Ankle Fractures and Dislocations
The ankle is the most commonly injured weight-bearing joint of the body,1 and most orthopedic surgeons routinely treat these injuries. A great deal has been written regarding the diagnosis and treatment of ankle fractures, although controversy persists regarding some aspects of their treatment.2–5 The ankle joint may be injured as the result of direct or more often indirect trauma (rotational, translational, or axial forces). These injuries often result in variable amounts of subluxation or dislocation of the talus from the mortise of the distal tibia and fibula. It was originally shown by Ramsey and Hamilton6 that mild malalignment of the ankle joint leads to abnormal pressure distribution and loading of the articular cartilage, potentially increasing the risk of subsequent arthritis. Generally, a good outcome might be expected if a congruent reduction of the ankle, through closed or open means, can be obtained and maintained. Mont and associates7 found that residual radiographic abnormalities after ankle fracture surgery, especially if multiple, correlated with poorer clinical outcomes. Thus, the goals of treatment for ankle fractures and dislocations are a stable congruent joint that enables early ankle mobility, fracture healing, and, ultimately, the prevention of arthritis. The decision for operative or nonoperative treatment of these injuries depends on whether the risks and benefits of open treatment are expected to provide improved results compared to closed treatment.
This chapter discusses the practical operative management of ankle fractures, including surgical indications, operative methods and technical pearls, and pre- and postoperative management, based on the available literature and the authors’ experiences.
Fracture Assessment and Decision Making
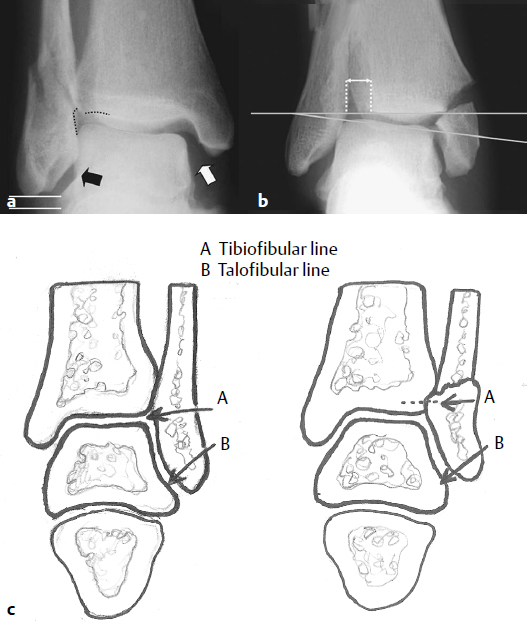
The standard radiographic assessment of the ankle includes three views: anteroposterior (AP), mortise (15- to 20-degree internal rotation), and lateral (Fig. 35.1). With significant injury to the ankle, a consistent pattern of in stability occurs, specifically lateral translation and external rotation of the talus relative to the tibial plafond. Radiographic findings of obvious ankle instability may include significant fracture displacement, subluxation or dislocation of the talus under the plafond, and widening of the medial joint space. Radiographic findings sometimes may be more subtle. Other radiographic clues that significant injury has occurred include alterations in the talocrural angle, talar tilt, widened tibiofibular clear space, loss of alignment of the subchondral plates at the tibiofibular line, and shortening of the fibula by loss of parallelism of the subchondral lines of lateral malleolus and that of the lateral talus8,9 (Fig. 35.2).

At times, a fracture of the lateral malleolus may be accompanied by an injury to the deltoid ligament. Recent work has demonstrated that soft tissue findings such as medial ankle pain and swelling are not reliable predictors of ankle instability associated with a supination/external rotation fracture of the distal fibula.10,11 Radiographic findings may also not clearly demonstrate the instability of this injury, and an AP or mortise stress view of the ankle taken while external rotation force is applied may be helpful in revealing lateral talar subluxation and associated medial joint space widening. Michelson and associates12 advocated a gravity stress test as being effective but less painful for the patient compared with other dynamic tests (Fig. 35.3). Using this method, the lateral side of the ankle is placed down on the table with the majority of the ankle off the edge of the table. A cross-table mortise view radiograph is taken. A positive stress test shows medial clear space widening relative to the nonstressed radiograph.

