Fig. 1
Schematic view of the sigmoid colon with several epiploic appendages
Normal appendages can be seen on sonography or CT only if surrounded by free intraperitoneal fluid (Fig. 2). Most of them are 2–5 cm in length and 1–2 cm thick, with vessels passing through their narrow pedicle. The pedunculated nature and the great mobility of the appendages are factors that increase the possibility of torsion and infarction.
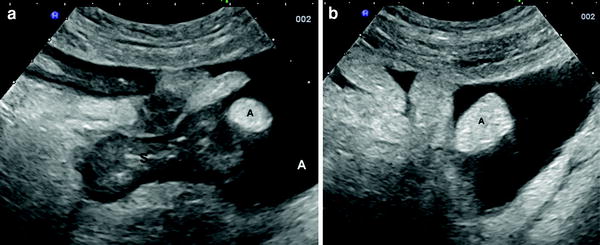
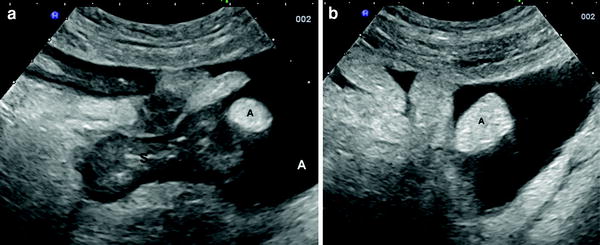
Fig. 2
a, b Ultrasonographic aspect of normal appendages (arrows) observed in patients with ulcerative colitis and ascites (A). S sigmoid colon
The nature of epiploic appendagitis may be primary or secondary. Primary epiploic appendagitis is attributed to either torsion or spontaneous venous thrombosis with subsequent ischemic or haemorrhagic infarction and inflammation of the epiploic appendages (Rao et al. 1997; Rioux and Langis 1994). Secondary epiploic appendagitis is caused by adjacent inflammatory processes such as diverticulitis, appendicitis or cholecystitis (Molla et al. 1998).
Epiploic appendagitis is primarily an adult disease. Epiploic appendages are rudimentary in children, reach an appreciable size in adulthood and are largest in obese patients. Obesity is a possible predisposing factor for epiploic appendagitis, and heavy exercise and excessive stretching have been reported to precede the onset of clinical symptoms (Hollerweger et al. 2002).
3 Clinical Manifestations
Epipolic appendagitis is characterised by acute or subacute abdominal pain, mostly at the left lower quadrant, suggestive of acute diverticulitis. Pain could be localised or show signs of peritonitis. Epiploic appendagitis of the caecum or ascending colon usually presents with right lower or right upper quadrant pain that mimics appendicitis or cholecystitis (Van breda vriesman et al. 1999).
Most patients report an acute onset of abdominal pain and well-localised tenderness. Pain may intensify on coughing, deep breathing or stretching or when a skin fold is pulled upward; this is due to the adherence of the inflamed appendages to the parietal peritoneum. A few patients may experience initially mild symptoms that increase during the first days. Symptoms improve gradually within 5–7 days after their onset, but, in some cases, they may last up to 2–3 weeks.
Other notable complaints or clinical findings, such as fever >38 °C, nausea, vomiting or diarrhoea are usually absent.
Although epiploic appendagitis has some specific clinical features, this is often misdiagnosed and it is rarely considered in the differential diagnosis with other acute conditions. In this regard, the degree of inflammatory response may help in the differential diagnosis because epiploic appendagitis is associated with no or only mild systemic inflammation (Legome et al. 2002). The leukocytes count is normal or slightly superior to normal values; erythrocyte sedimentation rate and C reactive protein are usually normal or slightly elevated (Table 1).
Table 1
Main biochemical features of patients with epiploic appendagitis reported by the largest series of patients published in the literature
Author, year | No. of pts | C reactive protein | White blood cells | ||
|---|---|---|---|---|---|
Increased values n, (%) | Median (range) of increased values | Increased values n, (%) | Median (range) of increased values | ||
Sand et al. (2007) | 10 | 5 (50) | 9 (5–15) | 1 (10) | 11,400 |
Görg et al. (2009) | 20 | 6 (30) | 14 (7–23) | n.a. | n.a. |
Ozdemir et al. (2010) | 12 | n.a. | n.a. | 4 (33.3) | 14,600 (12,800–20,500) |
Chen et al. (2011) | 21 | n.a. | n.a. | 6 (28.6) | 11,450 (10,500–11,800) |
Choi et al. (2011) | 27 | n.a. | n.a. | 4 (12.9) | n.a. |
Epiploic appendagitis is generally a self-limiting disease and conservative treatment is recommended unless imaging methods indicate a complicated disease. When patients are treated with mild analgesics, symptoms mostly resolve over the course of 1 week. Laparoscopic resection may be useful in selected cases, especially when abdominal pain persists (Schnedl et al. 2011).
4 Ultrasound
The first ultrasonographic description of epiploic appendagitis was reported in 1987 (Jennings and Collins 1987).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree