Chapter 11 Arrhythmias
Arrhythmogenic right ventricular cardiomyopathy (ARVC)
Catheter ablation of arrhythmias
Arrhythmias
Background
Cardiac imaging is an important part of the investigation of patients with cardiac arrhythmia. There are many structural cardiac conditions that can predispose to the development of cardiac rhythm problems. As treatment moves away from long-term medication to curative catheter ablation, information from echocardiography, computed tomography (CT) and cardiac magnetic resonance (CMR) are increasingly being used to plan as well as guide procedures.
Palpitation
‘Palpitation’ is defined as a patient’s awareness of an abnormal heartbeat. A combination of history, physical examination, surface 12-lead ECGs, and ambulatory ECGs is usually adequate to make a diagnosis. It is important to establish whether the symptoms are a result of structural heart disease. For this reason, transthoracic echocardiography is central in the diagnostic algorithm. Abnormalities of left ventricular size and function can be seen. Left atrial enlargement is common in patients with atrial fibrillation (AF). Occasionally CMR is required for further structural assessment of the myocardium in suspected cardiomyopathy.
Syncope
Syncope is ‘A transient, self-limited sudden loss of consciousness, usually leading to falling’. Syncope can be caused by a wide spectrum of conditions, ranging from the benign faint to potentially fatal cardiac arrhythmias. Imaging is guided by the clinical history and examination findings. For example, a patient with a systolic murmur may require transthoracic echocardiography to exclude aortic stenosis or hypertrophic cardiomyopathy. A patient presenting with syncope and unequal blood pressures in the upper limbs may have aortic dissection, and cross-sectional imaging might be considered.
Atrial arrhythmias
An understanding of the mechanism by which atrial tachyarrhythmias are initiated and sustained is important in developing strategies to plan and perform catheter ablation procedures. Arrhythmias involving the atria can be divided into those contained completely in the atria and those requiring activation of both the atrium and ventricle.
Atrial tachycardia
Atrial focus of cells firing faster than the sinoatrial node. Catheter ablation can offer a cure in symptomatic drug-refractory cases.
Atrial flutter
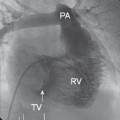
Typically there is a re-entry circuit within the right atrium which can be interrupted by ablating a series of lesions, creating a conduction block between the inferior vena cava and tricuspid valve. Re-entry circuits may also be found in the left atrium.
Atrial fibrillation (Figs. 11.1 and 11.2)
AF is the most common cardiac arrhythmia, affecting 1% of the population. There is chaotic electrical activation of the atria resulting in loss of coordinated contractile function. This can be from a single focus of cells with enhanced automaticity or from a single or several micro-re-entry circuits that depolarize rapidly, creating self-perpetuating waves of electrical activity with variable conduction resulting in fibrillation. AF ablation strategies are targeted at electrically isolating the four pulmonary veins from the left atrium. These are required to sustain the multiple re-entry circuits that lead to AF. Electrical signals in the superior vena cava and coronary sinus are additional targets.
Cardiovascular imaging
Atrial arrhythmias often occur in patients with structurally normal hearts, but echocardiography should be arranged to exclude underlying cardiomyopathy and to examine valvular function and atrial size. Further imaging is then planned based on findings of additional pathology.
AF can be associated with pulmonary conditions such as pulmonary embolism and pneumonia, and therefore additional imaging of the lungs with chest X-ray or CT may be required if clinically suspected.
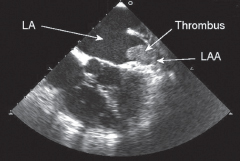
In patients presenting with AF in whom electrical cardioversion is being considered, a transoesophageal echocardiogram can help to exclude a left atrial appendage thrombus.
Fig. 11.1 Transoesophageal echocardiogram of the left atrium (LA) demonstrating a thrombus in the left atrial appendage (LAA). It is believed that >90% of strokes in AF result from emboli originating in the LAA.
Supraventricular tachycardia
Atrioventricular re-entry tachycardia (AVRT)
 Usually requires the AV node and at least one accessory pathway (AP) between the atrium and the ventricle to set up a re-entry circuit, or two accessory pathways without the participation of the AV node.
Usually requires the AV node and at least one accessory pathway (AP) between the atrium and the ventricle to set up a re-entry circuit, or two accessory pathways without the participation of the AV node.
 Where there is evidence of pre-excitation caused by an AP on the resting ECG, i.e. a short P–R interval and delta wave, the patient is said to have a Wolffe–Parkinson–White (WPW) abnormality. If the patient develops AVRT, they are said to have WPW syndrome.
Where there is evidence of pre-excitation caused by an AP on the resting ECG, i.e. a short P–R interval and delta wave, the patient is said to have a Wolffe–Parkinson–White (WPW) abnormality. If the patient develops AVRT, they are said to have WPW syndrome.
 Patients with AVRT due to an AP that only conducts retrograde are said to have a concealed pathway, as there is no evidence of it on the resting ECG.
Patients with AVRT due to an AP that only conducts retrograde are said to have a concealed pathway, as there is no evidence of it on the resting ECG.
 Catheter ablation of the AP offers a cure for AVRT.
Catheter ablation of the AP offers a cure for AVRT.
Atrioventricular nodal re-entry tachycardia (AVNRT)
 Re-entry circuit is contained entirely within the AV node.
Re-entry circuit is contained entirely within the AV node.
 Dual conduction pathways within the AV node, typically a slow and fast pathway, allow electrical impulses to recycle and sustain the arrhythmia.
Dual conduction pathways within the AV node, typically a slow and fast pathway, allow electrical impulses to recycle and sustain the arrhythmia.
 In drug refractory or intolerant cases catheter ablation offers a cure.
In drug refractory or intolerant cases catheter ablation offers a cure.
Cardiovascular imaging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree