Fig. 24.1
Cavernous hemangioma in a 69-year-old male. This lesion was found incidentally during evaluation of a gastric submucosal tumor. (a) Noncontrast transverse CT image shows a multiloculated low-attenuating lesion in the spleen. (b) On portal venous phase transverse CT image, the multiloculated cystic lesion does not show any enhancement except internal septation (arrowheads). A lobulated nodular lesion is seen abutting the stomach upper body, which was confirmed as gastrointestinal submucosal tumor (arrow). (c) Photograph of gross specimen shows a multiloculated cystic lesion which was diagnosed as cavernous hemangioma
24.11.2 Growing Hemangioma
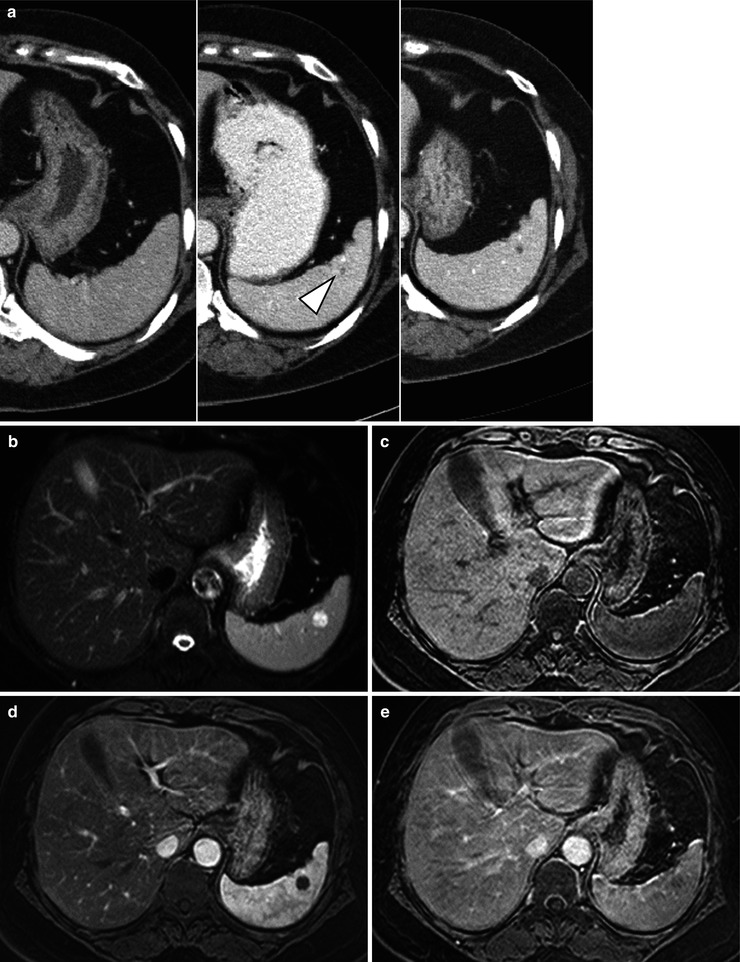
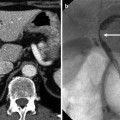
Fig. 24.2
Growing hemangioma in a 54-year-old female who underwent low anterior resection due to rectal cancer. (a) Serial follow-up of portal venous phase transverse CT images are shown. The left image was taken for preoperative evaluation of rectal cancer. There was no evidence of focal lesion in the spleen. The middle image was taken 2 years after the operation. A tiny low-attenuating lesion has newly developed in the spleen (arrowhead). The right image was taken 2.5 years after the operation. The low-attenuating lesion in the spleen has increased in size. On follow-up MR images taken 3 years after the operation, the splenic lesion shows further increase in its size. The lesion shows high signal intensity on T2-weighted image (b), low SI on T1-weighted image (c), and progressive centripetal enhancement on contrast-enhanced arterial (d) and delayed (e) phase T1-weighted images
24.11.3 Cavernous Hemangioma. Predominantly Solid
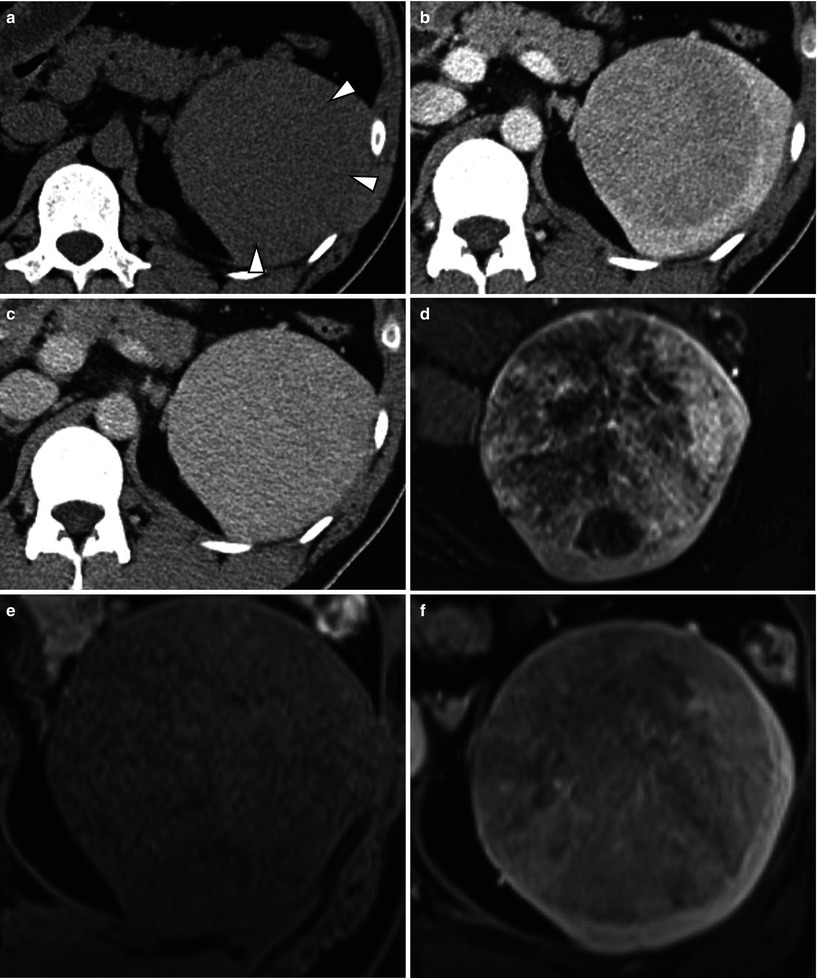
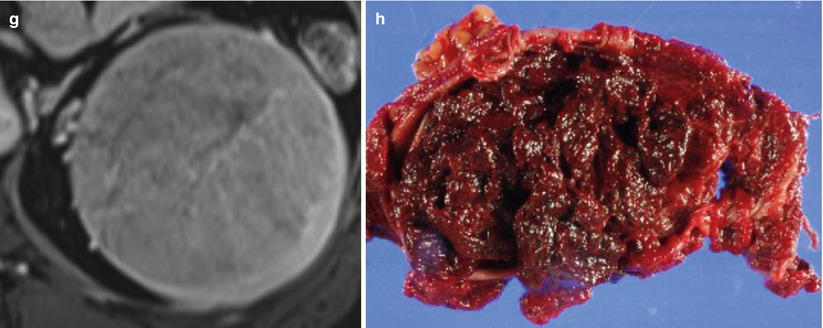
Fig. 24.3
Incidentally found splenic mass in a 39-year-old male. (a) Noncontrast transverse CT image shows an iso-attenuating focal splenic lesion compared to the adjacent spleen, resulting in difficulty of perception of the lesion (arrowheads). Portal venous (b) and delayed phase (c) transverse CT images show a well-defined mass with progressive homogeneous enhancement (d) T2-weighted transverse MR image shows a well-defined heterogeneous signal-intensity lesion in the spleen. (e) On precontrast T1-weighted transverse MR image, the lesion is seen as iso-signal intensity compared to the spleen. On dynamic contrast-enhanced portal venous (f) and equilibrium (g) phase transverse MR images, the lesion shows progressive enhancement. (h) Photograph of gross specimen shows small blood-filled spaces within the lesion which was confirmed as a cavernous hemangioma
24.11.4 Ruptured Splenic Hemangioma
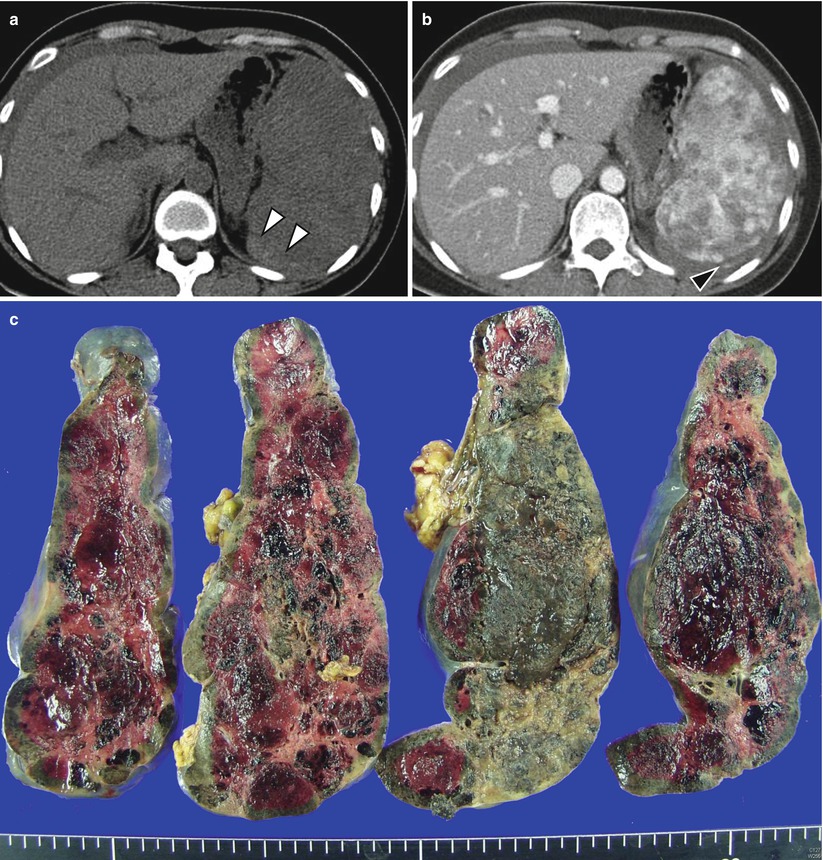
Fig. 24.4
Ruptured splenic hemangioma in a 43-year-old female. She presented with left frank pain to the emergency department. (a) Noncontrast transverse CT image demonstrates high-attenuating fluid in the perisplenic area (arrowheads). The spleen shows heterogeneous attenuation. (b) On contrast-enhanced transverse CT image, multiple low-attenuating lesions are noted in the spleen. Extravasation of contrast media is detected at the posterolateral aspect of the spleen (arrowhead), suggestive of active bleeding. (c) On photograph of a gross specimen, multiple cavernous hemangiomas were confirmed in the spleen
24.11.5 Hamartoma
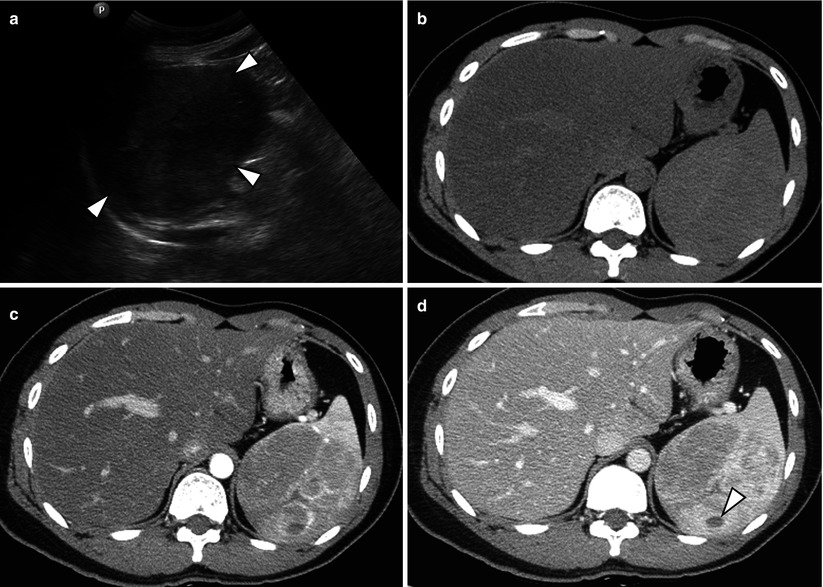
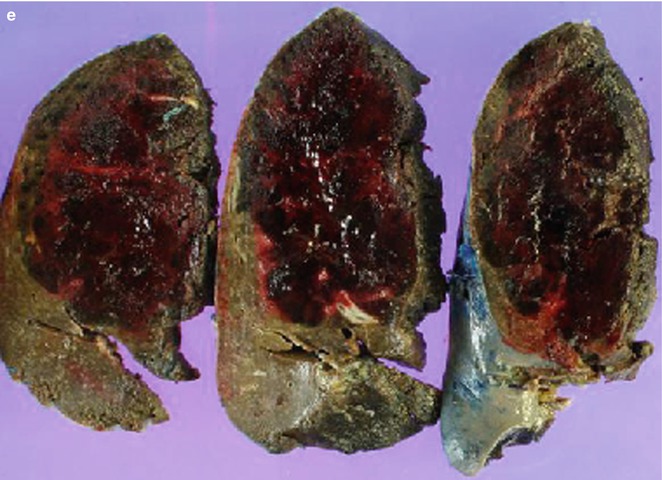
Fig. 24.5
Splenic hamartoma in a 37-year-old male. He underwent left nephrectomy due to nephroblastoma when he was 6 years old. (a) On gray-scale ultrasonography, a nodular mass with heterogeneous echogenicity is noted in the spleen (arrowheads). (b) On noncontrast CT, splenic lesion is iso- to slightly low attenuated compared to the spleen. (c, d) On arterial (c) and portal venous (d) phase transverse CT images, the lesion shows progressive heterogeneous enhancement. Focal poorly enhancing area is noted within the lesion, suggestive of cystic change (arrowhead). (e) On photography of a gross specimen, a well-defined reddish nodular lesion is noted. The final diagnosis is a splenic hamartoma
24.11.6 Lymphangioma
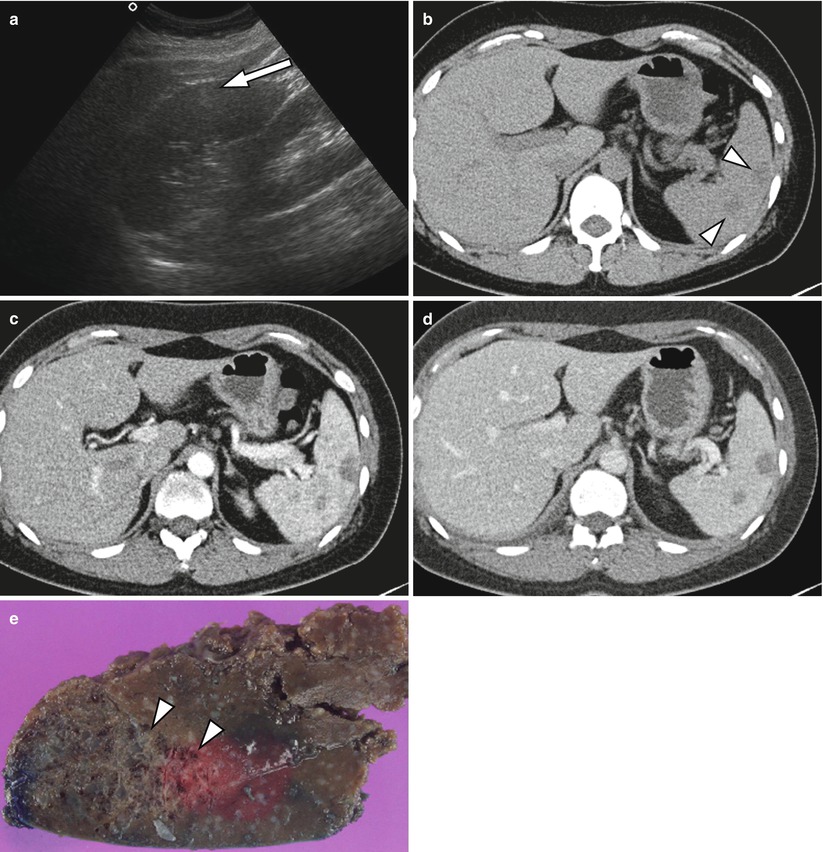
Fig. 24.6
Lymphangioma in a 61-year-old male. (a) On gray-scale ultrasonography, a heterogeneous hyper-echoic lesion is seen in the subcapsular area of the spleen (arrow).(b) Noncontrast transverse CT image shows two low-attenuating lesions in the spleen (arrowheads). (c, d) The lesions do not show any enhancement on contrast-enhanced arterial (c) and portal venous (d) phase images. (e) A gross specimen obtained after splenectomy shows a multiloculated nodular lesion composed with small dilated lymphatic spaces (arrowheads)
24.11.7 Sclerosing Angiomatoid Nodular Transformation
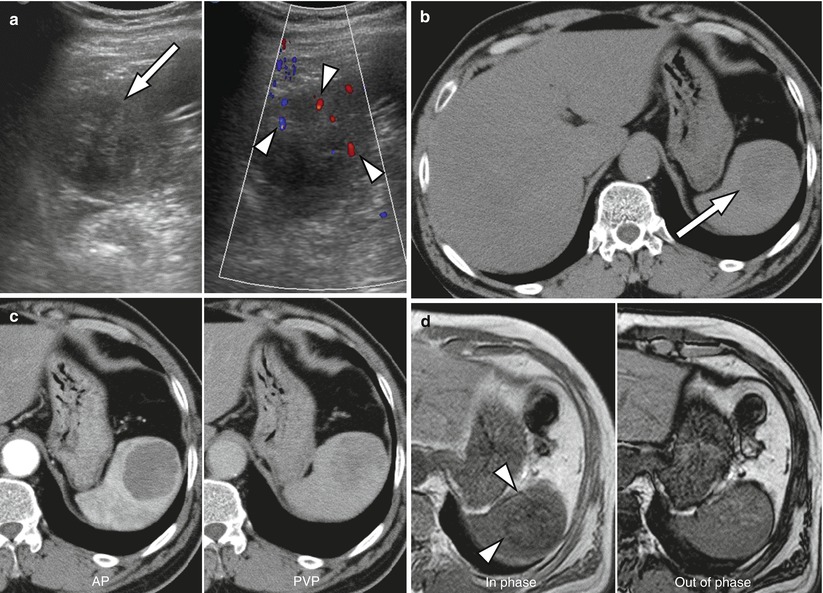
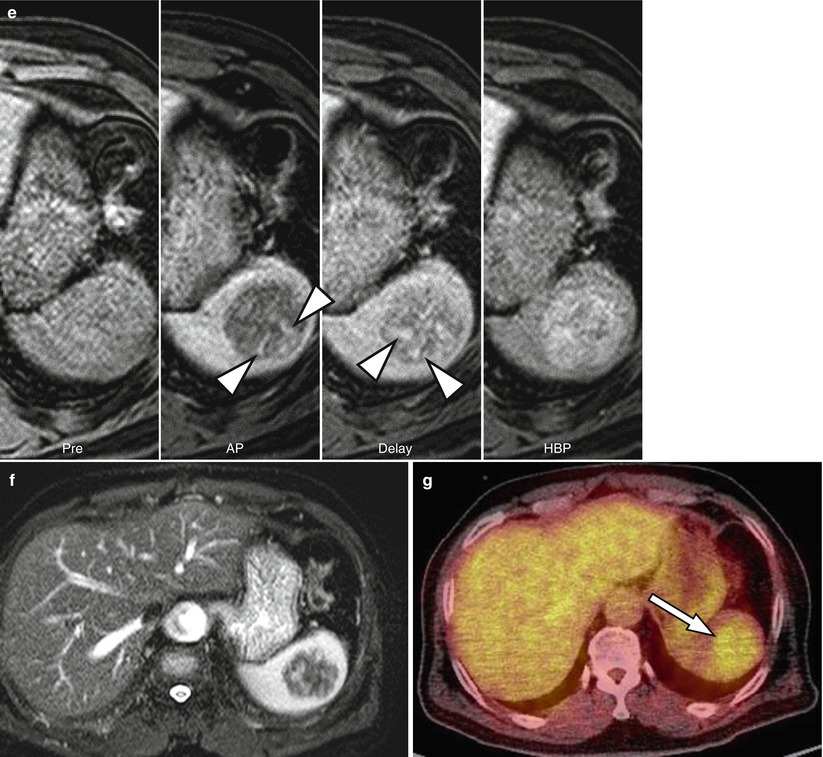
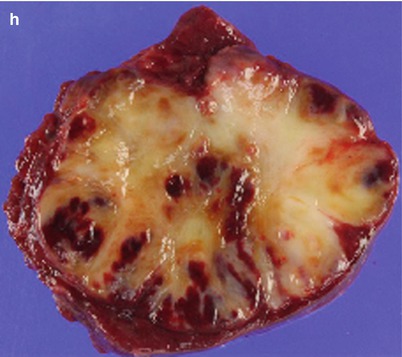
Fig. 24.7
Sclerosing angiomatoid nodular transformation (SANT) in a 74-year-old male. (a) On ultrasonography, SANT appears as a well-circumscribed heterogeneous low-echoic nodular lesion (arrow) with blood flow signals on Doppler ultrasonography (arrowheads). (b) On noncontrast transverse CT image, a well-defined nodular lesion is noted in the spleen (arrow). (c) Dynamic contrast-enhanced arterial (Left) and portal venous (Right) phase CT images show progressive-enhancing nodular lesion in the spleen. (d) On dual-echo T1-weighted MR image, SANT shows low signal intensity on in-phase image (arrowheads). (e) On dynamic contrast-enhanced MR images, SANT presents with progressive centripetal enhancement in radiating pattern (spoke-wheel appearance: arrowheads). (f) T2-weighted transverse MR image shows heterogeneous low-signal-intensity nodular lesion in the spleen. (g) On 18F-FDG PET scan, the splenic mass shows moderate increased 18F-FDG uptake (arrow). (h) On photograph of a gross specimen, the mass appears as a pale yellowish solid lesion with multifocal hemorrhage
24.11.8 Sclerosing Angiomatoid Nodular Transformation
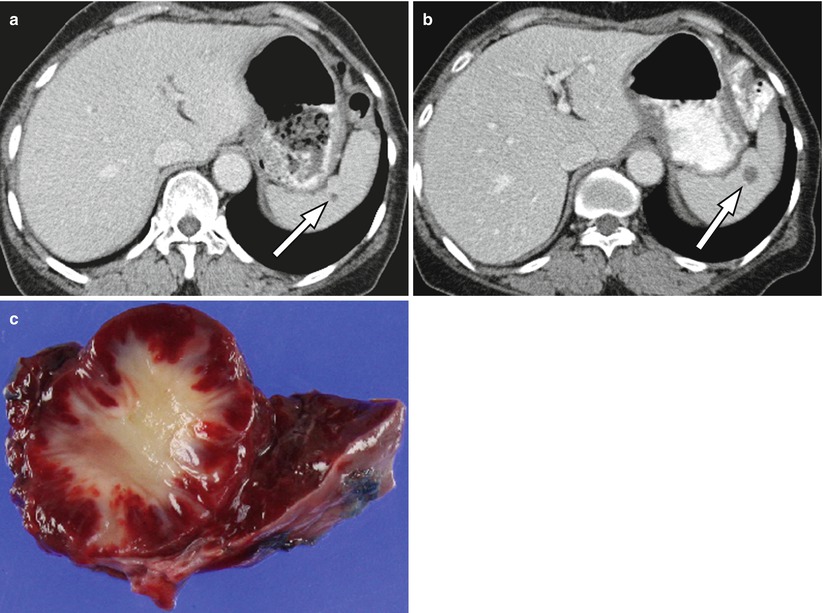
Fig. 24.8
Incidentally found sclerosing angiomatoid nodular transformation (SANT) in a 43-year-old female. (a) On contrast-enhanced transverse CT image, a small subcentimeter low-attenuating lesion is seen in the spleen (arrow). (b) Follow-up CT after 6 months, the focal splenic lesion has increased in size (arrow). Under suspicion of malignancy, laparoscopic splenectomy was performed, and the lesion turned out to be a SANT. (c) On photograph of a gross specimen, the lesion appeared as a coalescent red-brown mass with dense fibrotic stroma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree