KEY FACTS
Imaging
- •
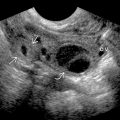
Findings of acute pyelonephritis (AP) are almost always asymmetric
- •
Renal enlargement with loss of corticomedullary differentiation
- •
Geographic areas of altered echogenicity
- •
Urothelial thickening
- •
In general, ultrasound is much more sensitive for causes (obstruction) and complications (abscess) of AP than for AP itself, which is clinical diagnosis
- •
Many kidneys with pyelonephritis will be sonographically normal
- •
Foci of gas in parenchyma (rare) could indicate emphysematous pyelonephritis; treat as urologic emergency
- •
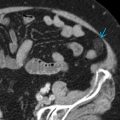
Altered nephrogram on CT, classically striated, best seen in excretory phase
- •
Microabscesses or areas of necrosis can emerge after 1-2 weeks of infection
Pathology
- •
Most common organism: Escherichia coli
- •
Route of spread of infection: Ascending (85%) > hematogenous (15%)
- •
Risk factors include obstruction, ureteric reflux, diabetes, pregnancy, lower UTI
Clinical Issues
- •
Positive urine culture for bacilli is typical
- •
Remember, especially in children, absence of lower UTI does not exclude pyelonephritis
Scanning Tips
- •
Pyelonephritis usually asymmetric; sonographic changes may be subtle in acute setting
- •
Focused US evaluation for ureteral stones if AP is suspected, including transvaginal images for distal ureter stones, because presence of stones would alter management
- •
Higher frequency linear transducers, especially in thin patients, may help identify subtle areas of involvement
- •
Best acoustic windows are often through liver or spleen but evaluation with different acoustic windows important for full evaluation