The elbow is complex in its multiple articulations, which allow for flexion and extension, as well as supination and pronation. Imaging of the pediatric elbow is deceptively simple: two conventional radiographic orthogonal views are all that is required to diagnose most pediatric elbow fractures. The challenge lays in the radiographic interpretation of a joint with evolving ossification whose appearance changes significantly as the child’s skeleton matures.
Elbow injuries are quite common in childhood; pediatric elbow fractures account for approximately 15% of all childhood fractures. The child’s upper extremity is central to their development, permitting babies to feed themselves and explore their environment. As a toddler and young child, the upper extremity plays an essential role in the child’s ability to play and climb, simultaneously protecting them during falls. In adolescence the elbow has vital functions in many popular sports. Patterns of injury change as the child evolves from a curious toddler discovering their world to the monkey bar champion of the elementary-school playground, from first gymnastics classes and little league games to playing on competitive traveling teams.
Part 1: Imaging Basics
What Are the Standard Radiographic Views of the Pediatric Elbow?
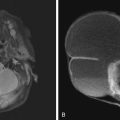
Anteroposterior (AP) and lateral projections are the standard radiographic views obtained in the evaluation of the pediatric elbow. The AP view is performed in full extension, with the forearm supinated. The lateral view is acquired with the elbow flexed at 90 degrees, the forearm in neutral position, with the wrist in a true lateral position, thumb up. Obtaining a true lateral is essential for accurate interpretation. Recognizing the hourglass or figure-of-eight morphology of the distal humerus is a quick technique for confirming adequate positioning of the lateral radiograph ( Fig. 13.1 ).

When Are Additional Views Helpful?
Oblique views can occasionally be helpful for specific injuries, including lateral condyle and medial epicondyle fractures. Comparison views of the contralateral elbow are occasionally helpful, particularly in the case of distinguishing a fracture from an ossification variant. In the majority of cases, however, additional views are not necessary.
When Are Other Imaging Modalities Useful?
When additional imaging evaluation is required, ultrasound and/or magnetic resonance imaging (MRI) is often the next imaging modality. Ultrasound is user/technologist and site dependent. The use of ultrasound, however, should always be considered, particularly in younger children who may require sedation for MRI. MRI is most commonly used in athletes with chronic repetitive injuries, although radiographs should always be acquired first. For traumatic injuries, acute or chronic, MRI is typically performed either without contrast or after arthrography. Indications for MRI with intravenous contrast include evaluation for infection, inflammatory arthritis, and/or masses. Computed tomography (CT) is rarely indicated.
Part 2: Approach to the Pediatric Elbow Radiograph: FOOL Checklist
Conventional radiography is the primary imaging tool used for the accurate diagnosis and management of children with elbow injuries. The unique and evolving radiographic appearance of the pediatric elbow can be challenging. Outlined here is an approach that aims to improve diagnostic accuracy and prevent one from looking like a “FOOL” ( Box 13.1 ).
- ▪
F = fat pads
- ▪
O = overt findings and outlines
- ▪
O = ossification centers
- ▪
L = lines
F: Fat Pads: Joint Effusion = Fracture (Most Likely)
Displacement of the fat pads indicates the presence of a joint effusion. A positive fat pad sign indicates high likelihood for fracture.
What Is the Significance of the Posterior Fat Pad Sign?
Presence of a posterior fat pad sign is always abnormal. The posterior fat pad is anatomically positioned within the intercondylar depression (olecranon fossa) of the distal humerus, and in the normal elbow it is obscured by overlying bone on the lateral radiograph (see Fig. 13.1 ). In the presence of a joint effusion the posterior fat pad is displaced posteriorly, allowing for its visualization ( Fig. 13.2 ). The presence of a posterior fat pad raises significant suspicion for a fracture.

What Is the Significance of the Anterior Fat Pad?
Presence of the anterior fat pad can be normal or abnormal. The anterior fat pad is normally visualized in all patients. Ordinarily it hugs the anterior cortex of the distal humerus (see Fig. 13.1 ). It too can be displaced by a joint effusion, and in this setting is often more prominent or elevated (“sail sign”) away from the anterior cortex of the distal humerus (see Fig. 13.2 ). Determining whether an anterior fat pad sign is present is a less reliable and more subjective tool than the posterior fat pad sign.
What If Positive Fat Pad and No Fracture Line Is Identified?
In the setting of trauma, the presence of a joint effusion as evidenced by displacement of the fat pads, is highly suspicious for fracture. In a retrospective study, joint effusions were identified in 91 percent of pediatric patients with elbow fractures. The presence of a displaced posterior fat pad should therefore prompt a rigorous, magnified search for any subtle fracture. Even if no fracture is identified on initial radiographs, most patients with isolated post traumatic joint effusions are treated as probable occult fractures with posterior elbow splinting and follow-up.
O: Overt Findings and Outlines
First the forest, then the trees: Always evaluate for obvious soft tissue injuries and obvious fractures and/or dislocations. This is akin to the physical examination and sets pretest probability of an abnormality. For example, patients with medial epicondyle avulsion fractures typically present with marked medial soft tissue swelling. Even if a fracture is not initially detected, the abnormal soft tissue swelling prompts a closer inspection. Occasionally, honing in on a small osseous finding may distract from the bigger picture. Soft tissue swelling and inflammatory stranding are important to note, particularly because radiologists often do not examine the child and may have a limited history. Use soft tissue clues to get a general gestalt of whether the study is normal or abnormal.
After general characterization of the forest, scrutinize individual trees. Trace outlines of each bone, particularly the distal humerus and proximal radius, for any subtle contour deformities and/or buckle fractures. Examples of subtle abnormalities seen in common fractures include subtle cortical disruptions in supracondylar and lateral condyle fractures and mild cortical buckling of the proximal radius in radial neck fractures.
O: Ossification Centers
Radiographic evaluation of the pediatric elbow is unique due to the variable appearance of the ossification centers about the elbow, which undergo transformation from cartilaginous at birth, progressively ossifying, and subsequently fusing during childhood and adolescence.
What Is the Significance of CRITOE?
There are six centers of secondary ossification in children. At birth, these centers are all cartilaginous, and therefore not visible by plain radiography until they begin to ossify. The age at which ossification and fusion occur varies, but fortunately the sequence of ossification is predictable: Capitellum, Radial head, Internal (medial) epicondyle, Trochlea, Olecranon, External (lateral) epicondyle (CRITOE). Familiarity with this pattern is critical to the interpretation of pediatric elbow radiographs ( Boxes 13.2 and 13.3 ) ( Fig. 13.3 ).
- ▪
C = capitellum
- ▪
R = radial head
- ▪
I = internal (medial) epicondyle
- ▪
T = trochlea
- ▪
O = olecranon
- ▪
E = external (lateral) epicondyle
- 1.
Ossification centers appear and fuse earlier in girls than boys.
- 2.
Capitellum ossifies first, often by 6 months of age, and is typically well formed by 1 year of age in both girls and boys.
- 3.
Lateral epicondyle ossifies last, typically by 10–12 years of age.
- 4.
Medial epicondyle is the last ossification center to fuse to the distal humerus, typically during mid to late teenage years.
- 5.
Trochlea, lateral epicondyle, and olecranon have multiple ossification centers and can normally appear fragmented or irregular.
- 6.
Variants include CIRTOE and CRIOTE.

Knowing the exact age at which ossification occurs is less important than sequence, with both ethnic and sex variability. A general rule of thumb used by some is 1-3-5-7-9-11 years. Girls ossify and fuse earlier than boys by an average of 2 years.
When Is CRITOE Most Useful?
If the sequence of CRITOE is abnormal, this raises suspicion for a traumatic avulsion fracture with displacement. This is most commonly seen with medial epicondyle avulsion fractures that may displace into the medial joint space, mimicking a trochlear ossification center. Thus, if a “trochlear” ossification center is identified without a medial epicondyle, the “trochlea” is most likely an avulsed medial epicondyle fragment.
Are There Any Variants of CRITOE?
Variants of CRITOE are rare but have been reported. One of the more common ossification sequence variants includes the appearance of the medial epicon dyle before the radial head, more commonly in girls (CIRTOE) ( Fig. 13.4 ). Case reports also include the olecranon before the trochlea (CRIOTE). In these rare cases, comparison with the contralateral elbow may be useful when the clinical history and imaging findings are not congruent. However, normal development can also be asymmetrical.

L: Lines
The anterior humeral line (AHL) and the radiocapitellar line (RCL) confirm normal alignment of the elbow. Disruption of either line is suspicious for fracture and/or dislocation. Remember that proper positioning of the elbow is paramount to avoiding pitfalls, particularly the lateral view; otherwise, the use of these lines can be misleading. In addition, both the AHL and RCL are less reliable in infants and toddlers, related to small and possibly eccentric ossification centers seen during early stages of physiologic ossification.
What Is the Anterior Humeral Line?
The AHL is a vertical line drawn parallel to the anterior cortex of the distal humerus on the lateral radiograph. This line normally bisects the middle third of the capitellum ( Fig. 13.5A ). Disruption of this line is suggestive, but not pathognomonic, for a supracondylar fracture (see Fig. 13.5B ).

What Is the Radiocapitellar Line?
The RCL is a vertical line drawn parallel through the central shaft of the proximal radius toward the elbow on both the AP and lateral views ( Fig. 13.6 ). The RCL should intersect the capitellum on both radiographic views, but it has been shown to be more reliable on the lateral view. Studies have demonstrated that the RCL is most accurate when drawn along the central shaft of the radial neck, rather than the proximal radial diaphysis, because of the mild normal angulation at the proximal radial metaphyseal–diaphyseal junction. The radial neck landmark should be used for both lateral and AP views. An abnormal RCL is characteristic of a radial head dislocation, as can be seen in the Monteggia fracture/dislocation. It is also abnormal in displaced lateral condyle fractures. Both of these fractures are described and illustrated in more detail later.

Are There Any Exceptions to the Anterior Humeral Line?
Proper positioning is paramount. A true lateral view is particularly necessary for the diagnostic accuracy of AHL. In younger children (<2.5 years old) the AHL may not be as reliable, frequently crossing the anterior third of the capitellum.
Are There Any Exceptions to the Radiocapitellar Line?
Studies validating the RCL have shown it to be reliable in 84% to 95% of children. It is most accurate on lateral radiographs and in older children (>5 years old). This may be explained by the fact that the ossification pattern of the capitellum in growing children begins in an eccentric location. As described earlier, reliability is most consistent when drawn parallel to the radial neck.
Part 3: Acute Pediatric Elbow Injuries
Radial Head Subluxation (Nursemaid’s Elbow)
Radial head subluxation is one of most common acute pediatric orthopedic injuries. The injury is unique to children, with most occurring in toddlers (peak incidence 2–3 years old). The injury has several colorful nicknames, including nursemaid’s elbow, pulled elbow, supermarket elbow, and temper tantrum elbow. The typical mechanism of injury occurs when a caretaker (“nursemaid”) pulls a young child’s pronated forearm while extended at the elbow, classically a sudden tug on the child’s arm, perhaps to prevent a fall. The left arm is affected more frequently, attributed to right hand dominance of caretakers. The sudden traction on the arm results in disruption of the annular ligament from its periosteal attachment to the radial head; the detached annular ligament then interposes between the radial head and capitellum. The annular ligament attachment is weak in young children, becoming stronger in later childhood, thus explaining the preponderance of this injury in toddlers. The second most common mechanism of injury is a fall.
The chief complaint in children presenting to the emergency department in a retrospective review by Schunk (1990) was “not using the arm,” with the majority of children described as in a good mood (81% of cases). In most cases, reduction maneuvers by an experienced clinician either with supination/flexion or hyperpronation techniques can be performed in an office setting or in the emergency department without sedation. With successful reduction the child’s symptoms usually immediately resolve. Recurrent subluxations can occur ( Box 13.4 ).
- ▪
Most common pediatric elbow injury, often not requiring imaging
- ▪
Toddlers: most commonly 1–4 years old
- ▪
Classic mechanism (50%): sudden longitudinal pull on child’s arm by parent/caretaker
- ▪
Most common presentation: refuses to use arm, usually in an otherwise happy child, no or minimal focal tenderness or swelling
- ▪
Radiographs: typically normal; sometimes disruption of the radiocapitellar line
What Is the Role of Imaging in Radial Head Subluxation? What If the Clinician Suspects Radial Head Subluxation But the Radiographs Are Normal?
In the majority of cases, radial head subluxation is diagnosed clinically. Radiographs are typically not necessary if the history and physical examination are consistent with the diagnosis. Indications for imaging include atypical presentation, focal pain and/or tenderness, swelling, and/or inability to reduce. In these cases, imaging is useful to exclude other causes of elbow pain, such as fracture.
Radiographs are normal in most cases with a history of nursemaid’s elbow/radial head subluxation, because the injury is often reduced before imaging. However, occasionally RCL displacement is identified with lateral subluxation of the radial head on the AP view and/or posterior subluxation on the lateral view. Joint effusions can be seen. Imaging does not change treatment, management, or outcome of radial head subluxation.
Can Radial Head Subluxation Occur in Infants 6 Months and Younger?
Yes, although this is rare. Typical history in this younger age group includes pain after either a pull/lift during play or while rolling over. The latter mechanism is thought to be secondary to the forearm getting trapped under the baby’s body, simulating a tug.
Common Pediatric Elbow Fractures
Pediatric elbow fractures are common, accounting for approximately 15% of all childhood fractures ( Boxes 13.5 and 13.6 ).
- 1.
Supracondylar
- 2.
Lateral condyle
- 3.
Medial epicondyle avulsion
- 4.
Radial neck
- ▪
Medial condyle
- ▪
Lateral epicondyle
- ▪
Radial head
- ▪
Olecranon apophyseal avulsion fractures (50% occur in osteogenesis imperfecta)
Supracondylar Fracture Overview
The supracondylar fracture accounts for 50% to 70% of all pediatric elbow fractures. The majority occur from a fall on an extended arm, commonly occurring in active toddlers and elementary-school children.
Typically, supracondylar fractures are most apparent on the lateral radiograph, although often identified on the AP view as well. With hyperextension, the distal humerus fractures across an area of relative weakness, demarcated by the “hourglass configuration” of the distal humerus seen on lateral radiographs, formed by the coronoid and olecranon fossa. When the child falls with arm extended, force on the distal humerus hinges against the olecranon, frequently resulting in posterior angulation/displacement of the distal fracture fragment. The degree of posterior displacement governs classification and treatment. Nondisplaced fractures can be subtle; always checking the AHL, particularly in the presence of a joint effusion, often aids in the detection of a subtle fracture. Gartland type 1 fractures are nondisplaced and are treated conservatively with casting ( Fig. 13.7 ). Gartland type 2 fractures are displaced with intact posterior cortex ( Fig. 13.8A ). Gartland type 3 fractures are displaced with disruption of the posterior cortex (see Fig. 13.8B ). Gartland type 2 and 3 fractures often require operative reduction and percutaneous pinning.


Rarely, supracondylar fractures occur from a flexion-type mechanism, typically from a direct blow to a flexed elbow. In these cases the distal fracture fragment may be anteriorly displaced.
Complications of supracondylar fracture include neurovascular compromise, residual deformity, and rarely, compartment syndrome. About 10% to 15% of patients present with neuropraxia, most commonly involving the anterior interosseus and median nerves. Fortunately, the majority of nerve injuries are stretch injuries, often transient, and rarely require treatment. Compartment syndrome is a rare but serious complication that mandates emergent surgery. Studies have shown that children with brisk capillary refill and warm pink hands even in the setting of diminished radial pulses are unlikely to have a true compartment syndrome ( Box 13.7 ).