Use of image-guidance allows safe and precise percutaneous placement of needles for various diagnostic and therapeutic procedures in the head and neck region. This review describes the anatomy relevant to safe-access route planning and the techniques, advantages, and limitations associated with various approaches used for percutaneous needle placement in different head and neck regions. Subzygomatic, retromandibular, paramaxillary, submastoid, transoral, and posterior approaches can be used for percutaneous access in the suprahyoid head and neck region, including skull base and upper cervical vertebrae. In the infrahyoid portion of the neck and for lower cervical vertebrae, access can be achieved via the anterolateral (between the airways and the carotid sheath), posterolateral (posterior to the carotid sheath), and direct posterior approaches.
Image-guided percutaneous needle placement is required for various diagnostic and therapeutic procedures, including biopsies, ablation procedures, and nerve root and ganglion blocks, in the head and neck region. A thorough knowledge of the anatomy of this region is essential for planning a safe route of access for needle placement in deep-seated head and neck lesions because major vessels, nerves, the airway, or osseous structures often intervene in the projected needle path. In this article, we review the various approaches that can be used for percutaneous needle placement in the head and neck region, focusing on the relevant anatomy, technical aspects, and the advantages and limitations of each approach.
Anatomy
For the purpose of this discussion, it is useful to describe the anatomy in terms of various fascial planes and intervening spaces that exist in the head and neck region, and focus on the important osseous, muscular, vascular, and neural structures that are contained within these fascial spaces. The head and neck area can be divided into suprahyoid and infrahyoid regions. The important fascial spaces in the suprahyoid region include the parapharyngeal, masticator, parotid, carotid, pharyngeal mucosal, retropharyngeal, and perivertebral spaces. In the infrahyoid neck, apart from the inferior extensions of the carotid, retropharyngeal, and perivertebral spaces, three other spaces, namely the visceral and the posterior and anterior cervical spaces, can be identified.
The parapharyngeal space is a pyramidal-shaped fat-containing potential space that extends from the hyoid bone inferiorly to the skull base superiorly, and is bordered by the masticator space anteriorly, the deep parotid space laterally, the pharyngeal mucosal space medially, the carotid space posteriorly, and the lateral extension of the retropharyngeal space posteromedially. The major neurovascular structures that traverse this space include the internal maxillary, middle meningeal, and ascending pharyngeal arteries; the pterygoid venous plexus; and branches of the mandibular nerve.
The pharyngeal mucosal space is medial to the parapharyngeal space and is located deep to the buccopharyngeal fascia in the nasopharynx and oropharynx and contains mucosa, lymphoid tissue, minor salivary glands, and pharyngeal constrictor muscles.
The masticator space extends from the mandible up to the skull base, and has two components: the infratemporal fossa below the zygomatic arch and the temporal fossa above it. Spaces that border the masticator space include the buccal space anteriorly, the parotid space posteriorly, and the parapharyngeal space posteromedially. The contents of the masticator space include the medial and lateral pterygoid, masseter, and temporalis muscles, the ramus and body of the mandible, and the inferior alveolar branch of the mandibular nerve and the inferior alveolar vessels.
The carotid space extends from the skull base to the aortic arch, and contains the common or the internal carotid artery (depending on the level); the internal jugular vein; sympathetic plexus; cranial nerves IX, X, XI, and XII in the nasopharyngeal portion; cranial nerve X in the oropharyngeal portion and infrahyoid neck; and lymph nodes. The parapharyngeal space forms the anterior boundary of the carotid space in the suprahyoid neck.
The parotid space is located lateral to the parapharyngeal space and posterolateral to the masticator space, extending from the level of the external auditory canal down to the angle of the mandible. The posterior belly of the digastric muscle separates the medial portion of the parotid space from the anterolateral aspect of the carotid space. Apart from the parotid gland, the space contains facial nerve, external carotid artery, retromandibular vein, and lymph nodes.
The retropharyngeal space, which contains fat and lymph nodes only, is a midline space located between the pharyngeal constrictor muscle anteriorly and prevertebral muscles posteriorly. This space extends laterally up to the carotid space.
The perivertebral space lies beneath the deep layer of deep cervical fascia and extends from the skull base to the fourth thoracic vertebral level. The prevertebral portion of this space contains the prevertebral muscles, the vertebral artery and vein, the scalene muscles, the brachial plexus, the phrenic nerve, and the vertebral body, transverse process, and pedicle, whereas the paravertebral portion of this space contains the paravertebral muscles and posterior elements of the cervical vertebrae.
The visceral space is bounded by the middle layer of the deep cervical fascia, extends from the hyoid bone to the mediastinum, and contains the thyroid and parathyroid glands, larynx, hypopharynx, esophagus, trachea, recurrent laryngeal nerve, and lymph nodes. The posterior cervical space is located posterior to the carotid space and lateral to the perivertebral space, and contains the spinal accessory nerve and the preaxillary portion of the brachial plexus. The anterior cervical space, which is located lateral to the visceral space and anterior to the carotid space, does not contain any important structure.
Image guidance
Image guidance is generally required for various percutaneous procedures in the head and neck region in nonpalpable deep-seated head and neck lesions. Superficial neck nodes, thyroid lesions, and parotid gland lesions can be accessed with sonographic guidance. However, the lack of an adequate acoustic window because of overlying bony structures such as the maxilla, mandible, mastoid, and the styloid process and the air-containing aerodigestive system preclude the use of sonographic guidance for many deep-seated head and neck lesions. Fluoroscopy is routinely used for guiding vertebroplasty and discography procedures for cervical spine. Although fluoroscopic-guided needle placement has been used for nerve root and ganglion blocks and for biopsy of cervical spine and skull base lesions, inability to visualize the intervening structures increases the risk of complications. CT, with its high spatial and contrast resolution, is the imaging modality of choice for percutaneous needle placement in nonpalpable deep-seated head and neck lesions. Air-containing spaces and bony structures do not result in significant image degradation, especially with the use of thin-section collimation. CT allows for excellent delineation of intervening vital structures, permitting safe biopsy path planning. Magnetic resonance imaging (MR imaging), because of its high contrast resolution, its multiplanar imaging capacity allowing the use of double oblique approaches, and its ability to visualize vessels without a contrast agent, has also been used for guiding needle placement in head and neck lesions. However, the limited availability of open-configuration MR imaging systems, high cost, longer acquisition times, and need for MR imaging–compatible needles has prevented more widespread use of MR imaging guidance for these procedures.
Image guidance
Image guidance is generally required for various percutaneous procedures in the head and neck region in nonpalpable deep-seated head and neck lesions. Superficial neck nodes, thyroid lesions, and parotid gland lesions can be accessed with sonographic guidance. However, the lack of an adequate acoustic window because of overlying bony structures such as the maxilla, mandible, mastoid, and the styloid process and the air-containing aerodigestive system preclude the use of sonographic guidance for many deep-seated head and neck lesions. Fluoroscopy is routinely used for guiding vertebroplasty and discography procedures for cervical spine. Although fluoroscopic-guided needle placement has been used for nerve root and ganglion blocks and for biopsy of cervical spine and skull base lesions, inability to visualize the intervening structures increases the risk of complications. CT, with its high spatial and contrast resolution, is the imaging modality of choice for percutaneous needle placement in nonpalpable deep-seated head and neck lesions. Air-containing spaces and bony structures do not result in significant image degradation, especially with the use of thin-section collimation. CT allows for excellent delineation of intervening vital structures, permitting safe biopsy path planning. Magnetic resonance imaging (MR imaging), because of its high contrast resolution, its multiplanar imaging capacity allowing the use of double oblique approaches, and its ability to visualize vessels without a contrast agent, has also been used for guiding needle placement in head and neck lesions. However, the limited availability of open-configuration MR imaging systems, high cost, longer acquisition times, and need for MR imaging–compatible needles has prevented more widespread use of MR imaging guidance for these procedures.
Complications
Image-guided percutaneous needle placement for various head and neck procedures is rarely associated with major complications. A thorough knowledge of the cross-sectional anatomy of the head and neck region and careful attention to access trajectory planning minimize the chances of injury to major neural and vascular structures. Minor complications including pain, vasovagal reaction, minor infection, and minor bleeding have been reported. Transient recurrent laryngeal nerve damage has been reported. Trauma to the trachea and esophagus can result in mediastinal or surgical emphysema. Injury to the lung and pleura may occur resulting in pneumothorax, which may require chest tube placement. Review of literature revealed one case report of maxillary artery pseudoaneurysm after needle biopsy of the masticator space lesion.
Approaches used for percutaneous access in suprahyoid head and neck
Subzygomatic (Infratemporal, Transcondylar, Sigmoid Notch) Approach
The subzygomatic approach is ideally suited for accessing lesions in the masticator space. In addition to lesions in the infrazygomatic portion of the space, lesions in the suprazygomatic portion (temporal fossa) of the masticator space and the skull base can also be accessed with this approach by using a cranial needle angulation. This approach also allows easy access to lesions in the parapharyngeal, pharyngeal mucosal, and retropharyngeal spaces and the prevertebral portion of the perivertebral space. Furthermore, this approach is used for needle placement in the pterygopalatine fossa for neurolysis of the pterygopalatine ganglion for pain management.
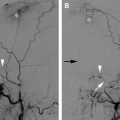
The needle is inserted below the zygomatic arch and is advanced through the intercondylar (sigmoid) notch between the coronoid process anteriorly, the mandibular condyle posteriorly, and the superior border of the mandibular ramus inferiorly. The needle can easily be angulated in various directions (anterior, posterior, cranial, or caudal), permitting access to multiple target sites. The needle traverses the masticator and the parapharyngeal spaces for lesions located in the pharyngeal mucosal, retropharyngeal, and prevertebral spaces and skull base lesions ( Fig. 1 ). Cranial needle angulation allows the subzygomatic approach to be used for accessing lesions in the skull base and the suprazygomatic portion of the masticator space. A triangulation method can be used to estimate the required needle angle from contiguous axial CT scans obtained from the level of the planned skin entry site to the level of the target lesion. The needle is inserted below the level of the zygomatic arch and advanced cranially and medially; the needle tip position and angulation are checked with intermittent axial CT scans ( Fig. 2 ). Alternatively, a change in the degree of neck flexion can bring the target lesion and the skin entry site into the same axial plane, allowing visualization of the entire needle length in a single axial CT image. Tilting the gantry 10 degrees caudally can also be used to facilitate needle placement in skull base lesions. Occasionally, if passage of need through the notch is difficult, having the patient keep his or her mouth open, preferably with a bite block, can help open up the space between the mandible and the zygomatic arch, facilitating needle insertion.
The structures that could potentially be injured with this needle trajectory include the mandibular branch of the trigeminal nerve and the internal maxillary artery and its branches, including the middle meningeal artery. The needle passes through or in between the pterygoid plexus of veins, which is found partly between the temporalis and lateral pterygoid and partly between the two pterygoid muscles. The origin of the maxillary artery from the external carotid artery is embedded in the parotid gland posterior to the neck of the mandible. The mandibular part of the artery runs horizontally forward along the medial surface of the ramus and the pterygoid part ascends forward and medially, located either superficial (60%) or deep (40%) to the lateral pterygoid muscle, to enter the pterygopalatine fossa through the pterygomaxillary fissure. The mandibular part gives origin to the middle meningeal artery, which ascends in the posterior part of the sigmoid notch deep to the lateral pterygoid muscle to enter the foramen spinosum. After exiting the cranial cavity through the foramen ovale, the mandibular nerve descends in the posterior part of the intercondylar notch (medial to the lateral pterygoid muscle and anterior to the neck of the mandible) to reach the inner surface of the mandibular ramus. However, the risk of major injury to the vessels or the nerves is extremely low.
Retromandibular (Transparotid) Approach
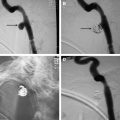
Lesions in the deep parotid space, parapharyngeal space, pharyngeal mucosal space, and lower part of the retropharyngeal space are accessible via a retromandibular approach. This approach can also be used for targeting lesions in the carotid sheath, if the vessels are displaced medially by the mass.
With this approach, the needle is inserted posterior to the mandible and anterior to the mastoid process and advanced through the parotid gland ( Fig. 3 ). The external carotid artery and the retromandibular vein, which are located within the parotid gland immediately posterior to the mandibular ramus, should be avoided. The external carotid artery, after exiting the carotid sheath, turns laterally and passes anterior to the posterior belly of the digastric muscle to reach the parotid gland. Within the substance of the parotid gland, it is located medial to the retromandibular vein, and ascends behind the condyle before dividing into the superficial temporal and maxillary arteries. The facial nerve as it courses through the parotid gland is located lateral to the retromandibular vein. The needle should be kept anterior to the styloid process to avoid injury to the internal carotid artery, which is located posterior to the styloid process. Occasionally, however, medial displacement of the carotid vessels by mass lesions may allow the needle to be advanced posterior to the styloid process.