Autoimmune (IgG4) Pancreatitis
Brooke R. Jeffrey, MD
Michael P. Federle, MD, FACR
Key Facts
Terminology
Autoimmune form of chronic pancreatitis responding dramatically to steroid therapy
Imaging
Diffusely or focally enlarged pancreas with “halo” of low density (intensity)
Sausage-like; loss of fatty lobulation
ERCP with long strictures or discontiguous strictures
Top Differential Diagnoses
Pancreatic ductal carcinoma
Significant dilatation of main pancreatic duct proximal to narrowed segment
Atrophy of distal parenchyma
Chronic pancreatitis
Pain is chief complaint of patient
Calcifications and pseudocyst are common findings
Chronic alcohol abuse in most
Pathology
2 distinct histologic subtypes (core biopsy not FNA is best for diagnosis)
Type 1: Dense lymphoplasmacytic infiltration and positive staining for IgG4
Often associated with other autoimmune diseases (cholangitis, thyroiditis, etc.)
Type 2: Periductal neutrophilic infiltrate with granulocyte-epithelial lesions and negative IgG4 staining
Clinical Issues
Lab findings: ↑ ↑ IgG4 (sensitive and specific), normal or ↑ serum amylase/lipase, ↑ ALP/GGT, ↑ bilirubin, ↑ ANA, ↑ autoantibodies, ↑ CA 19-9
Type 1 patients may have thyroiditis, dry eyes and mouth from Sjögren syndrome
TERMINOLOGY
Abbreviations
Autoimmune pancreatitis (AIP)
Synonyms
Lymphoplasmacytic sclerosing pancreatitis; primary sclerosing pancreatitis; nonalcoholic, duct-destructive, chronic pancreatitis
Definitions
Pancreatic involvement with fibroinflammatory disease responding dramatically to steroid therapy
IMAGING
General Features
Best diagnostic clue
Diffusely or focally enlarged pancreas with “halo” of low density (or signal intensity)
No vascular involvement, calcification, or pseudocyst
Lack of significant dilatation of main pancreatic duct
Location
May be focal and mass-forming, multifocal or diffuse
Morphology
“Sausage-shaped” appearance of body and tail of pancreas
Imaging Recommendations
Best imaging tool
MRCP and gadolinium-enhanced MR
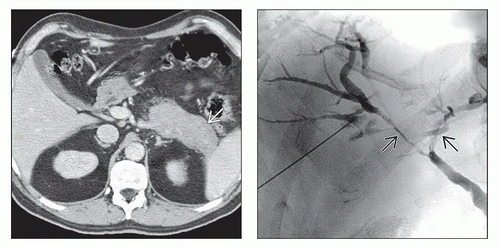
CT Findings
Enlargement of pancreas
Usually diffuse, can be focal swelling
Sausage-shaped, loss of fatty lobulation
Enhancement is variable
Often less enhancement than expected in arterial phase
Diffuse or segmental narrowing of pancreatic duct
Low-attenuation “halo” surrounds pancreas
Minimal peripancreatic stranding
Stricture of common bile duct ± intrahepatic ducts
Indistinguishable from primary sclerosing cholangitis
MR Findings
Diffuse enlargement with low signal on T1WI
“Halo” of low signal on T2WI
Capsule-like rim of peripheral enhancement
Delayed enhancement of focal or diffuse parenchymal lesions
Multiple discontiguous strictures of main pancreatic duct and bile ducts on MRCP
Biliary strictures may simulate findings of primary sclerosing cholangitis
Ultrasonographic Findings
May have normal appearance on US
Diffusely enlarged hypoechoic gland with sausage-like appearance
Other Modality Findings
ERCP
Diffuse or segmental narrowing of main pancreatic duct
Long narrow strictures typically greater than 1/3 length of pancreatic duct
Lack of upstream dilatation of pancreatic duct distal to stricture
Multiple discontiguous strictures of pancreatic duct
Side branch ducts arising from stricture
DIFFERENTIAL DIAGNOSIS
Pancreatic Ductal Carcinoma
Significant upstream dilatation of main pancreatic duct distal to narrowed segment
Atrophy of parenchyma distal to mass
Encasement of major peripancreatic vessels
Chronic Pancreatitis
Pain is chief complaint of patient
Chronic alcohol abuse in most
Calcifications and pseudocysts are common findings
PATHOLOGY
General Features
Etiology
Unknown; autoimmune
Unclear whether IgG4 plays a pathogenic role in type 1 or is only an epiphenomenon
Genetics
Genetic studies suggest association with a specific human leukocyte antigen (HLA) type
Associated abnormalities
Often associated with other fibroinflammatory autoimmune diseases
Sjögren syndrome, sclerosing cholangitis, primary biliary cirrhosis, ulcerative colitis, SLE, thyroiditis
Staging, Grading, & Classification
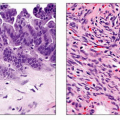
2 distinct histologic subtypes (core biopsy not FNA is best for diagnosis)
Type 1: Lymphoplasmacytic sclerosing pancreatitis (IgG4-related pancreatitis)
Serum IgG4 elevated twice normal in 80%
Mean age at presentation: 7th decade
Presentation: Obstructive jaundice 75%, acute pancreatitis 25%
Positive IgG4 tissue staining
Multiple organs involved in 60%
IBD in only 2-6%
Relapses after steroid therapy frequent
Imaging: Diffuse involvement of pancreas in 40% with focal lesions in 60%
Type 2: Idiopathic duct centric pancreatitis with granulocyte-epithelial lesions
Serum IgG4 not elevated
Mean age at presentation: 5th decade
Presentation: Obstructive jaundice 50%, acute pancreatitis 33%
No IgG4 tissue staining on histology
No other organs involved
Associated IBD in 16%
Few relapses after steroid therapy
Imaging: Focal pancreatic lesions in 85%
Microscopic Features
Type 1: Dense lymphoplasmacytic infiltration of parenchyma with scattered eosinophils
Inflammatory cells aggregated around interlobular pancreatic ducts
Storiform fibrosis and obliterative phlebitis common
Pancreatic ductal architecture preserved
Prominent lymphoid follicles
Positive IgG4 staining
Type 2: Neutrophilic infiltration of parenchyma associated with characteristic granulocyte-epithelial lesions
Negative staining for IgG4
Pancreatic duct destruction
Rarely storiform fibrosis and obliterative phlebitis
Dense periductal inflammation with neutrophils
Both types 1 and 2 lack intraductal protein plugs, calcifications and pseudocysts seen with other forms of chronic pancreatitis such as alcoholic pancreatitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree