents an inherent area of weakness in the ethmoid complex and is frequently a focal point of spread of pathology from the ethmoid sinus to the orbit. C–E: Patient 2. In (C), the infected contents of the frontal sinus extend directly through the orbital roof to produce a superior orbital subperiosteal abscess (arrowheads). In addition, there is an extra-axial area of enhancement (arrows) without an obvious bony defect along the margin of the frontal sinus superiorly. In (D), bone windows show fairly obvious erosion of the superior and medial roof of the orbit (arrows) but fail to demonstrate erosion of the frontal sinus wall (arrowhead). In (E), the breach responsible for the epidural collection was seen only in the axial images along the inner table of the frontal sinus (arrow). If this defect had not been found, the intracranial spread would have been presumed to be due to spread via thrombophlebitis.
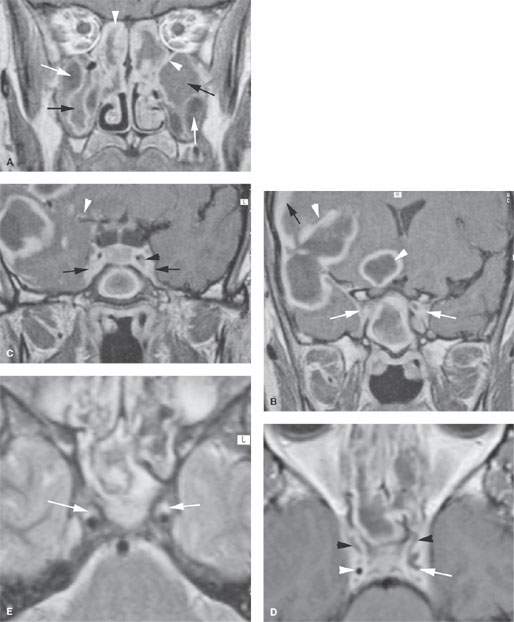
FIGURE 84.2. Magnetic resonance study of a patient with acute sinusitis with extensive intracranial complications. This was due to community methicillin-resistant Staphylococcus aureus (MRSA) sinus infection. A–D: Contrast-enhanced T1-weighted images. In (A), the variable appearance of mucosa and luminal contents in acute sinus disease is shown by this figure. The enhancing mucosa may be thick or relatively thin (arrowheads). The submucosal edema (white arrows) can vary in signal intensity but is simple to detect as it displaces the mucosa centrally. The luminal contents also vary in signal intensity, mainly depending on protein content (black arrows). In (B), there is extension of this disease to the cavernous sinus by way of infected veins (white arrows). This spread was not due to orbital involvement. There are also very extensive brain abscesses (white arrowheads) and reactive meningeal disease and possible early subdural empyema present (black arrow). In (C), a section through the cavernous sinus shows abnormal enhancement and widening as evidence of its involvement (black arrows) and lack of filling around the narrowed cavernous carotid artery (black arrowhead). There is also evidence of spread along vessels and/or within the leptomeninges (white arrowhead). In (D), the cavernous sinuses show irregular filling defects consistent with thrombosis in diffusely infected cavernous sinuses. The infection also is manifest by the diminished size of the right cavernous carotid artery (white arrowhead) and the unusual shape associated with the left cavernous carotid (white arrow), part of which is likely a filling defect due to thrombus as well. E: T2-weighted image showing the cavernous carotid arteries markedly diminished in size and abnormality either around the arteries or within their walls as a result of infection (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








