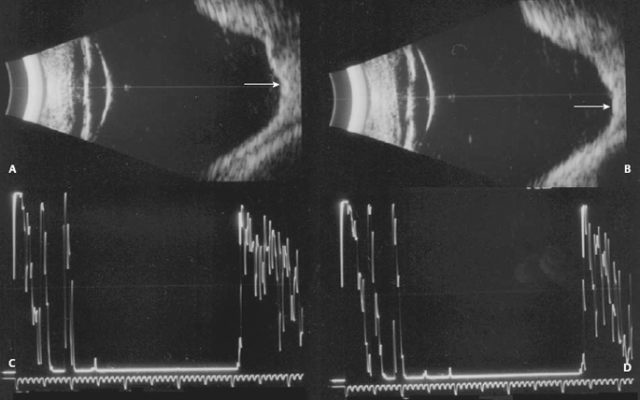
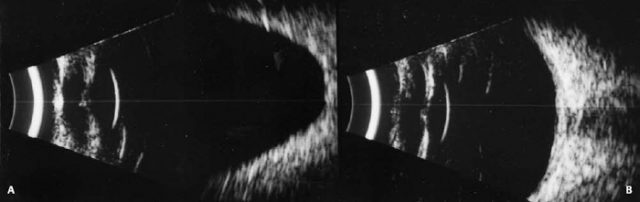
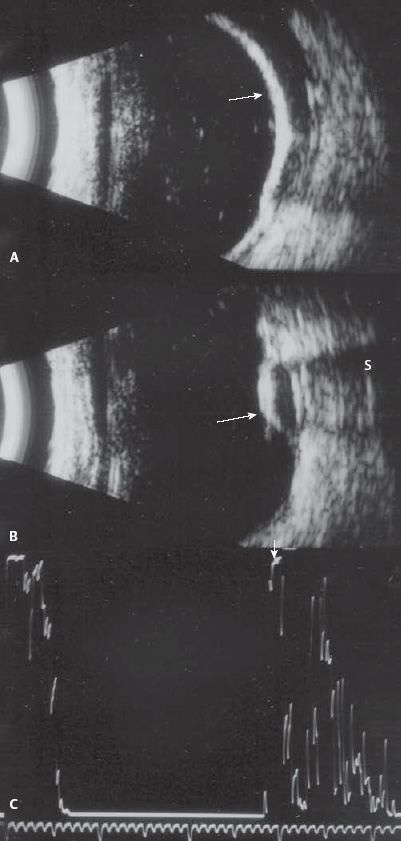
11 A collection of echographic images and findings for unusual or uncommon ocular conditions follows. In addition, we have included a section focusing on biometry for axial length measurements, as well as a brief discussion about the use of laser interferometry (IOLMaster®, Carl Zeiss Meditec, Dublin, CA) to obtain accurate measurements. We are all aware of the importance of obtaining accurate axial length measurements, as well as achieving reliable intraocular lens calculations, and patient satisfaction plays a major role in determining the outcome of the services we provide. Having a quality control mechanism to evaluate the results is extremely important. One way to increase the chances that the axial length measurements and calculations are appropriate for each patient is to employ a skilled echographer. Whether this person is a physician or a technician, having the ability to identify inaccuracies in the measurements and poor scan quality and knowing when further investigation is indicated are of utmost importance to achieve desirable postoperative results. The newer generation biometers offer many valuable features and have become increasingly more user friendly, however; the level of knowledge of the person or persons performing these examinations should take precedence over letting the equipment do the work and make the final determinations. There are several things to be considered when performing axial length measurements. The most important is to know the echographic features that indicate a good quality scan. These include steeply rising, high spikes from the cornea, anterior and posterior lens surfaces, and the retina (indications that the sound beam is aimed perpendicular to each of these structures). In addition, monitoring the anterior chamber depth as a way to minimize corneal compression, looking for the maximal lens thickness and using the longest measurement of a series of good scans obtained at the macula are vital components. Another factor that will have a significant impact on the final surgical outcome is the proper use of the A-constant, surgeon factor (SF), or anticipated anterior chamber depth constant (ACD), which are provided by the manufacturer of each lens. Studies suggest a close correlation between the various formulas now being used (in eyes of average length) as long as the correct numbers (A-constant, SF, or ACD) are incorporated into the equation. Using the correct sound velocities is also important. The average speed of sound through the phakic eye is 1550 m/s (meters per second), whereas the velocity through the aphakic eye is slowed to 1532 m/s. Pseudophakic eyes and eyes filled with silicone can also be measured using appropriate sound velocities and most equipment on the market today has been designed with adjustable settings to accommodate the different eye types. It is recommended that comparison measurements be made between the two eyes and if a difference of 0.3 mm or greater is found, a B-scan screening should be performed. B-scan should also be performed if there is difficulty obtaining perpendicularity to the intraocular structures or if atypical spikes are noted along the vitreous baseline that do not disappear with a change in the sound beam direction. In 2004, partial coherence interferometry (PCI) was introduced as a new way of obtaining accurate axial length measurements. The technique differs from ultrasound in that it uses near-infrared light instead of sound. It does not require contact with the eye and the corneal curvature, anterior chamber depth, axial length, and “white to white” measurements can be automatically obtained in a relatively short amount of time. The equipment is programmed with the most accurate calculation formulas, and calculations can be obtained with a few keystrokes. Gantenbein CP, Ruprecht KW. Comparison between optical and acoustic biometry. J Fr Ophtalmol 2004;27(10):1121–1127 Haigis W, Lege B, Miller N, Schneider B. Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol 2000;238(9):765–773 Figure 11-1 Staphyloma. Echograms from a patient with bilateral posterior staphylomas. (A) and (B) Horizontal axial scans showing the irregular globe contours and elongation of the globe involving the maculae (arrows). (C) and (D) Axial length measurements using the contact method. The right eye measured 32.2 mm, and the left eye measured 34.2 mm. Figure 11-2 Staphyloma. (A) and (B) Axial echograms of a patient with unilateral axial myopia. The left eye is much longer than the right.
Additional Ocular Conditions and Biometry
♦ Traditional Biometry for Axial Length Measurements and New Technology
Traditional Biometry
New Biometry Technology
♦ Suggested Readings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree