Etiology, Prevalence, and Epidemiology
Behçet disease is an uncommon systemic disorder of unknown etiology characterized by vasculitis and the triad of recurrent ulcers of the oral and genital mucosa with relapsing uveitis. Vascular complications develop in 20% to 40% of patients with Behçet disease and include subcutaneous thrombophlebitis, deep venous thrombosis, and pulmonary and systemic arterial aneurysms and occlusions. The reported frequency of pulmonary complications is highly variable, ranging from less than 1% to 18% of patients. The main pulmonary manifestations are pulmonary artery aneurysm, embolism, hemorrhage, and infarction. Although relatively infrequent, pulmonary complications are one of the most common direct causes of death in patients with Behçet disease.
Behçet disease affects men much more commonly than women (ratio of 10 : 1), and the mean age at presentation is 30 years (range, 10–59 years). Although it has a worldwide distribution, most cases cluster along the ancient Silk Road, which extends from the Middle East to East Asia. The highest prevalence rate is in Turkey (4 cases per 1000 population). The prevalence in other Asian countries ranges from 2 to 30 cases per 100,000. The prevalence in Europe and the United States is less than 1 case per 100,000 population. Of interest, there is heterogeneity in the clinical presentation of Behçet disease in nonendemic areas, suggesting that environmental factors may play a role in patient phenotype.
Clinical Presentation
The diagnosis of Behçet disease is based on the presence of recurrent oral ulcerations along with two of the following criteria: recurrent genital ulcerations; eye lesions, including uveitis and retinal vasculitis; skin lesions (folliculitis, erythema nodosum); and positive result of skin pathergy test (pustule formation 24–48 hours after skin prick). The symptoms typically wax and wane. Pulmonary manifestations may be the initial manifestation of the disease or, more commonly, develop several years after the diagnosis (mean, 5.5 years after diagnosis; range, 6 months to 26 years). Nearly all patients with pulmonary artery aneurysms have hemoptysis. Other symptoms include chest pain, dyspnea, and cough. The pulmonary symptoms may be secondary to formation of pulmonary artery aneurysms, arterial and venous thrombosis, pulmonary infarction, hemorrhage, recurrent pneumonia, or pleurisy. Hemoptysis may be massive and is a common cause of death. Behçet disease may also result in thrombosis of the superior vena cava and other mediastinal veins.
Pathophysiology
The pathogenesis of Behçet disease is unknown. The greater incidence in certain ethnic groups, the strong association with human leukocyte antigen (HLA)-B51 in many ethnic groups, the genetic association with mutations of factor V Leiden, and reports of familial clustering of disease unrelated to HLA-B51 imply that a genetic influence is important.
The histologic features of Behçet disease consist of systemic vasculitis and perivascular inflammatory infiltrates. The vasculitis can involve large, medium, and small vessels of both the arterial and venous circulation. There is a tendency to thrombus formation and for the thrombi to show evidence of inflammation. The earliest pulmonary vascular abnormalities histologically consist of transmural vascular inflammation by lymphocytes, plasma cells, and polymorphonuclear leukocytes. The inflammatory process can extend into adjacent airways and cause bronchial or pulmonary artery erosion and hemoptysis. With progression of disease, there is thinning of the muscular and elastic layers, resulting in aneurysm formation. The aneurysms are in fact pseudoaneurysms that arise as complications of vasculitis and transmural necrosis. In the majority of patients the aneurysms are multiple, bilateral, saccular, and partially or completely thrombosed; the pulmonary arteries distal to the pseudoaneurysms also are thrombosed. Other findings include organized thrombi and parenchymal infarcts, which can be related to local vasculitis and thrombosis or to thromboembolism secondary to systemic thrombophlebitis. Approximately 80% of patients with pulmonary artery aneurysms have concomitant extrapulmonary venous thrombi or thrombophlebitis.
Manifestations of the Disease
Radiography
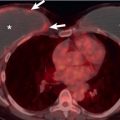
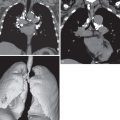
The radiologic manifestations are usually those of pulmonary artery aneurysms and thrombosis of the pulmonary arteries and systemic veins. Pulmonary artery aneurysms manifest radiographically as round perihilar opacities or as rapidly developing unilateral hilar enlargement ( Fig. 48.1 ). The aneurysms may be single or more commonly multiple and unilateral or bilateral; they usually measure 1 to 3 cm in diameter. When they are associated with an acute episode of hemoptysis, they appear poorly marginated; otherwise, they have a distinct outline. Thrombotic occlusion of the pulmonary vasculature most commonly involves the right interlobar artery and less often the lobar and segmental arteries. It may result in localized areas of consolidation resulting from infarction, areas of oligemia, and areas of atelectasis. Unilateral or bilateral pleural effusions may be seen in association with infarction. Pulmonary hemorrhage caused by vasculitis or pulmonary artery rupture occasionally results in focal, multifocal, or diffuse airspace consolidation. Thrombosis of the superior vena cava is relatively common and may be manifested on the chest radiograph as mediastinal widening resulting from associated collateral circulation and mediastinal edema ( Fig. 48.2 ). Mediastinal widening may also be due to aortic aneurysm formation.


Computed Tomography
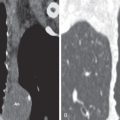
The presence, size, and location of the pulmonary aneurysms are best assessed on contrast-enhanced computed tomography (CT). Aneurysms are seen as saccular or fusiform dilatations that show homogeneous filling by contrast material simultaneously with the pulmonary artery (see Fig. 48.1 ). The aneurysms are often multiple and range from 1 to 7 cm in diameter. The wall of the involved pulmonary artery is often thickened and enhances after intravenous administration of contrast material. The aneurysms most commonly involve the right interlobar artery, followed in decreasing order by lobar and segmental arteries. Partial or complete thrombosis of the aneurysm may occur and result in localized areas of consolidation resulting from infarction, areas of decreased attenuation and vascularity, and atelectasis. Pulmonary hemorrhage from vasculitis or pulmonary artery rupture can result in focal, multifocal, or diffuse ground-glass opacities or consolidation (see Fig. 48.1 ). Other pulmonary manifestations include recurrent pneumonia and organizing pneumonia. Organizing pneumonia is a nonspecific pathologic response to lung injury characterized by organizing granulation tissue in the airspaces, alveolar ducts, and bronchioles. It is seen with increased prevalence in a variety of conditions, including collagen vascular diseases, hematologic disorders, and Behçet disease. It may occur in patients with or without evidence of pulmonary artery aneurysm or vasculitis. The CT findings typically consist of bilateral areas of consolidation involving mainly the peribronchial and peripheral lung regions.
Thrombosis of major veins, including the superior vena cava, is a common finding in patients with or without pulmonary artery aneurysms (see Fig. 48.2 ). Thrombosis of the brachiocephalic and subclavian veins may accompany superior vena caval occlusion. Thrombosis of the superior vena cava is well demonstrated on contrast-enhanced CT. It may result in partial or complete obstruction of the superior vena cava, collateral circulation, and mediastinal edema. Less common findings of Behçet disease include pseudoaneurysms of the thoracic aorta and subclavian and coronary arteries, mediastinitis (including fibrosing mediastinitis) ( Fig. 48.3 ), and pleural effusion. Unilateral or bilateral pleural effusions may result from thrombosis of the superior vena cava, pulmonary infarction, or vasculitis of the pleura.