Similarly, syndesmosis injuries may be obvious with widening of the distal tibiofibular joint, or they may be very subtle. Although the level of the fibular fracture may be used to assess the likelihood of syndesmosis injury,13 it has been found that syndesmosis instability can accompany more distal Weber type B fractures.14 A few imaging methods can demonstrate radiographically subtle syndesmosis instability. The external rotation stress test described above for ankle instability can also be used to evaluate competency of the syndesmosis. Candal-Couto and associates15 demonstrated that disruption of the syndesmosis causes even more displacement in the anteroposterior (sagittal) plane than in the coronal plane, and suggested that stress views evaluating anteroposterior displacement of the fibula relative to the tibia may be an even more sensitive indicator of syndesmosis injury. In the case of a more proximal fibula fracture without a medial fracture, a positive stress test likely indicates the presence of a combined deltoid and syndesmosis injury.
The treatment of ankle fractures with special circumstances, including open fractures and those in patients with diabetes mellitus or osteoporosis, is discussed later in the chapter.
Classification
Optimally, a classification system should guide treatment decisions and provide insight into prognosis. The two most commonly used classification systems for ankle fractures are the Danis-Weber5 and Lauge-Hansen16,17 systems (Fig. 35.4). Although orthopaedic surgeons commonly use both systems, neither is perfect, and their interobserver reliability is unsatisfactory.18 The Danis-Weber system is based on the level of the fibula fracture and is divided into three types: type A fibula fractures occur below the level of the tibial plafond; type B fractures typically rise obliquely from the level of the plafond; and type C fractures are centered well above the plafond. Typically, type C injuries have an associated syndesmotic injury. Although this system is relatively straightforward, it does not provide any guidance regarding treatment of a medial injury, options for fixation (except for the syndesmosis), and prognosis. The Lauge-Hansen system is based on the mechanism of injury and is more encompassing than the Danis-Weber system. It describes the typical medial injuries and proposes likely reduction maneuvers, which are of prime importance for nonoperative management of ankle fractures.
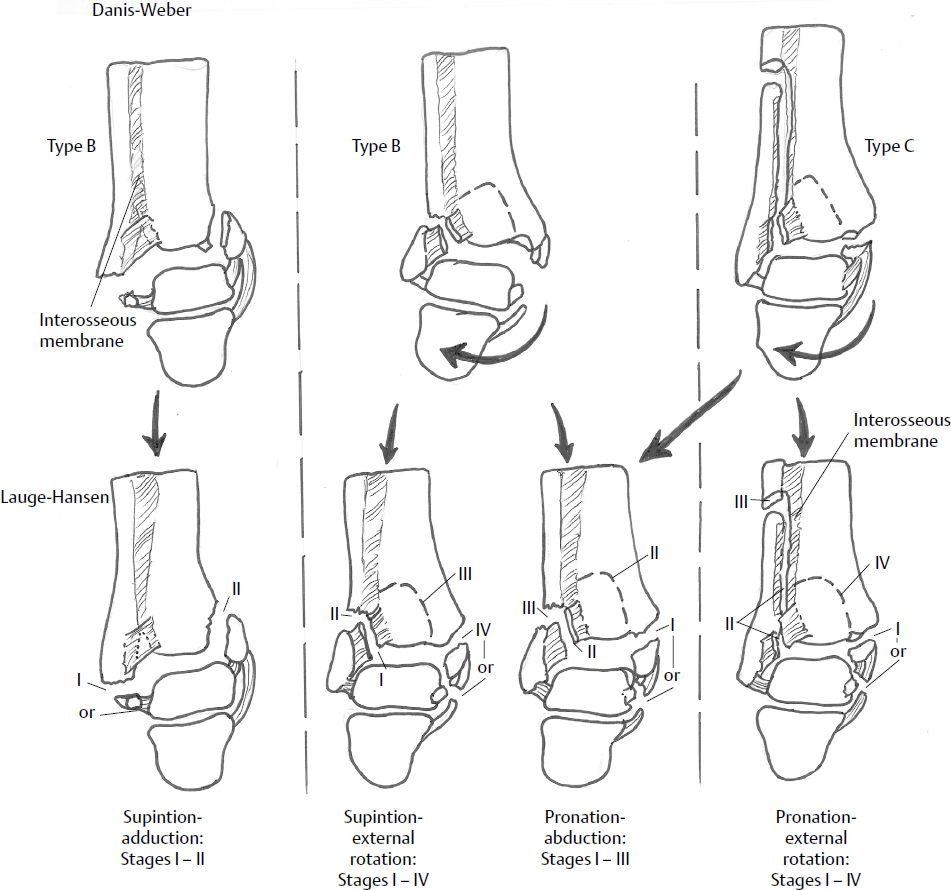
The Lauge-Hansen system has been criticized for having less relevance to the surgical treatment of these injuries. It is based on two terms: the first describes the position of the foot at the time of injury, and the second describes the direction of the force causing the injury. The position of the foot at the time of injury dictates which structures are taut and thus likely to fail at the onset of deformation. According to this system, there are four common types of ankle fractures: supination–external rotation injury (S-ER), supination-adduction (S-AD), pronation–external rotation (P-ER), and pronation-abduction (P-AB). S-ER is the most common type (up to 85% of fractures) and includes an oblique or spiral fracture of the fibula along with a variable medial injury.
This chapter discusses the operative treatment of ankle fractures and dislocations based on anatomic location (medial, lateral, posterior, and syndesmosis), but includes and integrates both ankle fracture classification systems into the discussion. Dislocations of the ankle are typically described by the direction of the dislocated talus. Using this system, though, little useful direction as to operative treatment or prognosis is attainable.
Nonoperative Treatment
The goals of treatment for ankle fractures and dislocations are the maintenance of a stable, congruent joint that enables early joint mobility, fracture healing, and ultimately the prevention of arthritis. Fortunately, many minor ankle fractures are functionally equivalent to lateral ankle sprains, consisting of a stable, isolated lateral malleolus fracture that will lead to a good outcome if treated nonoperatively.
If a closed reduction is determined to be adequate, with a medial clear space within 4 mm of the uninjured ankle and/or less than 2 mm of malleolar displacement,1 the patient may be treated with cast or splint immobilization and serial examinations. However, it may be very difficult to maintain the ankle in a reduced position with casting for two reasons. First, radiographic criteria can be misleading, because they are based on two-dimensional static representation of a three-dimensional dynamic joint. Second, the ability of a cast to hold the reduction is reduced as limb swelling diminishes with time, thus reduction may be lost even if diligent care is provided. Fractures that are often stable enough for nonoperative treatment include most of the Weber type A fractures, as well as some of the Weber type B fractures, including low-grade Lauge-Hansen S-AD or S-ER fractures (types 1 and 2).
Surgical Treatment
Indications
Traditionally, closed reductions have been considered unsatisfactory if radiographs showed a medial clear space greater than 4 mm or more than the opposite normal side, or a displacement of the medial or lateral malleolus greater than 2 mm.1 If closed reduction is inadequate or expected to be inadequate in accomplishing the desired goals, surgical treatment should be considered. General guidelines recommend surgical treatment for the following ankle fractures3,5,19:
Surviving the Night
Fracture-dislocations or subluxations of the ankle must be reduced immediately because excess pressure on the skin may cause necrosis or convert a closed fracture to an open one. Even a small amount of residual lateral subluxation of the talus can cause pressure necrosis of the medial ankle. A well-padded posterior and U-shaped splint is then applied to maintain reduction. The supramalleolar skin over the medial distal tibia is most often at risk, as subluxation of the talus and malleoli typically occurs laterally. Loss of reduction may occur relatively early as swelling resolves and the splint no longer fits well.
The treatment of patients who have open ankle fractures begins upon arrival at the emergency room with the administration of intravenous antibiotics and tetanus prophylaxis. The wound should be examined and then covered with a saline moistened sterile dressing. The open fracture is typically an 8- to 12-cm transverse supramalleolar wound that probably results from some element of tension force. Upon arrival at the emergency room, the injury is usually still grossly displaced and a reduction maneuver should be performed early to prevent further injury. If gross contamination of the wound is present, brief irrigation of the wound may be helpful prior to reduction and application of a well-padded splint. Antibiotics should be provided according to current recommendations for open fractures. For example, patients who have Gustilo type I and II fractures should receive a cephalosporin (e.g., cefazolin) on admission, which is continued every 8 hours for at least 24 to 48 hours. Patients who have type III fractures should receive the same dose of a cephalosporin plus an aminoglycoside, a broad-spectrum antibiotic (Zosyn), or fluoroquinolone for gram-negative coverage. Patients with farm injuries or grossly contaminated wounds should also receive penicillin.20
Urgent wound debridement and lavage is mandatory. An aggressive and organized surgical debridement is performed to remove all foreign material and tissue of questionable viability. The one exception to aggressive debridement may be an elderly patient with low-energy injury and very thin skin, which is a common scenario in open ankle fractures. This patient may not be a candidate for free soft tissue transfer, and thus a less aggressive skin debridement should be considered so that the wound has a chance to be closed. Once the wounds have been irrigated, the surgeon may proceed with either formal open reduction and internal fixation (ORIF) or, if this is not appropriate because of the severity of bone or soft tissue injury, ankle-spanning external fixation.
Weber type A and S-AD fractures associated with a medial injury
Weber type B and S-ER and P-AB fractures that occur as part of a more complex bimalleolar, trimalleolar, or bimalleolar equivalent fracture (fibular fracture with incompetent deltoid ligament)
Weber type C and P-ER type 2 and 3 fractures, because of the syndesmosis injury and associated instability
Open ankle fractures
Ankle fracture-dislocations with more extensive bone and soft tissue injury
Functional and Surgical Anatomy
The ankle joint consists of the articulation of three bones (tibia, talus, and fibula) that move relative to one another and are restrained by three ligament complexes (Fig. 35.5). The ankle joint relies on these bones and soft tissues to maintain stability and alignment, while enabling the motion necessary for gait. Normally, the talus sits in the ankle “mortise,” articulating with the weight-bearing tibial plafond, as well as the articular facets of the medial and lateral malleoli. In the neutral position, 90% of the weight borne across the ankle joint passes through the tibial plafond.21 Most of the ankle′s motion involves dorsiflexion and plantarflexion of the foot relative to the leg. However, when viewed from above, the talus is trapezoidal in shape, and thus with ankle dorsiflexion there is also widening of the mortise and external rotation of the fibula.22 The ankle might best be regarded as a complicated hinge.

The bony ankle is maintained by three sets of ligaments: the tibiofibular “syndesmosis” and the lateral and medial ankle ligament complexes (Fig. 35.5). The distal tibia and fibula are held together by the syndesmosis or inferior distal tibiofibular ligament complex. The syndesmosis maintains the ankle mortise and consists of four ligaments: the anterior and posterior inferior tibiofibular ligaments, the inferior transverse tibiofibular ligament, and the interosseous ligament. The lateral ankle ligament complex includes three distinct elements that fan out from the lateral fibula to attach to the lateral hindfoot: the anterior talofibular ligament, the calcaneofibular ligament, and the posterior talofibular ligament. Medially, the major ligament is the deltoid, which originates from the medial malleolus and includes a superficial component that inserts on the calcaneus, and a deep component that inserts on the talus.23 An injury to any of the three ligament complexes of the ankle, as well as the bony structures, can result in an unstable ankle joint. It is important to understand the anatomy, as it is usually a combination of bony and ligamentous injury that will render an ankle unstable and require surgical stabilization.22–25
There is a relatively thin soft tissue envelope around the ankle, which may be quite fragile in some patients. Additionally, many tendons and neurovascular structures cross the ankle joint. Due to the paucity of protective soft tissues and local blood supply to these tissues, soft tissue problems or wound complications are not uncommon after an ankle injury or subsequent surgery. Considerations regarding the timing of surgery and soft tissue management are therefore critical in minimizing the risks of perioperative complications, and are discussed at length in this chapter.
Timing of Surgery
The timing of surgery is somewhat controversial, but ultimately depends on the condition of the soft tissues. Several authors have suggested that surgery is best performed within 6 to 8 hours of injury, before significant edema develops.26,27 However, the logistics of performing early surgery may be difficult. Generally, most experts agree that swelling and edema should be controlled before surgery is undertaken in order to minimize the risk of soft tissue complications. Marked swelling, the presence of fracture blisters, or other skin changes should delay surgery until the soft tissues have had time to recover. In this situation, the fracture must be reduced and held in a well-padded splint, cast, or even in an external fixator, and the limb must be elevated. Most ankle fractures can undergo surgical treatment with no change in technique or complication rates up to 3 weeks after the injury.
Examination
Assessment of the soft tissues and the decision regarding timing of ankle fracture surgery are among the most important decisions a surgeon makes in these cases. Blisters, considerable swelling, or other signs of soft tissue trauma should alert the surgeon to delay surgery until these issues resolve. The “wrinkle” sign has been used in other areas of the lower extremity and may be helpful for deciding when the soft tissues are ready for ankle fracture surgery. Deformity from an ankle fracture-dislocation may cause pressure necrosis of the skin over the supramalleolar area. For this reason, if surgery is not to be performed immediately, a closed reduction should be performed and a splint applied that will maintain reduction of the talus beneath the plafond and decompress the skin “at risk.” The patient needs a thorough lower extremity exam despite the obvious ankle fracture. The limb should always be checked proximally for tenderness over the fibula (Maisonneuve fracture), along with examination of the Achilles tendon and foot for associated injuries. Medial tenderness in the ankle with no fracture should alert the surgeon to the likelihood of a deltoid injury and the possibility of an unstable ankle, although such injury can exist even without positive clinical findings.
Implants
In most cases, we use a small fragment set with a one-third tubular plate laterally, and 4.0- or 4.5-mm partially threaded cancellous screws (cannulated or solid) medially. The one-third tubular plate has been a workhorse plate for distal fibula and other ankle fractures, as it easily contours to the local anatomy, has a low profile, and enables ample mechanical strength for most fractures. Newer plates, however, may be beneficial in some particular cases. “Composite” plates that are one-third tubular distally and 3.5 mm proximally (DePuy, Warsaw, IN) may be useful in patients with poor bone quality or in cases with proximal fracture extension. Locking plate technology may also be useful in some difficult ankle fractures. These plate-screw devices create a fixed angled construct and may be beneficial in patients with poor bone quality and fracture comminution. Care must be taken when using locking plates around the ankle, however; if they are not placed in a lag fashion like traditional nonlocked plates, they are not useful for aiding in reduction. Rarely, intramedullary devices are used to control fractures of the distal fibula, and tension band wire techniques are sometimes useful medially or laterally for highly comminuted, distal fractures that require fixation.
A new alternative treatment implant is the fibular nail with interlocking screws (e.g., Acumed, Hillsboro, OR). These devices enable fixation in the distal fragment of the lateral malleolus, syndesmotic screw fixation through the nail, and target-guided screws proximal to the nail. The proximal screw is placed immediately adjacent to the nail, maintaining length by blocking shortening. The only way this implant maintains rotational control is with mandatory placement of a syndesmotic screw.28 A recent randomized study in patients over the age of 65 years showed fewer soft tissue complications and equivalent functional outcomes treated with nails compared with patients treated with traditional one-third tubular plate constructs.28
Preoperative Care and Planning
The importance of preoperative planning cannot be overemphasized. This is especially true for injuries around the ankle, for which multiple surgical incisions are often required and the injuries and soft tissues provide little leeway for surgical mistakes. Forethought as to which injury may need surgical treatment and what approaches may optimally provide access to each injury is typically time well spent.
Planning of reduction and implants begins with high-quality radiographs. On occasion, comparison views of the contralateral ankle may be helpful. Rarely, computed tomography (CT) may be indicated to judge the size and position of a posterior malleolar fragment, or involvement of the distal tibiofibular joint.
Operative Setup
Patients undergoing ankle fracture surgery are typically administered general or spinal anesthesia. Local anesthesia and sedation may be used on occasion, but they provide incomplete muscle relaxation, which may make fracture reduction difficult. A popliteal block administered preoperatively is a useful tool in the treatment of ankle fractures. This regional block can give excellent postoperative pain control for the lateral side of the leg when given as a onetime bolus, or as an indwelling catheter.
For patients being treated for injuries of the medial or lateral ankle, positioning is usually supine on a radiolucent operating table. It is often helpful to place a padded bump behind the buttock on the injured side to internally rotate the leg and provide comfortable access to the lateral malleolus. A well-padded thigh tourniquet is used to provide a dry surgical field. Two pillows or a foam base (or later a sterile towel roll) is placed under the fractured leg to elevate it above the contralateral leg; this assists in the surgical approaches and in obtaining lateral radiographs. A surgical prep of the limb is performed, and a preoperative dose of antibiotic is administered prior to exsanguination of the leg and insufflation of the tourniquet.
Postoperatively, wound closure is performed in a multilayer fashion. Obtaining soft tissue coverage over the lateral fibular plate with a full-thickness layer of soft tissue is desired. The subcutaneous tissues and skin are closed with atraumatic technique. Again, these tissues may have little physiological reserve, and wound problems around the ankle are rarely easily treated. We prefer not to use staples on the skin around the foot or ankle, but instead use 4-0 nylon sutures that can be carefully tensioned.
Isolated Lateral Malleolus Fractures
The importance of reduction of the lateral malleolus and its impact on overall ankle joint congruency and mechanics has been well recognized.6,29 Yablon and associates29 concluded that the lateral malleolus was the key to the anatomic reduction of bimalleolar ankle fractures, because the displacement of the talus faithfully followed the displaced distal fibular fragment. This concept has been challenged by Tornetta,30 who demonstrated that medial-only fixation is sufficient in many bimalleolar injuries.
Good results are typically achieved with nonoperative treatment of isolated lateral malleolus fractures when not accompanied by a medial injury.19 These clinical results are supported by cadaveric studies, which have shown that isolated displacement of the lateral malleolus does not cause ankle instability.21,31 The literature supports nonoperative treatment for less than 2 mm of displacement of the lateral malleolus and a normal medial clear space.6,32 For patients who have a closed, isolated lateral malleolus fracture with minimal displacement, we recommend nonoperative treatment with close follow-up.
Diagnosis of an associated deltoid ligament injury is not always easy. Medial tenderness and swelling may indicate a deltoid ligament injury, but clinical findings of a medial injury are occasionally quite subtle. Initial radiographs must be carefully scrutinized for widening of the medial joint space, which indicates incompetence of the deltoid ligament. Other methods of diagnosis include a variety of stress tests (described earlier in this chapter) and magnetic resonance imaging (MRI).
Technique of Fibular Plating
A direct lateral approach using a longitudinal incision is commonly used for the reduction and plating of fibula fractures (Fig. 35.6). The fibula is usually palpable beneath the subcutaneous tissues and its borders can be defined fairly easily. At times, the skin incision may be moved posteriorly (or anteriorly) depending on the soft tissues, site of plate placement, desire to access the postero- and antero-lateral tibia, or other reasons. The skin incision for posterior application of an antiglide plate is probably best modified by moving it 1 cm posteriorly to prevent soft tissue impingement during surgery. Additionally, the path of the superficial peroneal nerve is not always consistent, and meticulous dissection is required to assess whether the nerve is crossing through the operative wound, especially as the incision is carried proximally (Fig. 35.6).

Most lateral malleolar fractures that require open reduction and internal fixation (ORIF) are repaired with a pre-bent one-third tubular plate with or without lag screws. The plate can be applied directly laterally or posteriorly (Fig. 35.7). A laterally applied plate may result in occasional problems with implant prominence, but this position does provide more direct access for plate application. We prefer to apply a posterior antiglide plate for oblique fractures whenever possible. This technique may be more mechanically effective than lateral plating, and it minimizes the risk of implant problems (as long as the plate is not placed far distally impinging on the fibula′s peroneal groove).33,34 If the first screw is placed just above the apex of the fracture, the plate aids in the reduction by pushing the fracture into position (Fig. 35.8). A lag screw can then usually be placed through the plate to further increase fixation strength (Figs. 35.7b and 35.8b).


Simple fibular fracture patterns, such as the typical oblique or spiral fracture of an S-ER type 4 injury, are relatively easy to reduce. The fracture can be “freshened” by removing the organized fracture hematoma from the fracture line that may prevent interdigitation of the fracture′s bony interstices. One or two small pointed reduction or “lion-jaw” clamps can be used to restore length, translation, and rotation of the fibula. Fracture reduction can be judged by visualizing the proximal fracture spike and ensuring that it is keyed in at the fracture′s apex. As noted, a one-third tubular plate can be applied laterally or posteriorly for fixation. A lag screw can be applied before plating if a lateral plate is used, or through the plate if an antiglide plate is placed posteriorly.
Comminuted or “crushed” lateral malleolus fractures may be much more difficult to properly reduce and fix. Attention must be paid to restoring proper length and rotation across the fracture. These deformities are restored when the subchondral contour of the lateral talus matches that of the medial distal fibula, and the tibiofibular line is restored on the mortise view (Figs. 35.1 and 35.2). Useful techniques for gaining reduction include indirect reduction methods. For example, the plate can be used as an indirect reduction tool.35 Using this technique, the plate is initially applied to one side of the fracture (usually distal) and then length and rotation may be obtained using manual traction/manipulation, a mini-distractor, or the use of lamina spreaders against a “push-pull” screw. The plate is then temporarily secured to the bone proximally with a Verbrugge or other clamp, and the ankle imaged. The construct can be manipulated as necessary until an acceptable alignment is achieved, and then the plate may be secured proximally with screws.
An alternative method is to use a pointed reduction clamp to carefully correct rotation and bring the fibula out to length.36 One or two small Kirschner wires (K-wires) can then be used to pin the fibula to the talus or distal tibia. A plate can then be applied and the K-wires removed. Radiographs are then checked, and if an acceptable reduction is confirmed, a plate can be definitively fixed to the bone with screws. We typically use a stiffer plate, such as a well-contoured 3.5-mm dynamic compression plate (Synthes USA, Paoli, PA) or “composite” plate (DePuy-Ace, Warsaw, IN) in cases where there is considerable fracture shortening, comminution, or a more proximal diaphyseal injury. These more rigid plates must be carefully precontoured to include the anatomic rotation of the distal fibular shaft or they may tend to malreduce the fracture as the bone moves to the plate during screw insertion.
Tips and Tricks
After fixation of most unstable ankle fractures, stress views of the ankle should be performed to search for syndesmosis injuries.
A fracture of the fibula cannot be reduced with the aid of a locked plate and all locking screws. The fracture must be reduced prior to applying locked screws.
A small fragment posterior to the distal fibula may represent an avulsion of the superficial peroneal retinaculum. If not addressed, this injury may lead to peroneal tendon subluxation.
Technique of Fibular Nailing
Video 35.1 Fibular Fixation with an Intramedullary Nail
Used as a stand-alone implant, fibular nailing works best for transverse or short oblique fractures in which the intramedullary device maintains the reduction and keep the fibula out to length. Intramedullary nails have been fashioned from Steinmann pins, ball-tipped guidewires, long 3.5-mm cortical screws (found in most pelvic sets), or dedicated locked fibular nails. The “nail” is inserted percutaneously in a retrograde manner through a small incision distal to the tip of the fibula. Once the fibula reduction is obtained (usually open), a 3.5-mm or other oscillating drill gains access to the intramedullary canal of the fibula. Next the selected nail implant is inserted across the fracture in line with the intramedullary canal in both AP and lateral views on image intensification. For a “do-it-yourself” nail, it is bent distally and cut short. The potential advantages of a nailing technique include minimal wound complications, reduced blood loss, and fewer implant-related symptoms than a lateral plate. The disadvantages include a lack of rotational control in all fractures and the inability to maintain length in comminuted fractures. The effectiveness of this type of fixation has been shown in a few small studies.37 Specialty devices have been developed to enable a fibular nail to be inserted and locked proximally and distally to counteract these shortcomings (Fig. 35.9). A study looking at the use of these locking fibular nails in fragility fractures showed this device to be a viable treatment option, though there was no comparison group.38

Medial Malleolus Fractures
Medial malleolus fractures usually occur in conjunction with lateral malleolus fractures, but occasionally occur as an isolated injury in P-ER or P-AB injuries (Fig. 35.4). It is important to obtain radiographs of the entire tibia and fibula, as an isolated medial malleolus may be part of a more complex Maisonneuve fracture with a proximal fibula fracture and injury to the syndesmosis (Fig. 35.10). Medial malleolar fractures may be transverse, oblique, or nearly vertical in orientation. Transverse or oblique fractures represent avulsion injuries and may involve the entire medial malleolus or just the anterior colliculus. This distinction is made by careful review of the lateral radiograph. Because the deep deltoid ligament attaches to the posterior colliculus, injury to the deep deltoid ligament can coexist with an anterior collicular fracture. In this case, repair of the anterior malleolar fragment will not restore competence of the medial ligament and the ankle may remain potentially unstable. In contrast, transverse fractures of the entire malleolus are not associated with ligament injury, and fixation of complete malleolar fractures restores stability.30

Currently, there are no long-term studies on outcomes of isolated medial malleolus fractures. We recommend that nondisplaced or very minimally displaced fractures be treated with immobilization, but fractures displaced more than 2 mm should be treated with ORIF.1 Plain radiographs provide limited accuracy for imaging the medial malleolus, and even small amounts of residual radiographic displacement of medial malleolus fractures may in reality correlate with much larger amounts of true malreduction. One should carefully scrutinize all three radiographic views of the ankle in assessing these injuries, and even then they may be better visualized with a CT scan. It has been noted that a sizable malreduced fracture may behave like a deltoid ligament injury and lead to dynamic ankle instability,21 and painful nonunions of displaced medial malleolus fractures are not uncommon after closed treatment.39 Strong consideration should also be given to open reduction for fractures where small osseous or osteochondral fragments are in the joint, as these can lead to mechanical wear or impingement.40 When the fractured medial malleolus is exposed, the joint should be carefully inspected for free fragments and chondral injuries, which may indicate a more guarded prognosis for the ankle.
Technique of Medial Malleolar Fixation
We use a curvilinear incision extending from above the anteromedial aspect of the ankle joint superiorly and curving distally around the tip of the medial malleolus (Fig. 35.11). The advantage of this approach is the excellent visualization of the medial ankle joint and fracture reduction proximally. Partially threaded lag screws are then typically placed through the incision more distally. The disadvantage of this approach is that the surgeon necessarily encounters the saphenous vein and nerve, which must be carefully preserved. Some surgeons prefer a straight longitudinal medial incision extending over the fracture and the tip of the medial malleolus or a curved incision that extends around the posterior aspect of the medial malleolus.41 The major limitation of these approaches is impaired visualization of the articular reduction and any articular injury. Furthermore, making an incision of the skin directly over the fracture could lead to potentially catastrophic wound problems.

Most medial malleolus fractures are well fixed with two partially threaded cancellous lag screws (Fig. 35.12), either cannulated (3.5–4.5 mm) or noncannulated (4.0 mm). Depending on the fracture configuration, smaller fragments may be fixed with a screw and a K-wire (cut short and bent) placed for rotational stability. Comminuted fractures may require a tension band construct or even supplemental fixation with mini-fragment screws. Type S-AD fractures (Fig. 35.4) or other more vertically oriented fractures that extend further into the tibia should be fixed with an antiglide plate (with or without lag screws) to prevent vertical migration (Fig. 35.13). A third tubular plate from the small fragment set, or even a 2.7- or 2.4-mm mini-fragment plate, is effective as long as the screws are placed in the appropriate order and the purchase is acceptable.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree