Neuroimaging is crucial for evaluating the craniocervical junction (CCJ), where pathologies are categorized into traumatic and nontraumatic. While traumatic conditions are more prevalent, nontraumatic abnormalities, though less common, carry significant morbidity and mortality and present a diagnostic challenge due to their diverse differential diagnoses. Nontraumatic CCJ abnormalities often necessitate careful diagnosis and management. Imaging plays a key role in identifying and characterizing these conditions, aiding clinical decisions. Nontraumatic CCJ abnormalities include various conditions, such as congenital anomalies, tumors, inflammatory conditions, degenerative changes, and infections. This review highlights the imaging features of common nontraumatic CCJ abnormalities, emphasizing key imaging characteristics for differentiation.
Key points
- •
Nontraumatic pathologies of the craniocervical junction (CCJ) carry significant morbidity and require accurate imaging for diagnosis.
- •
Tumors at the CCJ are categorized as intramedullary, intradural extramedullary, and extradural lesions, with metastases being the most common neoplastic condition in this region.
- •
MRI is the preferred modality to identify classic spinal patterns, like adjacent vertebrae and disc involvement in spinal infections, or disc preservation in spinal tumors.
| AAS | atlantoaxial subluxation |
| AS | ankylosing spondylitis |
| CCJ | craniocervical junction |
| CSF | cerebrospinal fluid |
| CT | computed tomography |
| DISH | diffuse idiopathic skeletal hyperostosis |
| NF2 | neurofibromatosis type 2 |
| NPC | nasopharyngeal carcinoma |
| OA | occipitoatlantal |
| OA | osteoarthritis |
| OPLL | ossification of the posterior longitudinal ligament |
| T1W | T1 weighted |
| T2W | T2 weighted |
Introduction
Neuroimaging is crucial for evaluating the craniocervical junction (CCJ), where pathologies are categorized into traumatic and nontraumatic. While traumatic conditions are more prevalent, nontraumatic abnormalities, though less common, carry significant morbidity and mortality and present a diagnostic challenge due to their diverse differential diagnoses. Nontraumatic CCJ abnormalities often necessitate careful diagnosis and management. Imaging plays a key role in identifying and characterizing these conditions, aiding clinical decisions.
Nontraumatic CCJ abnormalities include various conditions, such as congenital anomalies, tumors, inflammatory conditions, degenerative changes, and infections. This review highlights the imaging features of common nontraumatic CCJ abnormalities, emphasizing key imaging characteristics for differentiation. It organizes these abnormalities by their underlying pathophysiology, providing a structured approach to understanding them.
Anatomy
CCJ is formed by the occipital bone and the first two cervical vertebrae, C1 and C2. The occipital condyles are bony projections emerging from the external aspect of the occipital bone, defining the lateral edges of the foramen magnum with the basiocciput anteriorly and the supraocciput posteriorly. These condyles articulate with the superior articular surfaces of the lateral masses of the atlas. Variations such as precondylar tubercles or third occipital condyles may also be present.
The atlas (C1) is unique as it is the only vertebral segment that lacks a body, a spinous process, and an intervertebral disc. It consists of paired bilateral lateral masses joined by anterior and posterior arches and articulates superiorly with the occipital condyles and inferiorly with C2, forming the atlanto-occipital and atlantoaxial joints, respectively.
The axis (C2) is characterized by its prominent odontoid process, or dens, which projects upward and provides a pivot for the atlas and skull to rotate. It typically has a bifid spinous process that attaches to the ligamentum nuchae and surrounding muscles.
A complex network of ligaments stabilizes the CCJ, limiting excessive movement and protecting neural structures passing through this region. These ligaments are classified as extrinsic and intrinsic ( Figs. 1 and 2 ).


The intrinsic ligaments , located anterior to the dura mater, are the most important ligaments for CCJ stability. They include the tectorial membrane, the cruciform ligament, and the odontoid ligaments (apical and alar ligaments). The odontoid ligament comprises the apical and alar ligaments; the latter limits axial rotation and maintains head and neck alignment. The cruciform ligament, consisting of a horizontal band (transverse ligament) and longitudinal bands including the superior and inferior longitudinal fibers, divides the atlas into anterior and posterior compartments and stabilizes the dens to the atlas. The tectorial membrane continues from the posterior longitudinal ligament and extends from the body of C2 to the occipital bone, forming the posterior border of the supraodontoid space.
The extrinsic ligaments include the anterior and posterior atlanto-occipital membranes and the nuchal ligament. They extend from the CCJ to the cervical spine; these ligaments are continuations of the anterior longitudinal ligament and ligamentum flavum. The anterior atlanto-occipital membrane attaches the anterior aspect of the atlas to the foramen magnum, while the nuchal ligament extends from the C7 vertebra to the occipital bone, restricting hyperflexion and providing proprioceptive feedback. The posterior atlanto-occipital membrane extends from the posterior arch of the atlas to the foramen magnum, providing structural support, and limits excessive flexion and extension at the atlanto-occipital joint. It also protects neural structures, including the spinal cord and cervical spinal nerves, during head and neck movements.
Mechanical stability of the CCJ is primarily maintained by the occipitoatlantal capsular ligaments (OACLs), which are the dominant stabilizers of the occipitoatlantal (OA) joint. Finite element analysis shows that OACL injury causes the largest increase in range of motion, particularly in lateral bending and axial rotation, compared to injuries of other ligaments such as the transverse ligament or tectorial membrane.
Muscles associated with the CCJ include the prevertebral muscles, such as the longus capitis and longus colli, which stabilize the cervical spine and facilitate head and neck movements. The suboccipital muscles, including the rectus capitis posterior major and minor and the obliquus capitis superior and inferior, support head extension, rotation, and lateral bending. These muscles delineate the suboccipital triangle, through which the vertebral arteries and occipital nerves pass.
Congenital anomalies
Congenital anomalies of CCJ are uncommon and clinically significant, as they can mimic other pathologic conditions. Radiologists must accurately distinguish these anomalies, which requires an understanding of their developmental origins. Pang and Thompson categorize them into two primary groups: anomalies of the central pillar and anomalies of the surrounding rings, each reflecting specific embryologic disruptions that manifest in characteristic ways ( Fig. 3 ).

Anomalies of the central pillar involve disturbances in the axial components of the occipital sclerotomes, proatlas, and C1–C2 sclerotomes, often resulting in craniocervical instability and neural impingement. These anomalies are divided into odontoid dysgeneses, which primarily affect the dens and axis complex, and basioccipital dysgeneses, which impact the basiocciput and its relationship with the skull base.
Os odontoideum is a CCJ anomaly characterized by a round or oval ossicle at the tip of a hypoplastic odontoid process ( Fig. 4 ). Its etiology is debated, potentially congenital or resulting from trauma before skeletal maturity. It is associated with syndromes like Morquio’s disease, Down syndrome, and achondroplasia. Initial evaluation with plain radiographs assesses atlantoaxial instability. Computed tomographic (CT) scans provide detailed bony anatomy, differentiating Os odontoideum from odontoid fractures or other anomalies, while MR imaging assesses soft-tissue and spinal cord involvement. Differential diagnoses include persistent ossiculum terminale and type 2 odontoid fracture ( Fig. 5 ), which demonstrates irregular lucent margins and variable morphology ( Table 1 ).


| Os Odontoideum | Os Termianle Persistens | Odontoid Fracture Type 1 | Odontoid Fracture Type 2 | |
|---|---|---|---|---|
| Location | Base of the dens | Tip of the dens | Tip of the dens | Base of the dens |
| Morphology | Round or oval | Triangular | Irregular/variable | Irregular/variable |
| Margins | Smooth, well corticated | Smooth, well corticated | Lucent/irregular | Lucent/irregular |
| Clinical findings | Incidental/asymptomatic, from neck pain to neurologic deficits | Incidental/asymptomatic | History of trauma, from neck pain to neurologic deficits | History of trauma, from neck pain to neurologic deficits |
| Atlantoaxial instability | Common | Rare | Variable | Variable |
| Additional features | Hypertrophy of the anterior arch of C1, hypoplastic base of the dens | Underlying V-shaped cartilaginous cleft | Multiple adjacent fractures and soft tissue injury | Multiple adjacent fractures and soft tissue injury |
Ossiculum terminale persistens results from the failure of fusion between the secondary ossification center at the tip of the odontoid and the rest of the odontoid process after puberty. , It is generally asymptomatic and considered a normal variant unless it persists beyond skeletal maturity, potentially contributing to atlantoaxial instability, particularly in individuals with Down syndrome. On imaging, it appears as a well-corticated triangular structure with smooth margins at the tip of the dens, sometimes with an underlying V-shaped cartilaginous cleft. Differential diagnoses include Os odontoideum and type 1 odontoid fractures (see Table 1 ).
Platybasia is characterized by abnormal flattening of the skull base. It is defined by a basal angle greater than 143°, measured using traditional landmarks: a line from the nasion to the pituitary fossa and another from the anterior border of the foramen magnum to the pituitary fossa. A modified technique, which uses landmarks across the anterior cranial fossa and clivus, provides more reproducible and often lower basal angle measurements compared to the conventional approach. When associated with basilar invagination, characterized by the abnormal displacement of the odontoid process into the foramen magnum, it can cause brainstem compression and neurologic symptoms ( Fig. 6 ). The condition can be congenital, associated with disorders such as osteogenesis imperfecta, or acquired from conditions like trauma. ,

Atlanto-occipital assimilation occurs when the atlas fuses with the occiput. The condition can be complete or partial, often reducing the size of the foramen magnum and possibly causing brainstem or spinal cord compression ( Fig. 7 ). This condition is frequently associated with other CCJ anomalies, including basilar invagination and Chiari malformation.

Tumors
Tumors affecting the CCJ are rare, with metastatic lesions being more prevalent than primary tumors. On the other hand, in the pediatric population, atlantoaxial involvement is more frequent and predominantly benign. Tumors in this region pose unique diagnostic and therapeutic challenges due to the anatomic complexity and risk of craniocervical instability. Differentiating these tumors is facilitated by focusing on their anatomic origin, classifying them as intramedullary, intradural extramedullary, or extradural ( Fig. 8 ). MR imaging is the primary imaging technique for diagnosing intramedullary and intradural extramedullary tumors, while CT is preferred for evaluating osseous spinal tumors.

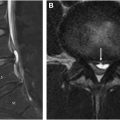
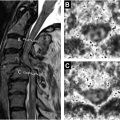
Intramedullary tumors typically appear on MR imaging as spinal cord widening with narrowing of the cerebrospinal fluid (CSF) column on T2-weighted (T2W) images. Gadolinium is particularly useful for evaluating these tumors, which may also be associated with syringomyelia or cyst-like lesions.
Intradural extramedullary tumors displace the spinal cord contralaterally, widen the CSF space above and below the tumor, and show a sharp demarcation between the tumor and CSF.
Extradural tumors on MR imaging compress the thecal sac away from the lesion, flatten the cord, and display an eccentric tumor origin.
Intramedullary Tumors
Intramedullary tumors account for 16% to 25% of primary spinal neoplasms and arise from parenchyma of the spinal cord or nerve root. Approximately 80% of intramedullary spinal cord tumors are gliomas, which include astrocytomas and ependymomas. Astrocytomas are more common in children, while ependymomas are more frequent in adults.
Ependymomas and astrocytomas both span multiple vertebral segments and exhibit hypo/iso-intensity on T1 weighted (T1W) and are hyperintense on T2W, with contrast enhancement. Ependymomas typically span 3 to 4 vertebral bodies, are centrally located, cause symmetric spinal cord expansion, and display diffuse enhancement with clear borders. Astrocytomas, on the other hand, often span 5 to 6 vertebral bodies, are more eccentrically located, may show no enhancement or have an enhancing nodule or large satellite cysts, and generally lack well-defined borders. Intratumoral hemorrhage can occur in both, though it is more common in ependymomas, often presenting as a cap sign on MR imaging. ,
Hemangioblastomas are the third most common intramedullary tumors. These highly vascular lesions typically cause diffuse spinal cord enlargement and are located peripherally. On MR imaging, they show robust contrast enhancement and often display flow voids. Entire neural axis imaging is recommended to detect multiple lesions, as they may be associated with von Hippel-Lindau syndrome ( Table 2 ).
| Astrocytoma | Ependymoma | Hemangioblastomas | Metastasis | |
|---|---|---|---|---|
| Epidemiology | Common in children, in adult the peak incidence is fourth decade | Common in adults, third decade, more common in male | Peak presentation in the fourth decade | Mean age 55 y |
| Common location in the spinal cord | Thoracic, 5–6 vertebral bodies, involvement of the entire cord diameter | Cervical, 3–4 vertebral bodies | Thoracic | Cervical Usually solitary 2–3 vertebral body segments |
| MR imaging findings | ||||
| Location | Eccentric | Central location | Eccentrically and exophytic component | |
| Border | Ill-defined border | Well circumscribed | Discrete nodules and can have diffuse enlargement of the spinal cord | Well defined |
| Cyst | Cysts are less common | Cysts are less common | Tumor cysts are common | In contrast to primary intramedullary neoplasms, associated cysts are rare |
| Hemorrhage or flow void | Uncommon | More common (cap sign) | Focal flow voids | |
| Peritumoral edema | ∼40% | 60% | Common | Common |
| Enhancement | Patchy enhancement pattern, sometimes, non-enhancing | Diffuse enhancement with a clear border | Vivid enhancement | Avid enhancement, rim sign enhancement, ill-defined enhancement extending above and/or below the lesion (flame sign) |
| Other | Scoliosis and bony remodeling less common | Scoliosis and bony remodeling more common | Should be taken to image the whole neuraxis to ensure that no other lesions are present. | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree