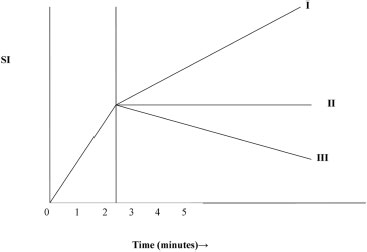
3 Approach to Magnetic Resonance Imaging Similar to mammography, effective evaluation of breast magnetic resonance imaging (MRI) requires an organized approach. The first step involves identifying all possible suspicious lesions. Because suspicious lesions exhibit contrast enhancement, you should review MRI sequences that are produced after contrast injection. Depending on the MRI protocol, these sequences may be T1 fat-suppressed images, maximum intensity projection (MIP) images, or T1 subtracted images in which the image results from subtracting the precontrast image from the postcontrast image. Various MRI computer-aided detection (CAD) systems may also aid in quickly demonstrating potentially suspicious enhancing lesions. Upon identifying suspicious enhancement, you face the first diagnostic decision: does the lesion represent a mass, non-mass enhancement, or a focus? Whereas a mass is a space-occupying lesion, non-mass enhancement represents a pattern of enhancement that does not have a defined three-dimensional shape. In contrast to the mass, the focus represents punctuate enhancement that is too small to be characterized. If the lesion is a mass, then the next step is to assess if it is benign (American College of Radiology [ACR] Breast Imaging Reporting and Data System [BI-RADS] category 2). The easiest lesions to characterize as benign are masses such as lymph nodes and cysts. If these masses are suspected, review T2 images without fat suppression to search for the fatty hilum of the lymph node and the fluid composition of the cyst. If the mass is not clearly benign, analyze the shape and margin of the mass, preferably on high-resolution images that are produced soon after contrast injection. These characteristics are best identified when the mass reaches maximal enhancement; as the enhancement fades, the margins of the mass may be distorted or indistinct. Masses with irregular shape or irregular or spiculated margins are either suspicious or highly suspicious (ACR BIRADS category 4 or 5). Enhancement patterns that increase the suspicious nature of the mass include enhancing septations and central enhancement. Rim enhancement is also a suspicious finding. The most common benign entities that may exhibit rim enhancement are an inflamed cyst and fat necrosis. These abnormalities may be differentiated from malignancy by the appearance of cyst fluid or fat on the T2 non–fat-suppressed image. Masses that exhibit suspicious or highly suspicious morphology should be biopsied no matter what type of kinetic curve the mass exhibits (Table 3.1). For those masses that are not clearly suspicious, kinetic curve analysis is important in determining the final assessment of the mass. Masses that require kinetic curve analysis include those that have round, oval, or lobulated shapes as well as smooth contours. There are three main types of kinetic curves: type I, persistent; type II, plateau; and type III, washout. Type I curves show enhancement that increases throughout the entire observed time course. Type II curves exhibit an early rise in enhancement, then reach a steady state. Type III curves initially demonstrate a rapid increase, reach a peak, then decrease in enhancement (Fig. 3.1). Benign lesions tend to exhibit type I curves, and malignant entities commonly demonstrate type II (30%) or III (60%) curves. If the round, oval, lobulated mass with smooth contours exhibits a type I curve, then the mass is assessed as probably benign, and short interval follow-up MRI is recommended (ACR category 3). However, if the mass has a type II or III curve, then the mass is suspicious, and biopsy is recommended (ACR category 4). If the lesion is not a mass, then the lesion is either a focus or exhibits non-mass enhancement. A focus is generally ≤ 5 mm in size. When there are multiple foci, the pattern of the foci is important. Multiple diffusely scattered, bilateral foci are generally benign. This pattern is most commonly due to fibrocystic changes but is sometimes related to hormonal effects. If foci are distributed in a linear or segmental pattern, the foci may be due to ductal carcinoma in situ. Furthermore, if the multiple foci are close to a dominant malignancy, then these foci are likely to be satellite malignancies. Single foci are more worrisome than multiple foci. Although these foci are most likely benign (< 3% in one series), if they exhibit a suspicious kinetic curve, they should be biopsied. The differential diagnosis of foci include hormonal enhancement (either physiologic or due to exogenous hormone replacement), fibrocystic change, fibroadenoma, papilloma, radial scar, atypical ductal hyperplasia, lobular carcinoma in situ, ductal carcinoma in situ, and invasive lobular or ductal carcinoma. Of the non–mass-enhancing descriptions, the most suspicious are ductal and clumped enhancement. Ductal enhancement is linear enhancement that is oriented toward the nipple and conforms to a duct. Clumped enhancement in a focal location looks like a bunch of grapes or, when linear, looks like a string of pearls. When clumped enhancement involves larger areas of the breast, this enhancement pattern looks like cobblestones.
 Analyzing the Breast Magnetic Resonance Imaging Scan
Analyzing the Breast Magnetic Resonance Imaging Scan
Identifying Suspicious Lesions
BI-RADS Assessment | Definition | Examples MRI Findings |
Category 2 | Benign finding | 1. Cyst 2. Fat necrosis 3. Lymph node 4. Mass: oval, round, lobulated shape, and smooth margin with dark septation (fibroadenoma) |
Category 3 | Probably benign finding; initial short-term interval follow-up suggested | Mass: oval, round, or lobulated shape and smooth margins and homogeneous enhancement and benign kinetic curve (e.g., persistent time course) |
Category 4 | Suspicious abnormality; biopsy should be considered | 1. Mass: oval, round, or lobulated shape and smooth margins and homogeneous enhancement and suspicious kinetic curve (e.g., plateau or washout time course) 2. Mass: irregular shape, irregular margin, persistent kinetic curves 3. Non-mass: segmental enhancement with clumped or ductal enhancement and either persistent or plateau kinetic curves |
Category 5 | Highly suspicious for malignancy | 1. Mass: irregular shape, spiculated margin, and any kinetic curve 2. Mass: irregular shape, irregular margin, and any of the following enhancement patterns: rim (first, rule out fat necrosis and inflammatory cyst), enhancing septations, or central enhancement 3. Mass: irregular shape, irregular margin with rapid enhancement and washout 4. Non-mass: segmental with clumped or ductal internal enhancement with rapid enhancement and washout |
Fig. 3.1 Schematic diagram of contrast enhancement kinetic curves. The diagram illustrates the three types of kinetic curves exhibited by breast masses. Type I is the persistent curve that exhibits increasing enhancement. Type II is the plateau curve that initially increases and then reaches a stable level. Type III is the washout curve that initially increases, reaches a peak level between 2 and 3 minutes, then decreases. Type I curves tend to characterize benign lesions. Malignant masses most commonly produce type II and III curves. SI, signal intensity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree