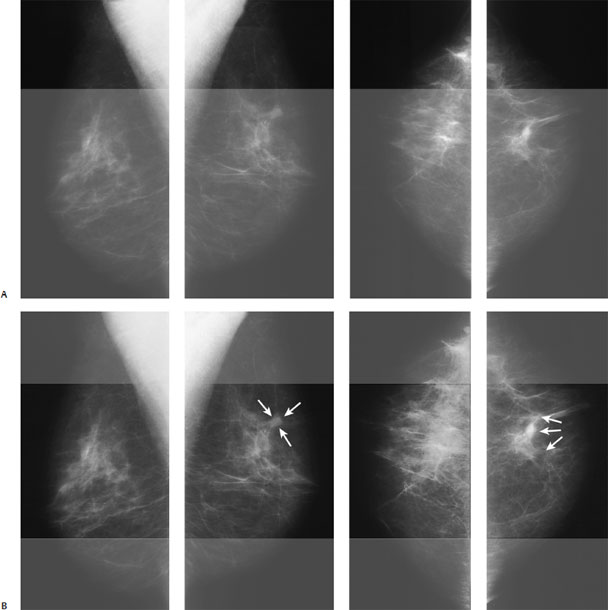
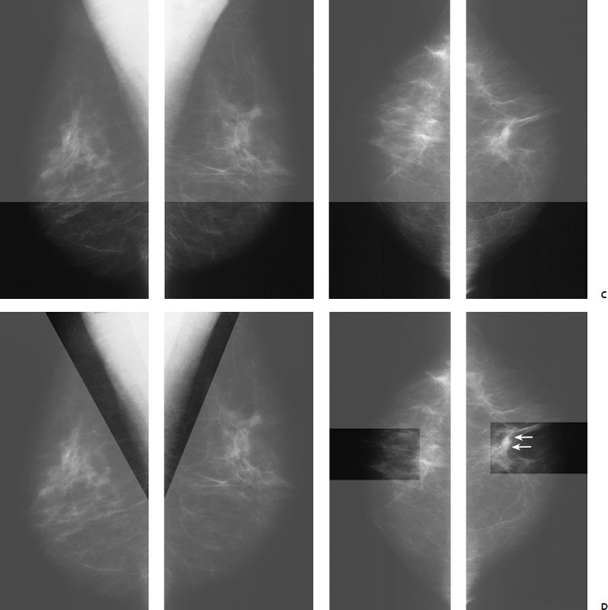
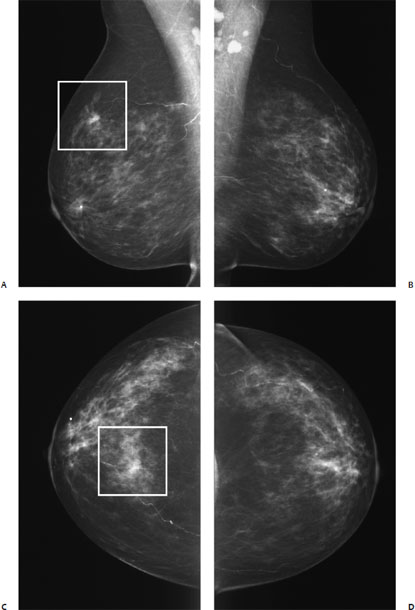
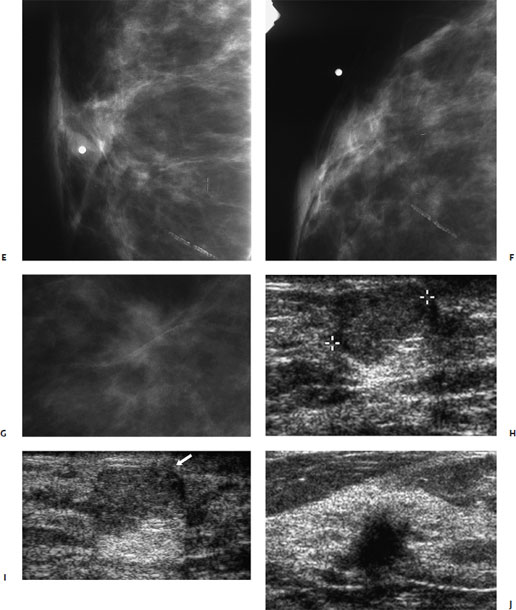
1 Approach to Mammographic Analysis There are three factors that lead to identifying mammo-graphic abnormalities: production of high-quality images, perception of a lesion, and characterization of the finding. A team of professionals is needed to produce high-quality mammograms. The radiologist and the technologist should constantly be evaluating images for film contrast, exposure parameters, patient position, and image processing. Furthermore, a radiation physicist should work with the technologist to monitor equipment performance. Perception of mammographic abnormality is the first step in identifying a breast malignancy. Perception is aided by a systematic review of the mammographic examination. Consistent systematic review of the mammogram is critical in avoiding perceptual errors. Tabar and Dean’s Teaching Atlas of Mammography 1 has an excellent explanation of a horizontal and vertical masking technique that facilitates identification of abnormal mammographic asymmetries. Masking entails physically covering portions of the film so that only small corresponding regions of the two breasts are visible. In a busy practice or with digital mammography this technique is not practical, but one can develop the ability to visually mask by focusing on a small area of the breast and comparing it with the equivalent area on the contralateral side. My personal method involves this latter technique. I visually mask all breast views horizontally and then perform a second focused review of the axilla and the subareolar regions (Fig. 1.1). During the review of the mammographic examination, one may identify asymmetries or calcifications. The breast imager should classify the asymmetry as a density or architectural distortion. The densities should be further analyzed and subdivided into either masses or asymmetric densities. Using the following methods, the breast imager then analyzes the lesion and assigns an assessment category according to the American College of Radiology (ACR) Breast Imaging Reporting and Data System (BI-RADS). These assessment categories are as follows: • Category 0: Need additional imaging evaluation. This evaluation may include additional mammographic views (e.g., spot compression) or other imaging modalities (e.g., ultrasound). • Category 1: Negative. The breasts are normal. • Category 2: Benign finding. The mammogram is normal, but there is a finding that the interpreter wishes to describe. • Category 3: Probably benign finding. Short-interval follow-up suggested. The finding has a high probability of being benign and is not expected to change in appearance. In this book, I generally assume that the patient will be reimaged approximately 6 months after this assessment is made. • Category 4: Suspicious abnormality. Biopsy should be considered. The radiologist has enough concern about the lesion that biopsy is being recommended. • Category 5: Highly suggestive of malignancy. Appropriate action should be taken. After finding an asymmetry, the breast imager should classify the finding into one of four patterns: mass, focal asymmetry, calcifications, and architectural distortion. If a density is identified, then the radiologist should first clarify if the density is a mass or a focal asymmetry. A mass is a density that has a consistent shape when imaged at different angles and with different patient positions. If the imager concludes that the lesion is a mass, then he or she should determine whether the shape of the mass is circumscribed or irregular. Circumscribed masses are round, oval, or lobulated (see Chapters 5 and 6). Circumscribed masses are commonly benign. Only 1.4% of well-defined circumscribed masses are malignant. As there are many benign lesions in this category, diagnostic evaluation should be directed toward excluding many of these benign lesions from being biopsied. The first step is to analyze the density of the mass. If the mass has a density equal to or greater than the parenchyma, then further examination is necessary. The next step is to examine the margins of the mass. If the margins are sharp or obscured by the surrounding parenchyma, then the mass should be examined sonographically. If the mass clearly has ill-defined or spiculated borders, then biopsy is indicated (category 4 or 5). This biopsy may be performed sonographically, as almost all of these lesions are sonographically visible, particularly if they are larger than 4 to 5 mm. As noted earlier, circumscribed mammographic masses that have well-defined or obscured margins should be examined sonographically. Of these masses, sonographically identified cysts are obviously benign (category 2). If the mass is well defined and uniformly hyperechoic to fat, it is probably benign (category 3). The mass is also probably benign (category 3) if it has all of the following characteristics: (1) shape: round, oval, or one or two lobulations; (2) margin: well defined with a hyperechoic thin capsule; (3) echogenicity: uniformly hypoechoic. Fig. 1.1 (A,B) Systematic method to review mammograms. Horizontal examination: initially, you should focus on a small region in the superior section of the right film and then compare it with the comparable left side. You should then proceed inferiorly in the mammogram and continue the process. In this case, there is trabecular thickening and architectural distortion at the 12 o’clock position of the left breast (arrows). This lesion is an infiltrating ductal carcinoma. Systematic method to review mammograms. After the horizontal examination, (C) you should study the axillary and subareolar regions of each breast, (D) and compare each area with the contralateral side. The axillary region is important because the upper outer quadrant contains the highest percentage of breast cancers. Extra attention to the subareolar region is worthwhile, as this area exhibits a complex architecture consisting of numerous ductal lines. Subareolar architectural distortion is commonly difficult to identify. In this case, the malignancy produces left subareolar architectural distortion (arrows). If the margin is extremely well defined but does not have a hyperechoic capsule, I also assess it as probably benign (category 3). To characterize whether a margin is well defined, you must have high-quality, high-resolution, and high-frequency (≥ 10 MHz) equipment. Furthermore, the entire margin must be well defined and clearly visible (Fig.1.2). Finally, there should not be any other associated abnormality such as sonographic architectural distortion. In this situation, I am also assuming that I have seen the patient only once, and there is no evidence of growth. If the lesion has been identified on earlier imaging exams and has grown in size, then I will recommend biopsy (category 4). Fig. 1.2 Two breast cancers. (A) Right mediolateral oblique (MLO) digital mammogram. (B) Left MLO digital mammogram. (C) Right craniocaudal (CC) digital mammogram. (D) Left CC digital mammogram. There is a palpable right breast mass that is labeled with a radiopaque dot at the 3 o’clock position near the nipple. Independent of this palpable lump, there is an irregular mammographic mass (square). Two breast cancers. (E) Right MLO spot magnification mammogram of palpable lump. (F) Right CC spot magnification mammogram of mammographic mass. (H) Right antiradial breast sonogram of palpable lump. (I) Right antiradial breast sonogram of palpable lump. (J) Right antiradial breast sonogram of mammographic mass. (E,F) Although the palpable lump does not correspond to a mammographic mass, (H) sonography demonstrates that the lump is an oval mass. (I) Although most of the margins of the palpable sono-graphic mass are well defined, close inspection reveals subtle irregularity of the border (arrow). This palpable lump is infiltrating mucinous carcinoma. (G) The irregular mammographic mass corresponds to (J) an irregular sonographic mass that is infiltrating ductal carcinoma. If the mass has any other sonographic characteristics, then it is category 4 or 5. Examples of these lesions include (1) solid masses within cysts, (2) masses that have any other shape or that are microlobulated, (3) lesions that exhibit heterogeneous echogenicity or that present as a focal area of intense shadowing, (4) tumors with either completely or partially ill-defined margins, and (5) masses associated with other sonographic abnormalities such as architectural distortion. Masses with microlobulations or other shapes that cannot be classified as circumscribed should be considered irregular in shape (see Chapters 7 and 8
 General Overview
General Overview
 Patterns of Mammographic Abnormality
Patterns of Mammographic Abnormality
Masses
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree