Chapter 9 Aorta
Aortic atherosclerosis
Aortic atherosclerosis is nearly universal by midlife. Its severity is governed by factors including diabetes, hypercholesterolaemia, hypertension, and smoking. It can be clinically manifested as aneurysms, embolization from atheromatous plaques, obstruction (commonly the infrarenal aorta), and penetration of plaque into the media that can initiate dissection.
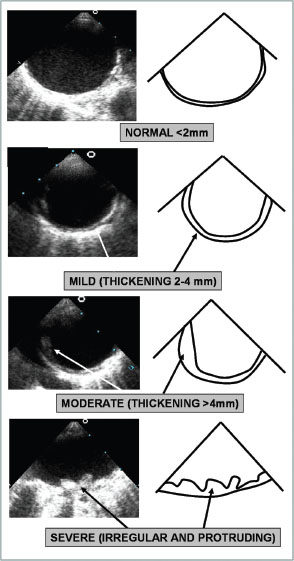
Aortic atherosclerosis is a sign of increased cardiovascular risk from coronary artery, cerebrovascular and renovascular disease. Plaques can be identified on transoesophageal echocardiography (TOE) see Fig. 9.1. Calcific plaques are readily visualized on computed tomography and rarely on plane films.
Penetrating atherosclerotic ulcer
 Ulceration of an atherosclerotic lesion of the aorta that penetrates the elastic lamina of the aorta allowing haematoma formation within the media.
Ulceration of an atherosclerotic lesion of the aorta that penetrates the elastic lamina of the aorta allowing haematoma formation within the media.
 Usually occurs in the descending aorta in elderly smokers.
Usually occurs in the descending aorta in elderly smokers.
 Clinical presentation is similar to aortic dissection with chest or back pain.
Clinical presentation is similar to aortic dissection with chest or back pain.
 In up to 25% of cases, penetration through to the adventitia results in formation of a false aneurysm, and transmural aortic rupture occurs in up to 10% of cases.
In up to 25% of cases, penetration through to the adventitia results in formation of a false aneurysm, and transmural aortic rupture occurs in up to 10% of cases.
 Aortography is the diagnostic standard.
Aortography is the diagnostic standard.
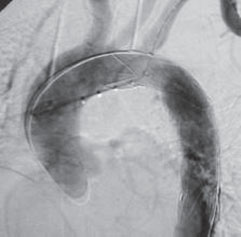
 Standard treatment is high-risk surgery, but there has been increasing success with the use of endovascular stents (Fig. 9.2).
Standard treatment is high-risk surgery, but there has been increasing success with the use of endovascular stents (Fig. 9.2).
Athero-embolism
 Embolization of plaque material from the luminal surface of a severely diseased aortic segment to cerebral, coronary, visceral, and renal circulations and extremeties is a common cause of mortality and morbidity.
Embolization of plaque material from the luminal surface of a severely diseased aortic segment to cerebral, coronary, visceral, and renal circulations and extremeties is a common cause of mortality and morbidity.
 TOE can identify such material as well as spontaneous contrast.
TOE can identify such material as well as spontaneous contrast.
 Anticoagulation can reduce the risk of future events, as can statin and antiplatelet use.
Anticoagulation can reduce the risk of future events, as can statin and antiplatelet use.
Fig. 9.1 Transoesophageal echocardiography images of atherosclerosis in the descending aorta. The images demonstrate the grades of severity from normal to severe.
Aortic aneurysm
 Commonly seen in the abdominal aorta.
Commonly seen in the abdominal aorta.
 Degeneration of the media results in widening of the lumen and loss of structural integrity.
Degeneration of the media results in widening of the lumen and loss of structural integrity.
 Elastic recoil is lost and ischaemic changes can be precipitated through obstruction of the vasa vasorum.
Elastic recoil is lost and ischaemic changes can be precipitated through obstruction of the vasa vasorum.
 Multiple factors, such as genetic defects in collagen, collagenase, and elastase, are believed to be involved in the mechanism resulting in vessel wall injury. Atherosclerosis is thought to contribute to the pathogenesis as a secondary response to vessel wall injury.
Multiple factors, such as genetic defects in collagen, collagenase, and elastase, are believed to be involved in the mechanism resulting in vessel wall injury. Atherosclerosis is thought to contribute to the pathogenesis as a secondary response to vessel wall injury.
Chest X-ray
On plain X-ray aortic wall calcification is seen in less than half of aortic aneurysms, leading to a high false-negative rate. Therefore plain X-ray is not routinely recommended in suspected cases.
Ultrasound (Fig. 9.2)
This is a sensitive test for screening patients at risk of abdominal aortic aneurysms or to monitor size over time. It is of limited value for detecting leakage, rupture, or branch artery involvement
CT
CT is highly sensitive for detecting abdominal aortic aneurysms. It can also detect leakage or rupture and accurately define size and shape, involvement of branch arteries, and adjacent organ involvement. 3D series are used to plan endovascular procedures.
Cardiac magnetic resonance
Imaging of the aorta is equivalent to CT. Advantages are avoidance of dye and superior imaging of branch vessels compared with CT or ultrasound.
Fig. 9.2 Aortography during implantation of a covered stent in a patient with limited rupture of the descending aorta. The stent is carefully positioned just distal to the left subclavian artery. Reproduced with permission from Myerson SG, Choudhury RP, and Mitchell ARJ (2010) Emergencies in Cardiology 2e, Oxford University Press.
Aortic dissection
An aortic dissection is a tear in the aortic intima through which blood enters the aortic wall and strips the media from the adventitia (Fig. 9.3).
 The dissection may result in fatal aortic rupture or propagate distally generating a blood-filled space between the dissected layers.
The dissection may result in fatal aortic rupture or propagate distally generating a blood-filled space between the dissected layers.
 The blood supply to major branches (including the coronary arteries) may be compromised.
The blood supply to major branches (including the coronary arteries) may be compromised.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree