BENIGN MASSES OF THE EXTERNAL AUDITORY CANAL, MIDDLE EAR, AND MASTOID
KEY POINTS
- A variety of diseases of the temporal bone and adjacent sites can present in the external auditory canal, middle ear, and mastoid, and imaging can focus the diagnostic process.
- Imaging is critical to treatment planning—typically, surgical removal and repair—of lesions that involve the external auditory canal, middle ear, and mastoid.
- Cancer of this region can present with the same clinical signs and symptoms as benign conditions, and imaging findings can help to anticipate a more aggressive process.
Benign lesions of the external auditory canal (EAC), middle ear, and mastoid most often have a nonspecific imaging appearance. Their anatomic location and accompanying findings will often shed the most light on the correct diagnosis (Figs. 121.1 and 121.2). Many of these benign masses/ conditions1–10 are discussed in other chapters. These include paragangliomas (Fig. 121.1 and Chapters 33 and 123), facial nerve tumors (Chapter 130), vascular malformations (Chapter 132), aberrant or variant positions of the carotid artery and jugular bulb, respectively (Chapter 108), acquired cholesteatoma (Fig. 121.3), and other chronic inflammatory middle ear and mastoid disease (Chapter 111). Malignant tumors of this region and Langerhans histiocytosis enter the differential and are discussed in Chapter 122. Fibro-osseous lesions (Fig. 121.4) are discussed in general in Chapter 40, and fibrous dysplasia more specifically as to its temporal bone manifestations is discussed in Chapter 119. Benign bone tumors and reactive changes (Fig. 121.5) are discussed in general in Chapters 38 and 14, respectively, and subsequently in this chapter.
An imaging study is usually done when an EAC lesion is covered by skin and the etiology is uncertain (Fig. 121.1). Middle ear and mastoid masses are imaged when the etiology and/or extent is unclear from the history and physical examination. Imaging allows the surgeon to understand the full extent of the disease process prior to removal, if removal is necessary (Fig. 121.6). Imaging may also provide morphologic features that suggest malignancy or a lesion that might bleed excessively if biopsied (Fig. 121.1A).
The general etiologies of a benign EAC mass will include normal anatomic variations (Fig. 104.22), developmental abnormalities (Fig. 121.7), various nonneoplastic skin diseases, reactive changes, cholesteatoma, and a wide variety of unusual to rare benign neoplasms (Fig. 121.8). Those of the middle ear and mastoid will be the same as the EAC except for the added possibility of herniation of meninges and or brain tissue or a meningioma (Fig. 121.6) and the lack of skin disorders unless they have extended to the middle ear and mastoid from the EAC.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
The complex development of the first and second branchial arches as it relates to the formation of the EAC, middle ear, and mastoid is responsible for some of the rare causes of benign masses of the external canal (Fig. 121.7). The further maturation of the EAC may also lead to EAC problems. While the inner ear and middle ear are adult size at birth, the EAC continues to develop from birth to about 9 years of age; this predisposes the EAC of children to an acquired process that might narrow the canal. Incomplete ossification in the anterior and inferior canal may result in a persistent defect known as the foramen of Huschke (Fig. 104.22); herniation of normal tissue through this developmental defect may produce a subcutaneous EAC mass.
The middle ear and mastoid are intimately associated with the brain, carotid artery and carotid canal, and jugular fossa and jugular bulb during development. This relationship can result in developmental anomalies of these structures to present as masses of the middle ear and mastoid.
Applied Anatomy
A detailed and complete knowledge of normal temporal bone anatomy and related neural and vascular structures is required for evaluation of benign masses of the EAC, middle ear, and mastoid. Computed tomography (CT) and magnetic resonance imaging (MRI) of the anatomy of the temporomandibular joint (TMJ), parotid and periparotid region, and facial nerve must also be understood when evaluating benign processes that present as a mass in this region. The main elements in this evaluation include the following:
- Soft tissues: Pinna, cartilaginous portion of the EAC, parotid gland and capsule attachments to the EAC, upper masticator space, and TMJ (Chapter 175)
- Temporal bone: EAC, middle ear, and mastoid (Chapter 104)
- Facial nerve (Chapter 104)
- Carotid artery and canal and jugular bulb and jugular fossa: Variations in their position (Chapter 104)
The pinna and cartilaginous portion of the EAC are skin covered with numerous associated hair follicles and sebaceous and ceruminous glands. In the bony EAC, the skin firmly adheres to the periosteum. The entire external ear canal is about 2 to 4 cm long, the lateral third being fibrocartilage and the remainder bone up to the bony tympanic ring where the tympanic membrane attaches and separates the EAC and middle ear (Figs. 104.20 and 104.21). Both the bony and cartilage parts of the EAC may be incomplete, with gaps that are filled with fibrous tissue; the most prominent of these is the foramen of Huschke located along the mesial anteroinferior aspect of the bony EAC (Fig. 104.22). The TMJ lies anteroinferior to the EAC. Part of the tissue of the joint capsule may herniate into the foramen of Huschke. The capsule of the parotid gland attaches to the cartilage of the EAC, providing a conduit for spread of pathology arising from either structure.
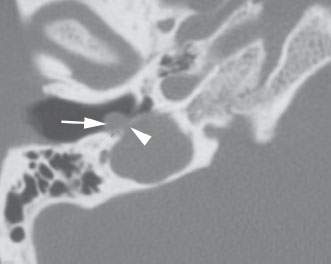
FIGURE 121.1. A patient presenting with pulse synchronous tinnitus and a mass in the external auditory canal (EAC). The mass (arrow) undermined the tympanic ring, and its relationship to the jugular bulb (arrowhead) suggested the correct diagnosis of a paraganglioma arising from the jugular bulb and projecting into the EAC.
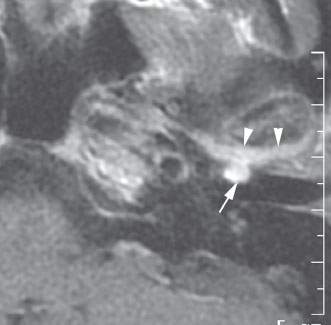
FIGURE 121.2. Contrast-enhanced T1-weighted magnetic resonance imaging of a patient with ear pain and an abnormal mass in the external auditory canal (EAC). This was found to be secondary to inflammatory arthropathy within the temporomandibular joint (arrowheads) and extending into the (EAC) (arrow).
The middle ear cavity is connected to the mastoid and eustachian tube. The tympanic cavity and mastoid antrum and air cells are lined by ciliated and nonciliated columnar epithelium. This epithelium extends into the eustachian tube to the nasopharynx.
The mastoid lies posterior to the EAC and contains the descending facial canal and its nerve as it exits the skull into the stylomastoid fat pad.
IMAGING APPROACH
Techniques and Relevant Aspects
The techniques required for the high-quality CT and MRI studies necessary in this region are presented in Appendixes A and B. In summary, CT scans must be done with a slice thickness of 0.50 to 0.75 and a combination of focused (7- to 9-cm) temporal bone field of view and wider fields of view encompassing surrounding soft tissues and the adjacent brain. These must be processed with bone and soft tissue algorithms.
Magnetic resonance (MR) studies should be focused on the precise area of interest and done with the highest possible spatial resolution. Focused studies with small volume coils produce the best results and have become more convenient to perform with the newer multiplex receiver options available. Coronal and axial MRI sections should be routinely performed, and sequences will generally include a steady state three-dimensional sequence. Intravenous contrast is used selectively.
Pros and Cons
Imaging is indispensable for the differential diagnosis and planning therapy in benign masses of the temporal bone. Both CT and MR may be necessary. CT is usually the primary study because the assessment of bony detail is often critical to diagnostic surgical decision making.
Most lesions of the EAC are epithelial in origin and often are biopsied before imaging. However, any subcutaneous or submucosal lesion should be studied with CT and supplemented by MR whenever necessary prior to biopsy (Fig. 121.1A).
Lesions that are not an obvious cholesteatoma and that present medial to the tympanic ring and tympanic membrane should always be imaged first with CT before biopsy (Fig. 121.6). Such study can help to avoid rare complications such as sampling of a paraganglioma, aberrant carotid, or encephalocele. Some might prefer MRI as the primary examination. However, MR is more typically used in selected cases to confirm meningoencephaloceles or other changes at the dura–brain interface and to aid in the differential diagnosis and perhaps to distinguish between obstructive and reactive mucosal changes in the middle ear and mastoid as opposed to those caused by the primary pathologic process of interest. In this way, imaging may obviate uniformed middle ear exploration in a considerable number of patients and entirely in some patients.
SPECIFIC DISEASE/CONDITION
Benign Masses of the External Auditory Canal
Etiology
Benign Tumors
Benign skin tumors are the most commonly encountered lesions in this group. Keratinizing stratified squamous epithelium lines the EAC, but skin adnexal structures are absent in the skin of the medial canal because the skin is adherent to the underlying periosteum of the EAC and its subcutaneous layer is absent. Benign neoplasms such as squamous cell papilloma and adenomas are uncommon in the EAC and rare in the middle ear. Ceruminous gland adenomas and other even more rare adnexal adenomas such as apocrine hidrocystoma, sebaceous adenoma, and pilomatrixoma arise from glands of the EAC.
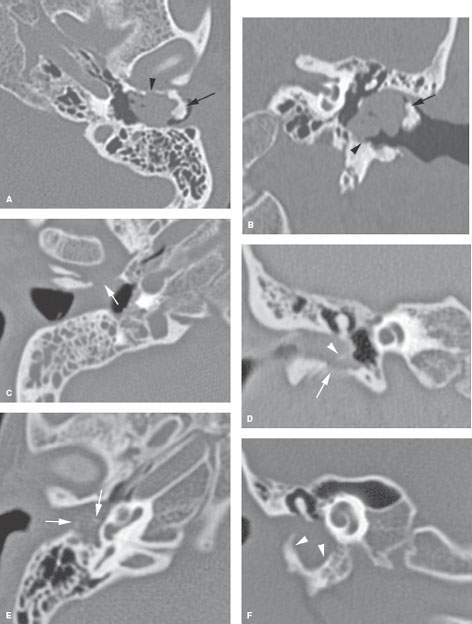
FIGURE 121.3. Three patients with manifestations of external auditory canal (EAC) cholesteatoma. A, B: Patient 1. An obstructing EAC osteoma (arrows) produced the cholesteatoma within the EAC, causing erosion of the canal walls (arrowhead). C, D: Patient 2. In (C), an axial view shows soft tissue mass in the EAC eroding the canal wall. In (D), the canal wall erosion (arrow) is again seen, and there is density related to impacted keratin debris (arrowhead). E, F: Patient 3. Cholesteatoma involving both EAC and middle ear, with origin in the EAC (arrow). There is evidence of impacted keratin debris (arrowhead in E) and extensive remodeling of the canal wall and hypotympanum (arrowheads in F).
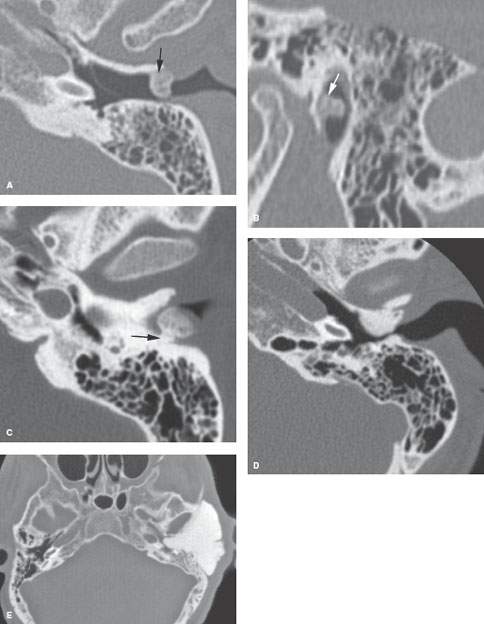
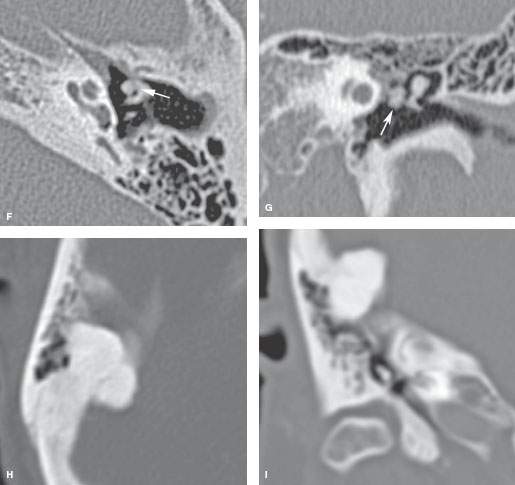
FIGURE 121.4. Several patients with osteochondral lesions of the external auditory canal (EAC). A, B: Patient 1. Osteochondroma of the EAC at the junction of the bony and cartilaginous portions (arrow). C: Patient 2. A density within the EAC showing a small pedicle (arrow) to the canal wall, identifying it as an osteochondral lesion. D: Patient 3. EAC osteoma similar to those seen in Figure 121.5, which are reactive osteomas. E: Patient 4, presenting with a large mass in the region of the temporal bone that was revealed by a computed tomography study to be a giant osteoma. F, G: Patient 5. An osteoma involving the ossicles (arrows). H, I: Patient 6. An osteoma involving a mastoid portion of the temporal bone.
Other EAC benign tumors are exceedingly rare. Leiomyoma (Chapter 35) has been reported as well as nerve sheath tumors (Chapter 29).
Benign tumors arising from the tympanic cavity, mastoid, or eustachian tube, other than a paraganglioma or facial nerve sheath tumor secondarily extending to these areas, are all exceedingly rare. The specific tumor types reported include adenoma, some of which are of minor salivary gland tumors; these tend to arise from the middle ear and the medial two thirds of the eustachian tube.
Developmental Masses
A first branchial cleft anomaly such as cyst, sinus, or fistula may protrude at the junction of the bone and cartilage portions of the EAC (Fig. 121.7). The complex branchial cleft development includes phases when mesoderm grows between the ectodermal and endodermal layers at times during development so that rests of aberrant tissue such as a salivary gland choristoma can occur.
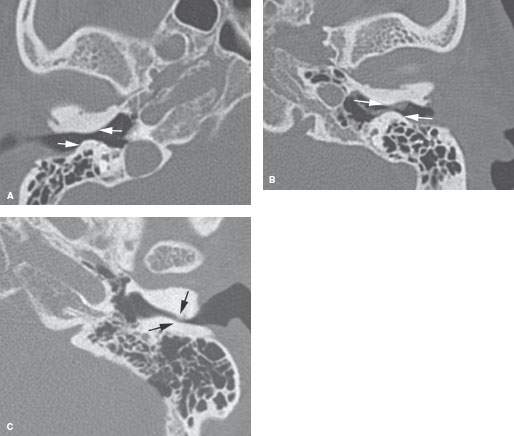
FIGURE 121.5. Two patients with reactive osteomas of the external auditory canal (EAC), or surfer’s ear. A, B: Patient 1 has moderately severe and bilateral osteomas. C: Patient 2 has an osteoma on one side and particularly severe narrowing of the EAC that produced a conductive hearing loss.
While most EAC cholesteatomas are the result of acquired disease, they may be developmental.
Incomplete ossification in the anteroinferior canal may result in a persistent defect known as the foramen of Huschke; herniation of fat, parotid tissue, and portions of the TMJ capsule (Fig. 121.2) through this developmental defect may produce a subcutaneous EAC mass.
Venolymphatic malformations (Chapter 25) may present as a mass of the EAC. These may be solely in or around the EAC or be the presenting portion of a much larger regional venolymphatic malformation that involves the temporal bone and/ or surrounding structures and spaces. A localized venolymphatic malformation in this region is most commonly called a hemangioma.
Local Trauma and Reactive and Chronic Inflammatory Changes
Damage to the canal epithelium may lead to abrasion, hematoma, or laceration. Disruption of the epithelial protective mechanisms can lead to infection or dermal inclusion cysts or keratin implantation granulomas.
A reactive exostosis will show a characteristic concentric lamellar bony organization without intervening vascular tissue in the mesial aspect of the EAC (Fig. 121.5). They are most often asymptomatic and are seen due to prolonged cold water exposure. These may obstruct the EAC and cause conductive hearing loss, infection, or otalgia.
Aural polyps result from hyperplastic inflammatory proliferation of middle ear mucosa due to chronic otitis media. They are composed of pseudostratified columnar epithelium, often with squamous metaplasia and an edematous stroma. Aural polyps extend through tympanic membrane perforations to the EAC. The polyps may completely obstruct the EAC lumen.
Foreign Bodies
Foreign bodies are a frequent problem in pediatric patients. Small objects and even insects may be found. The foreign body may be the nidus of a surrounding reactive granulomatous foreign body reaction (Fig. 121.9).
Osteoma
Osteomas (Chapter 38) are common benign neoplasms of the temporal bone.10 They are usually pedunculated lesions and arise from the anterior wall of the EAC near the bony cartilaginous junction. The bony tissue appears less organized than that seen in an exostosis due to its fibrovascular tissue content. Treatment is the same for both and consists of complete excision with preservation of as much of the normal EAC architecture as possible. These may obstruct the EAC and cause conductive hearing loss, infection, or otalgia (Fig. 121.4).
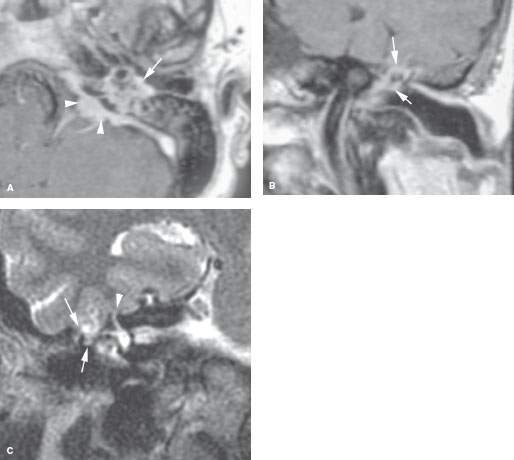
FIGURE 121.6. Three patients identifying lesions possibly with central nervous system origin that present as middle ear or external auditory canal masses. A: Contrast-enhanced T1-weighted (T1W) image of Patient 1 with conductive hearing loss and a mass in the middle ear that is visible at physical examination. The mass in the middle ear (arrow) was due to a meningioma that had its origins in the posterior fossa (arrowheads). B: Patient 2 presenting with conductive hearing loss. The T1W magnetic resonance (MR) image shows an enhancing mass in the middle ear surrounding the ossicles due to a meningioma arising within the middle ear cavity. Because the findings are confined to the middle ear, this enhancement in the middle ear is nonspecific and could just as well be due to granulation tissue. C: Patient 3 presenting with a conductive hearing loss. Computed tomography had suggested a possible encephalocele through the roof of the middle ear and mastoid. That study is not shown. The T2-weighted coronal MR image shows the encephalocele (arrows) and that the patient had an incidental superior semicircular canal dehiscence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








