KEY FACTS
Terminology
- •
Synonym: Adrenocortical adenoma
Imaging
- •
Varies from 2-5 cm, typically < 3 cm, bilateral in 10%
- •
Can be bilateral (10%)
- •
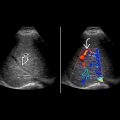
Nonspecific sonographic appearance
- •
Well-circumscribed, solid, oval-shaped mass
- •
Usually homogeneous and hypoechoic
- •
Atypically can appear more heterogeneous, but necrosis is rare in small adenomas
- •
Necrosis is seldom seen in small adenoma
- •
May suggest diagnosis based on US; however, no specific sonographic features distinguish adenomas from other adrenal lesions
- •
Typically small, smoothly marginated, homogeneous, and hypoechoic
- ○
Size is particularly important: Smaller adrenal lesions tend to be benign; > 4 cm more likely malignant
- ○
Size stability over 12 months supports benignity
- ○
- •
Smaller lesions are seen with Conn syndrome, usually < 2 cm (20% < 1 cm)
- •
CT and MR: Best imaging modalities to confirm diagnosis
- ○
Lipid-rich adenomas are best characterized with NECT or chemical shift MR
- ○
Lipid-poor adenomas can be characterized with CECT with 10-min delayed-phase imaging
- ○
- •
T1WI: Chemical shift MR can confirm presence of intracellular lipid
- •
Lipid-rich adenomas (70-90%): Attenuation < 10 HU is characteristic and diagnostic
- •
Hypovascular on color Doppler
Top Differential Diagnoses
- •
Adrenal metastases
- •
Adrenal hemorrhage
- •
Pheochromocytoma
Pathology
- •
Classified as nonfunctioning vs. functioning
- •
70% show high intracytoplasmic lipid content: “lipid rich”
Clinical Issues
- •
More commonly detected as incidental finding
- ○
Increased detection in recent years due to greater imaging utilization, > 90% of all incidentalomas
- ○
- •
15% are functional and produce hormones
- •
Accounts for > 90% of all incidentalomas
- •
Functioning adenomas: Cushing syndrome, Conn syndrome, or virilization syndromes
- ○
Cushing syndrome, Conn syndrome, or virilization syndromes
- ○
- •
Hypertension and weakness with Cushing and Conn syndrome
Diagnostic Checklist
- •
Benign vs. malignant: Consider size and stability
- ○
Comparison with any available prior imaging may help to establish stability over 12 month period and avoid unnecessary additional testing
- ○
- •
Attenuation < 10 HU on NECT → lipid-rich adenoma
- •
Signal drop on T1 out-of-phase MR → lipid-rich adenoma
- •
> 60% absolute washout on 10-min delayed-phase CECT → lipid-rich and lipid-poor adenomas
Scanning Tips
- •
Size and stability are helpful clues to diagnosis
- •
CT or MR required for confirmation
 arising from the peripheral adrenal gland. Note the oval shape and smooth margin typical of an adrenal adenoma. Adenomas have a high cholesterol content similar to adrenal cortex.
arising from the peripheral adrenal gland. Note the oval shape and smooth margin typical of an adrenal adenoma. Adenomas have a high cholesterol content similar to adrenal cortex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree