Abstract
Aims
To evaluate dental anomalies in survivors of childhood cancer after chemotherapeutic and irradiation therapy at 0–6 years of age and compare it with healthy controls.
Material and methods
Retrospective analysis was performed for 47 childhood cancer survivors aged below six years at time of diagnosis and minimum 14 years old at time of analysis. Cancertherapy-related information and dental case history, including x-rays and photographs, were evaluated. All teeth were dichotomously assessed for malformations like agenesis, microdontia, hypoplasia, and root dilacerations.
Results
We identified six main malformations that were overpresented in childhood cancer survivors in comparison to control group. Of all evaluated teeth we detected 2.5% agenesis, 4% microdontia, 3.8% circular hypoplasia and 6.8% or 6.1% slender or shortened root, respectively. Findings were correlated to the age at start of therapy, showing a strong correlation between a young age under 36 months and the development of malformations. Furthermore, we can see a gap of root malformations for boys older than three years.
Conclusion
Children who received cancer therapy are at high risk for diverse dental damages. The main risk factor for malformations is an age below 36 months. Sex has an influence on the occurrence of root malformation in older children.
Highlights
- •
Chemotherapy has a strong impact on dental health.
- •
Malformation occurs independent on treatment duration and protocol.
- •
Age and sex influence the presentation of malformation.
1
Introduction
Pediatric cancer is rare but represents one of the most frequent fatal diseases in childhood. Over the last decades, the development of effective disease-specific treatments resulted in a remarkable survival rate. The current 5-year overall survival rate of malignant diseases in childhood has reached 80% in high-income countries [ , ]. However, since the number of children surviving cancer increases, focus needs to be directed to long-term side effects of various antineoplastic therapies. A child affected by cancer is at great risk for treatment-related late sequelae with potential impact on various organs, including the neurologic, cardiopulmonary or endocrine systems [ ]. Two-thirds of childhood cancer survivors (CCS) will develop at least one late-onset complication, and pediatricians developed guidelines for long-term follow-up care to optimise monitoring even in adulthood [ ].
Recurrent dental complications are brought in association with cancer therapy, but studies remain very limited. Accordingly, dental care is often not covered by health care insurance of pediatric oncology patients. The possible impact of chemotherapy and irradiation on oral health during treatment periods has been assessed in several studies [ , ]. CCS may have an increased risk of dental diseases after chemotherapy since permanent teeth are in an evolving developmental state when intensive chemotherapy was administered. A transient metabolic disturbance like chemotoxic stress can lead to abnormal tissue, which will be visible by an incremental line or more severe dental defects. Because of the metabolic stability of their structures, teeth can provide a permanent record of disturbances occurring during their development [ ]. Thus any effects of cytotoxic chemotherapy and irradiation on dental development would be recorded in the teeth developing at that time.
The most frequently reported oral manifestations of antineoplastic therapies are agenesis, microdontia, enamel hypoplasia, arrested root development, and tooth discolouration. These effects might have a considerable impact on the quality of life of CCS.
This study aimed to evaluate the frequency of dental abnormalities in CCS in Switzerland in comparison to healthy controls. Furthermore, we correlated the appearance of the central sequelae with the patients’ age at start of therapy and sex to define time windows of risk of tooth malformations.
2
Material and Methods
2.1
Study population
This retrospective study compares defects in dental structures in CCS to an equally sized, randomly selected control group. This study followed the code of ethics in the Declaration of Helsinki. Admission was obtained from the regional Ethics Committee, and informed consent was obtained from all participants or their legal guardians. All patients that underwent chemotherapy after the year 2000 and were not older than six years at the time of diagnosis were identified. Criteria for inclusion are: postpartum antineoplastic therapy until the age of six, no manifestations of tumors or metastases in the head/neck region and their medical records, dental history and dental imaging after antineoplastic therapy had to be accessible. Definition of sex is done by self-report. Patients who received radiotherapy in the head/neck region were excluded. Only CCS with a minimal age of 10 at time of data collection were included. For the control group, clinic’s database was queried for all patients aged 14–15 who had received at least one orthopantomogram. Subjects were randomly selected from this query, only adequate sex representation was ensured. Data were evaluated if image quality was satisfactory and transition from primary to permanent dentition had been completed.
2.2
Data collection and assessment
Information regarding treatment protocols, systemic medication doses, the use of stem cell transplant, or radiation therapy and localisation were protocolled. Dental case history, x-rays, and, if existent, photographs were evaluated. Radiographic films and oral photographs were digitised at 800dpi using an Epson Perfection v800-film scanner. Only permanent teeth were assessed. All entirely visible teeth on intraoral or extraoral x-rays were digitally measured inside the Rhinoceros CAD-software using the adapted Lind-method by Hölttä [ ] to determine the root-to-crown ratio. Values were not rounded. Tooth measurements were omitted if not all measuring points could be determined confidently or if the root did not show terminated apexification. All teeth were dichotomously assessed for malformations. Wisdom teeth were not evaluated. Data management and analysis were performed in IBM SPSS-26, Python-3.7, and R-Studio-1.2.5019.
3
Results
3.1
Patients
We identified 47 children, meeting our inclusion criteria (22 female, 25 male). The mean age at therapy start was 33.5 ± 22.4 months (range 1–81), and treatment duration was 486.7 ± 10.3 days (range 5–1679) ( Table 1 ). Acute lymphoblastic leukemia (49%, n = 23) and neuroblastoma (19%, n = 9) were most often diagnosed. The protocols most often used were ALL-BFM 2000 (32%, n = 15) and NB-2004 (11%, n = 5). Seven received radiation therapy (one female, six male), and five received stem cell transplants (two female, three male). Two sustained a relapse. Details are listed in Suppl. Table 1 . The control group consists of 22 female and 25 male patients.
| Characteristic | N | % | |
|---|---|---|---|
| Sex survivors | Male | 25 | 53.2 |
| Female | 22 | 46.8 | |
| Sex control | Male | 25 | 53.2 |
| Female | 22 | 46.8 | |
| Diagnoses | c-ALL | 12 | 25.5 |
| Pre-B-ALL | 2 | 4.3 | |
| T-ALL | 2 | 4.3 | |
| Not specified | 7 | 14.9 | |
| Neuroblastoma | 9 | 19.1 | |
| AML | 3 | 6.4 | |
| Nephroblastoma | 3 | 6.4 | |
| Rhabdomyosarcoma | 3 | 6.4 | |
| Wilms tumor | 2 | 4.3 | |
| Erwingsarcoma | 1 | 2.1 | |
| Fibromatosis | 1 | 2.1 | |
| Hepatoblastoma | 1 | 2.1 | |
| MDS | 1 | 2.1 | |
| Protocols | ALL-BFM 2000 | 15 | 31.9 |
| NB-2004 | 6 | 12.8 | |
| AEIOP-BFM 2009 | 5 | 10.6 | |
| SIOP 2001/GPOH | 4 | 8.5 | |
| NB97 | 3 | 6.4 | |
| AML-BFM 2004 | 2 | 4.3 | |
| AALL03 | 1 | 2.1 | |
| ALL-BFM 2004 | 1 | 2.1 | |
| CCG 106 | 1 | 2.1 | |
| CWS 2002 | 1 | 2.1 | |
| CWS guidance | 1 | 2.1 | |
| EpSSG RMS 2005 | 1 | 2.1 | |
| EuroWing99 | 1 | 2.1 | |
| HK-SG-ALL-97 | 1 | 2.1 | |
| HR-NBL1.5/GPOH | 1 | 2.1 | |
| SIOPEL III | 1 | 2.1 | |
| No strict protocol | 1 | 2.1 | |
| Mean | SD | ||
| Age at therapy start | (months) | 33.5 | 22.4 |
| Treatment duration | (days) | 486.7 | 331.6 |
3.2
Anomalies with relevant findings
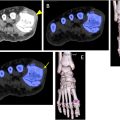
First, we analysed the distribution of anomalies by teeth, treating bilateral homonymous teeth as one variable ( Fig. 1 ). Aside from circular hypoplasia, all relevant anomalies can be observed in the survivor cohort and the control group. The control group presents mainly root dilacerations and slender roots. However, the incidences of all observed anomalies are considerably higher in the survivor cohort than in controls ( Table 2 , Suppl. Tables 1 and 2 ). An example of microdontia, shortened or slender roots and circular hypoplasia is given in Fig. 2 .

| Malformation | Patients | Teeth | ||||||
|---|---|---|---|---|---|---|---|---|
| Survivor group | Control group | Survivor group | Control group | |||||
| N | % | N | % | N | % | N | % | |
| Agenesis | 6 | 12.8 | 3 | 6.4 | 28 | 2.2 | 4 | 0.3 |
| Microdontia | 19 | 40.4 | 1 | 2.1 | 52 | 4 | 1 | 0.1 |
| Disturbed crown morphology | 10 | 21.3 | 3 | 6.4 | 26 | 2 | 3 | 0.2 |
| Circular hypoplasia | 9 | 19.1 | 0 | 0.0 | 50 | 3.9 | 0 | 0 |
| Slender root | 16 | 35.6 | 6 | 12.8 | 63 | 6.8 | 7 | 0.5 |
| Radiologically short root | 15 | 33.3 | 4 | 8.5 | 57 | 6.1 | 8 | 0.6 |
| Root dilaceration | 11 | 24.4 | 25 | 53.2 | 20 | 2.2 | 46 | 3.6 |
| Single-rooted molars | 8 | 17.8 | 4 | 8.5 | 10 | 1.1 | 6 | 0.5 |
| Restorations or visible caries | 11 | 23.4 | 6 | 12.8 | 28 | 3.3 | 15 | 1.2 |
| Taurodontism | 8 | 17 | 6 | 12.8 | 19 | 1.5 | 14 | 1.1 |
| Obliteration of the root canal | 0 | 0 | 0 | 0.0 | 0 | 0 | 0 | 0 |
| Lateral resorption of the root | 0 | 0 | 0 | 0.0 | 0 | 0 | 0 | 0 |
| Missing enamel | 1 | 2.1 | 0 | 0.0 | 1 | 0.1 | 0 | 0 |
| Gemination | 0 | 0 | 0 | 0.0 | 0 | 0 | 0 | 0 |
| Dens invaginatus | 0 | 0 | 0 | 0.0 | 0 | 0 | 0 | 0 |
| Failure of apexification | 0 | 0 | 0 | 0.0 | 0 | 0 | 0 | 0 |
| Denticles | 4 | 8.5 | 5 | 10.6 | 14 | 1.1 | 13 | 1 |
| Abnormal anatomy of the coronal pulp chamber | 2 | 4.3 | 0 | 0.0 | 2 | 0.2 | 0 | 0 |
| Accessory roots | 0 | 0 | 0 | 0.0 | 0 | 0 | 0 | 0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree