Approach to the Lateral Neck Radiograph
The lateral neck radiograph is a relatively inexpensive, readily available, and easy-to-perform examination that is very useful for the evaluation of suspected abnormalities in the upper aerodigestive tract. In the emergency setting the lateral neck radiograph is commonly obtained to evaluate for abnormalities causing acute respiratory distress or dysphagia. The examination also can be useful in the workup of chronic obstruction of the airway. The first portion of this chapter will outline the appropriate technique for acquiring the optimal lateral neck radiograph image and review pertinent anatomy. The common indications for obtaining the lateral neck radiograph will then be addressed, as well as the findings seen in some of the most common and most critical diagnoses encountered when this examination is ordered.
Technique
Before imaging the child, it is prudent for the radiologist to gather clinical data regarding the patient, if possible. This will facilitate the appropriate approach to imaging the patient in the safest manner, as well as help guide diagnosis. Important considerations include the onset and duration of symptoms, associated symptoms (e.g., fever, toxic appearance, or drooling), physical examination findings (e.g., stridor, barky cough, rales, rhonchi), and the known or suspected ingestion of a foreign body or caustic agent. For a patient in respiratory failure or impending respiratory failure, imaging should be deferred until an adequate airway is established.
When a child presents in acute respiratory distress, it is important to consider how positioning of the child can affect breathing, because maintaining the airway is of paramount concern. Given that the child’s airway is incompletely developed and flexible compared with the adult, supine imaging can acutely worsen respiratory distress and result in complete respiratory obstruction. Thus the lateral radiograph is ideally obtained in an upright position.
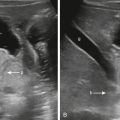
To obtain maximal distention of the airway, the child is typically imaged with the neck extended and breath held in inspiration. Together, these techniques minimize prevertebral soft tissue redundancy and maximally distend the airway to better evaluate the anatomy ( Fig. 26.1 ). When taking a breath in, the musculature of the upper airway contracts, which allows for increased air flow while maintaining or dilating the nasal, pharyngeal, and laryngeal airways. In the older child a command to take a deep breath is usually adequate. In the young child, timing the radiograph can be more difficult, often requiring more than one attempt. In addition, the prevertebral soft tissues in neonates, infants, and toddlers can be particularly difficult to efface even with optimal technique. If all else fails, airway fluoroscopy could be performed for real-time evaluation of the soft tissues of the neck.

How to Read the Lateral View
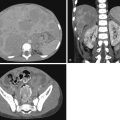
Evaluation of the lateral neck radiograph requires a good understanding of the relevant anatomy of the neck, and it is important for the radiologist to be familiar with the normal and abnormal appearance of the anatomical structures ( Fig. 26.2 ). One approach is to evaluate the anatomy from the point of entrance of inspired air in the nasopharynx through the lower cervical trachea as it approaches the chest.

Tonsils and Adenoids
The adenoids, also known as the nasopharyngeal tonsils, are located superior to the palatine tonsils along the roof of the nasopharyngeal airway. As with other tonsillar tissues, the adenoids play a protective role against infectious disease in the upper airway. Adenoidal pathology predominantly relates to abnormally enlarged size, which can impinge on the nasopharyngeal airway and contribute to significant acute or chronic upper respiratory obstruction. Various methods for the radiographic evaluation of adenoidal enlargement have been proposed in the literature. An easy and effective approach is to give a subjective assessment on the level of impingement on the nasopharyngeal airway (mild, moderate, or severe narrowing versus complete obstruction). One can also calculate the adenoidal/nasopharyngeal ratio, which provides a more objective description of nasopharyngeal impingement by way of measuring the adenoidal size (A) relative to the diameter of the nasopharynx (N) and reporting the A/N ratio. Distance “A” is measured from the margin of the basiocciput to the maximal convexity of the adenoid, while distance “N” represents the distance between the posterior superior margin of the hard palate and the anterior edge of the sphenobasioccipital synchondrosis. An A/N ratio greater than 0.8 indicates enlarged adenoids. Finally, a direct measurement of the diameter of the adenoids can also be reported. This is more difficult to interpret and generalize to all children, however, because the acquired measurement could have different implications based on the child’s age and size.
Epiglottis
The epiglottis is a small, fibrocartilaginous flap of tissue that protects the airway from aspiration during swallowing by covering the trachea and facilitating the propulsion of an ingested bolus into the esophagus. It is located at the level of C3 and the hyoid bone. When normal in size, the epiglottis is a thin structure. An abnormally enlarged epiglottis has a thickened appearance and has been described as similar to the size and shape of a child’s thumb. The aryepiglottic folds are the normally thin and delicate slips of tissue extending obliquely from the free edge of the epiglottis to the arytenoid cartilages. The laryngeal vestibule, or inlet of the larynx, is formed anteriorly by the epiglottis and posteriorly and laterally by the aryepiglottic folds and arytenoid cartilages. An infectious or inflammatory abnormality of the epiglottis causes airway obstruction not typically because of the enlargement of the epiglottis by itself, but because of the swelling of the surrounding soft tissues and obstruction of the laryngeal inlet.
Subglottic Airway
The subglottic airway extends from the true vocal cords to the lower margin of the cricoid cartilage. This region is vulnerable to significant pathological obstruction due to its small size and the relatively inflexible surrounding cricoid. Narrowing of the subglottic airway is an important indicator of even mild edema and inflammation associated with an acute infectious process. Although mild subglottic narrowing can sometimes be visualized on the lateral radiograph, findings are usually much more evident on the frontal view. Therefore in children who present with stridor or a barky cough, it is prudent to obtain a frontal view for optimal evaluation. In the normal anteroposterior appearance of the subglottic airway, there is shouldering of the subglottic trachea, with a nearly horizontal superior margin of the tracheal column ( Fig. 26.3 ). Symmetrical or asymmetrical narrowing, compression, or deviation of the tracheal column on the frontal view indicate significant pathology.

Prevertebral Soft Tissues
Evaluation of the prevertebral soft tissues can be one of the most important yet most frustrating components of interpretation of the lateral neck radiograph. This is particularly true in very young patients who have short necks, redundant soft tissues, and are unable to cooperate with instructions for respiration and positioning. Occasionally the presence of prevertebral soft tissue thickening remains unclear despite two or three attempts to acquire an adequate image. If the radiologist is not satisfied with the quality of examination achieved with static radiograph technique, further evaluation with dynamic fluoroscopic observation could quickly elucidate the upper airway anatomy and resolve any questions from the radiographic examination.
Determining the presence of prevertebral soft tissue thickening is critical in evaluation of potential retropharyngeal infection, trauma, or mass. Normal measurements of the prevertebral soft tissues vary considerably according to the cervical level and age of the patient. One simple technique is to compare the prevertebral soft tissue thickness with the anteroposterior dimension of the adjacent vertebral body, which adjusts for patient age and growth. The prevertebral soft tissues from C1 to C4 usually measure less than half the anteroposterior dimension of the adjacent vertebral body. In older children, because of increasing ossification of the adjacent vertebral bodies, the prevertebral soft tissues decrease in relative thickness from C1 to C4. Below C4, up to one vertebral body width is considered normal, because of the esophageal soft tissues. These are general rules for a technically adequate radiograph. Close attention to imaging technique is important because lateral radiographs obtained in expiration and flexion can exaggerate prevertebral thickness. Repeat radiographs may be necessary. If there is persistent prominence of the soft tissues, retropharyngeal edema or abscess may be present, and computed tomography (CT) of the neck may be indicated (guided by history and level of clinical concern).
Secondary signs of infection or trauma are as important as, if not more important than, soft tissue swelling if present. Foci of gas (outside the esophagus) could indicate infection with gas-forming infectious agents or tracheal or esophageal perforation as a result of foreign body or trauma. Abnormal radiodensity may indicate ingested foreign body or calcification within a mass.
In general, paired calcified structures projecting in the soft tissues are likely normal. The hyoid bone ossifies progressively after birth at the level of C3. There may also be styloid processes extending caudally from the inferior surface of the temporal bones toward the hyoid and variable calcification of the stylohyoid ligaments. Although normal calcification of the thyroid, cricoid, and arytenoid cartilages occurs with age, these structures are generally noncalcified in childhood, with the exception of those seen in teens.
“Edge of Film” Findings
Although the majority of pathology in the neck will cause an alteration in the normal anatomy described earlier, one must scrutinize all structures included in the field of view. Occasionally, significant findings can be detected within the bones, sinuses, nasal cavity, or upper chest. Foreign bodies can be located anywhere along the aerodigestive tract, including the nasal cavity and thoracic inlet. Careful review of the osseous structures may reveal fracture, malalignment, or focal lesion that could point to trauma or neoplasm. Paranasal sinus opacification may indicate sinusitis or mass lesion.
Case Examples
Adenoid and Tonsillar Enlargement
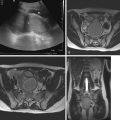
Adenotonsillar hypertrophy results from growth of lymphoid tissue in Waldeyer ring in the nasopharyngeal region as a result of frequent infection and obstructive causes. The enlarged tonsillar tissue may cause respiratory compromise in the acute phase of infection, or on a chronic basis in the setting of obstructive sleep apnea. Other factors may also contribute to nasopharyngeal obstruction, such as craniofacial dysplasia, neuromuscular disorders, and palatal surgeries, so it is preferred to describe adenoidal size with respect to relative amount of impingement on the nasopharyngeal airway rather than a single measurement. As previously described, an A/N ratio greater than 0.8 indicates adenoidal enlargement with significant nasopharyngeal obstruction likely ( Fig. 26.4 ).

Acute tonsillitis is accompanied by the clinical signs of fever, dysphagia, and odynophagia. Lymphadenopathy is often present, and occasionally the patient exhibits excessive drooling and altered voice quality. Airway compromise can result from enlargement of the tonsils themselves or from the formation of tonsillar or peritonsillar abscess or edema, which results in prevertebral soft tissue thickening. Retropharyngeal abscess is an important complication of tonsillitis and pharyngitis with potentially severe clinical implications, which will be discussed separately.
Obstructive sleep apnea consists of recurrent events of partial or complete airway obstruction during sleep, resulting in disrupted ventilation and sleep patterns. The point of obstruction is often in the nasopharynx or oropharynx, which again could be caused by adenotonsillar hypertrophy or other anatomical or neuromuscular abnormalities. Imaging plays an important role in determining the cause of obstruction, and early intervention is critical, because chronic obstructive sleep apnea has been linked to daytime hypersomnolence, behavior disorders, secondary enuresis, and failure to thrive. Delayed diagnosis can lead to more severe complications, such as cor pulmonale or neurological damage.
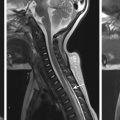
Retropharyngeal Abscess
Retropharyngeal abscess is most commonly diagnosed before 6 years of age, usually in association with upper respiratory tract infections and tonsillitis. Additional causative factors include injury from foreign body ingestion or iatrogenic injury (e.g., after traumatic intubation). Clinical symptoms include odynophagia, dysphagia, trismus, fever, drooling, and muffled voice. Torticollis and displacement of the uvula may be present on physical examination. By radiography, prevertebral soft tissue swelling, loss of the cervical lordosis, and abnormal soft tissue gas are all indicators of retropharyngeal abscess. CT or MRI is necessary to confirm diagnosis and is helpful in identifying drainable fluid collections, providing more precise anatomical delineation and extent of infection, and evaluating for complications, such as vascular thrombosis (typically internal jugular thrombosis) or pseudoaneurysm ( Fig. 26.5 ). The radiologist should also be aware of Grisel syndrome, a rare but severe complication of cervical infection where inflammation leads to cervical ligamentous laxity and atlantoaxial subluxation, with potential for development of permanent neurological sequelae.