Chapter Outline
Benign tumors of the esophagus constitute only about 20% of all esophageal neoplasms. Most are small lesions that cause no symptoms and are discovered fortuitously on barium studies or endoscopy. Occasionally, however, these tumors may cause dysphagia, bleeding, or other symptoms, necessitating endoscopic or surgical removal. Depending on their site of origin, benign esophageal neoplasms may be classified as mucosal or submucosal lesions, which have typical radiographic and endoscopic features.
Mucosal Lesions
Papilloma
Squamous papillomas (or simply, papillomas) are uncommon benign tumors, accounting for less than 5% of all esophageal neoplasms. The lesions consist histologically of a central fibrovascular core with multiple finger-like projections covered by hyperplastic squamous epithelium. Papillomas usually appear grossly as coral-like excrescences from the mucosa. Although the pathogenesis of these tumors is uncertain, the human papillomavirus and chronic reflux esophagitis have been implicated as causative factors.
All papillomas in the esophagus reported thus far have been benign lesions. Nevertheless, malignant degeneration has been observed in experimentally induced esophageal papillomas in rats. Malignant transformation has also been documented in papillomas arising in the oral cavity, larynx, and uterine cervix. In some cases, benign papillomas can be mistaken on histologic examination for verrucous carcinoma, an uncommon form of squamous cell carcinoma. Thus, some investigators believe that all papillomas in the esophagus should be resected because of the uncertain risk of malignant degeneration and potential confusion with verrucous carcinoma.
Papillomas in the esophagus usually occur as solitary lesions, ranging from 0.5 to 1.5 cm in size. Most patients are asymptomatic, but dysphagia is an occasional finding. Rarely, multiple papillomas may be present in the esophagus, a condition known as esophageal papillomatosis.
Radiographic Findings
Papillomas are difficult to detect on single-contrast barium studies because of the small size of the lesions. In contrast, they can be recognized on double-contrast studies as small (<1 cm), sessile polyps that have a smooth or slightly lobulated contour ( Fig. 22-1 ). Because early esophageal cancers may also appear as small polypoid lesions, endoscopy should be performed to exclude an early carcinoma. Occasionally, larger papillomas may be manifested by lobulated intraluminal masses that are indistinguishable from advanced esophageal carcinoma. Rarely, esophageal papillomas may have a bubbly appearance secondary to trapping of barium between the papillary fronds of the tumor ( Fig. 22-2 ).


Multiple papillomas may be demonstrated on esophagography in patients with esophageal papillomatosis. Despite its rarity, the diagnosis of papillomatosis should be suggested by the presence of multiple, discrete, lobulated protrusions on the mucosa ( Fig. 22-3 ). Even when multiple papillomas are present, these lesions rarely cause obstruction.

Adenoma
Adenomas account for less than 1% of all benign esophageal neoplasms. They are rarely found in the esophagus because it is lined by squamous rather than columnar epithelium. However, adenomas may develop in patients with Barrett’s esophagus (see Chapter 19 ). These adenomas are important because of the risk of malignant degeneration via an adenoma-carcinoma sequence similar to that found in the colon. Esophageal adenomas should therefore be resected endoscopically or surgically, whenever feasible.
Radiographic Findings
Esophageal adenomas may appear on barium studies as sessile or pedunculated polyps in the esophagus ( Fig. 22-4 ). Larger, more lobulated lesions have a greater likelihood of harboring adenocarcinoma. Most adenomas are located in the distal esophagus at or near the gastroesophageal junction. As a result, they can be mistaken for inflammatory esophagogastric polyps (see next section). Nodularity, lobulation, and the large size of the lesion should favor an adenoma or adenocarcinoma. When an adenoma is suspected on barium studies, endoscopy and biopsy should be performed for a definitive diagnosis.

Inflammatory Esophagogastric Polyp
Although inflammatory esophagogastric polyps are not neoplastic, they are included in this chapter because they are characterized by the presence of a polypoid protuberance in the distal esophagus abutting the gastroesophageal junction. The polyp represents the bulbous tip of a thickened gastric fold extending into the distal esophagus from the gastric fundus. The lesions are composed of inflammatory and granulation tissue and are thought to be a sequela of chronic reflux esophagitis (see Chapter 19 ). Affected individuals may therefore have clinical signs of chronic reflux disease. Because inflammatory esophagogastric polyps have no malignant potential, endoscopic resection is unwarranted.
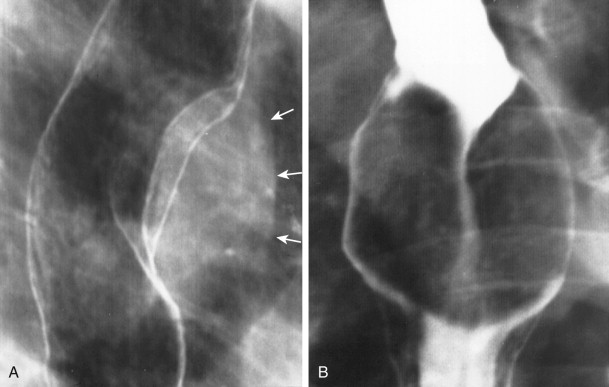
Radiographic Findings
Inflammatory esophagogastric polyps are usually manifested on barium studies by a single prominent fold that arises in the gastric fundus and extends into the distal esophagus as a smooth, ovoid, or club-shaped protuberance ( Fig. 22-5A ). The lesions frequently straddle a hiatal hernia and may be associated with other findings of reflux esophagitis. When the characteristic features of these lesions are present on barium studies, endoscopic confirmation is unnecessary. Occasionally, however, the polyps may have a more irregular, nodular, or lobulated appearance, so a malignant lesion cannot be excluded ( Fig. 22-5B ). In such cases, endoscopy and biopsy are required for a definitive diagnosis.

Glycogenic Acanthosis
Since its original description in 1970, glycogenic acanthosis has been recognized as a benign, non-neoplastic condition of unknown cause. Nevertheless, it is included in this chapter because it is manifested by mucosal nodules or plaques. Glycogenic acanthosis is characterized histologically by hyperplasia of squamous epithelial cells secondary to increased cytoplasmic glycogen. It is a common condition, with a prevalence of 3% to 15% at endoscopy. The lesions appear endoscopically as white mucosal plaques or nodules, ranging from 2 to 15 mm in size. A definitive diagnosis is made by demonstrating the characteristic glycogen-rich epithelial cells on biopsy specimens stained with periodic acid–Schiff stain.
Glycogenic acanthosis is a degenerative condition; the lesions first appear when patients are in their 40s and 50s and become larger and more numerous in patients over 60 years of age. Glycogenic acanthosis rarely causes esophageal symptoms, and it is not associated with any known risk of malignant degeneration. This condition is therefore almost always discovered as an incidental finding on radiologic or endoscopic examination.
Radiographic Findings
Although the appearance of glycogenic acanthosis was not described on barium studies until 1981, it has since been recognized as a frequent finding on double-contrast esophagography, occurring in up to 30% of patients. Glycogenic acanthosis is usually manifested on double-contrast radiographs by discrete, small, rounded nodules or plaques in the mid or distal esophagus ( Fig. 22-6 ). The lesions tend to be more obvious in the midesophagus because the distal esophagus is often obscured by pooling of barium in this region. The nodules usually range from 2 to 3 mm in size, but occasional plaques may be 1 cm or larger.

Differential Diagnosis
Although glycogenic acanthosis has little clinical significance, it should be distinguished from other causes of mucosal nodularity, such as superficial spreading carcinoma and reflux or Candida esophagitis. However, superficial spreading carcinoma is characterized by poorly defined, confluent nodules and plaques (see Chapter 23 ), and reflux esophagitis is characterized by innumerable tiny nodules in the distal esophagus, producing a granular appearance (see Chapter 19 ). In contrast, the nodules of glycogenic acanthosis are more prominent in the midesophagus and have more discrete margins with normal intervening mucosa. Although the plaques of Candida esophagitis may be indistinguishable on double-contrast studies from those in glycogenic acanthosis (see Chapter 20 ), Candida esophagitis occurs in immunocompromised patients with odynophagia or dysphagia, whereas glycogenic acanthosis occurs in older individuals who are not immunocompromised and have no esophageal symptoms. Thus, the clinical history and presentation are extremely helpful for differentiating these conditions.
Leukoplakia
Oral leukoplakia is a common condition characterized by white mucosal plaques that exhibit various combinations of hyperkeratosis, epithelial dysplasia, and frank carcinoma on histologic examination. In contrast, leukoplakia rarely involves the esophagus, and its malignant potential in this location is unknown. Endoscopy may reveal white mucosal plaques smaller than 1 cm. Rarely, the lesions may be recognized on double-contrast esophagograms as tiny nodules or plaques. However, most asymptomatic patients with a nodular mucosa probably have glycogenic acanthosis. Esophageal leukoplakia should therefore be considered a histologic rather than a radiologic diagnosis.
Acanthosis Nigricans
Acanthosis nigricans is a dermatologic disorder characterized by the triad of papillomatosis, pigmentation, and hyperkeratosis. Some patients have a malignant type of acanthosis nigricans associated with adenocarcinomas of the gastrointestinal tract, ovary, lung, or breast. Esophageal involvement has occasionally been reported in patients with the malignant form of the disease. The esophageal lesions appear on barium studies as numerous tiny nodules. Because this condition rarely involves the esophagus, the diagnosis should be suggested only in patients with known acanthosis nigricans involving the skin.
Submucosal Lesions
By definition, all submucosal lesions arising in the wall of the gastrointestinal tract are intramural. Not all intramural lesions are submucosal, however, because they can also arise from the muscularis propria or even the subserosa. Despite this distinction, the terms submucosal and intramural are used interchangeably in this text based on long-standing convention.
Leiomyoma
Leiomyomas are the most common mesenchymal tumors of the esophagus, accounting for more than 50% of all benign esophageal neoplasms. These lesions are composed of intersecting bands of smooth muscle and fibrous tissue in a well-defined capsule and consist histologically of an interlacing or palisading pattern of spindle cells with eosinophilic cytoplasm. Leiomyomas are usually smaller than 3 cm, but giant lesions as large as 20 cm have been reported. These tumors are predominantly located in the middle and lower thirds of the thoracic esophagus, because this is the portion of the esophagus lined by smooth muscle. Leiomyomas usually appear grossly as discrete submucosal masses, but some lesions have an exophytic, intraluminal, or even circumferential pattern of growth.
Most leiomyomas in the esophagus occur as solitary lesions, but multiple leiomyomas are present in 3% to 4% of patients. Rarely, these tumors may be associated with uterine or vulvar leiomyomas, apparently on a familial basis. Esophageal leiomyomas have also been documented in patients with hypertrophic osteoarthropathy, a condition characterized by clubbed fingers and toes, swollen joints, and subperiosteal new bone formation in the extremities.
Clinical Findings
Most patients with esophageal leiomyomas are asymptomatic, but lesions that encroach on the lumen may cause slowly worsening dysphagia or other symptoms such as substernal discomfort, vomiting, and weight loss. Unlike gastrointestinal stromal tumors (GISTs) in the stomach, esophageal leiomyomas rarely ulcerate, so upper gastrointestinal bleeding is extremely uncommon. Because of the slowly progressive nature of the lesions, symptoms may be present for several years before these patients seek medical attention. Rarely, affected individuals may present with signs and symptoms of acute esophageal obstruction. The treatment of choice for symptomatic patients is surgical enucleation of the tumor, but larger lesions may necessitate a more extensive esophageal resection. Leiomyomas typically do not recur after surgery.
Although leiomyomas are relatively common lesions in the esophagus, their malignant counterparts, leiomyosarcomas, are rare (see Chapter 24 ). To date, sarcomatous degeneration of an esophageal leiomyoma has not been reported. In one series, esophageal leiomyomas were followed for as long as 15 years without evidence of malignant transformation. Thus, surgical removal of small leiomyomas in asymptomatic patients is probably not warranted.
Radiographic Findings
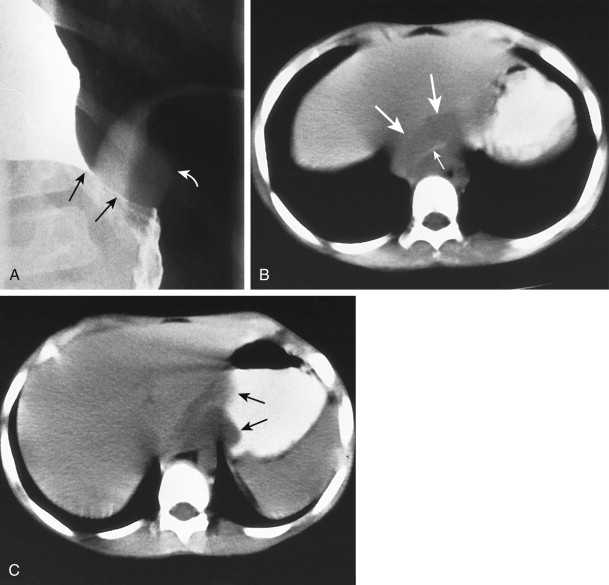
Leiomyomas that grow exophytically into the mediastinum may be recognized on chest radiographs by the presence of a mediastinal mass. Rarely, these tumors may contain amorphous or punctate calcification. Because calcification almost never occurs in other benign or malignant tumors of the esophagus, the presence of a calcified esophageal mass should suggest a leiomyoma, although one case of a densely calcified esophageal leiomyosarcoma has been reported.
On barium esophagography, leiomyomas usually appear in profile as smooth-surfaced submucosal masses (etched in white on double-contrast radiographs) that form right angles or slightly obtuse angles with the adjacent esophageal wall ( Figs. 22-7 and 22-8A ) and en face as round or ovoid filling defects with splitting of the barium column around the lesion and apparent widening of the lumen ( Fig. 22-8B ). These tumors may gradually enlarge over time, but ulceration is rare. Leiomyomas typically appear on computed tomography (CT) scans as homogeneous soft tissue masses, but differentiation from other esophageal tumors is difficult.
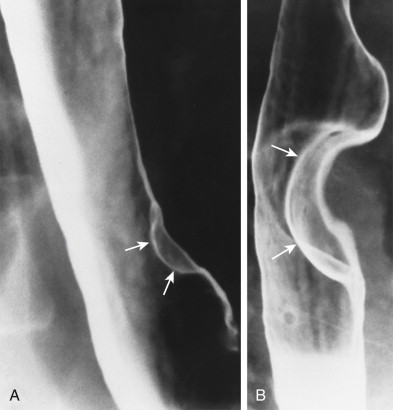
Although the vast majority of leiomyomas in the esophagus occur as solitary submucosal masses, esophagography may occasionally reveal multiple lesions or even annular lesions with varying degrees of obstruction. Rarely, leiomyomas may be giant intraluminal masses that are attached to the upper thoracic or cervical esophagus by a long pedicle. However, most pedunculated intraluminal tumors in the esophagus contain a variety of other mesenchymal elements; these tumors have therefore been classified together as fibrovascular polyps (see later, “ Fibrovascular Polyp ”). Rarely, distal esophageal leiomyomas may directly involve the gastric cardia and fundus.
Differential Diagnosis
Most submucosal masses in the esophagus are leiomyomas. However, other unusual intramural tumors such as granular cell tumors, lipomas, hemangiomas, and neurofibromas may produce identical radiographic findings (see later). Cystic lesions such as congenital duplication cysts and acquired retention cysts may also appear as submucosal masses on barium studies (see later, “ Cysts ”). Even an isolated esophageal varix may resemble a submucosal tumor, but effacement or obliteration of the lesion by esophageal distention should suggest its vascular origin (see Chapter 25 ). Because leiomyomas usually occur as solitary lesions in the esophagus, the presence of multiple submucosal masses should raise the possibility of multiple granular cell tumors or hemangiomas or malignant conditions such as lymphoma, leukemia, or Kaposi’s sarcoma involving the esophagus (see Chapter 24 ). In contrast, hematogenous metastases almost never involve the esophagus.
Leiomyomas should be distinguished from extramural lesions that are extrinsically compressing or indenting the esophagus. When viewed in profile, extrinsic lesions tend to have more obtuse, gently sloping borders than intramural lesions. Another useful criterion for differentiating these lesions is the spheroid sign, which is based on the principle that the estimated center of the mass should lie outside the projected contour of the esophagus for extramural lesions but inside the projected contour for intramural lesions. When the radiographic findings are equivocal, CT may be helpful for differentiating a submucosal tumor from a mediastinal mass compressing the esophagus.
Gastrointestinal Stromal Tumor
In the past, almost all mesenchymal neoplasms in the esophagus were thought to be benign leiomyomas, but recent studies have shown that GISTs are more common in the esophagus than previously recognized. Like leiomyomas, these tumors consist histologically of multiple spindle cells, but GISTs are characterized by their unique immunohistochemical expression of CD117, also known as C-KIT. Immunochemical testing is therefore extremely helpful for differentiating GISTs from leiomyomas because only GISTs are positive for CD117 and CD34. Patients with esophageal GISTs may be asymptomatic, or they may present with dysphagia, depending on the size of the lesion and how much it encroaches on the lumen. Unlike leiomyomas, which are always benign, however, esophageal GISTs appear to have a malignant potential similar to that of GISTs elsewhere in the gastrointestinal tract (with the development of recurrent tumor after surgical resection), so more aggressive management of these tumors may be warranted. Patients with esophageal GISTs could also benefit from adjuvant treatment with imatinib (Gleevec), a tyrosine kinase inhibitor. Thus, differentiation of leiomyomas from GISTs in the esophagus has important ramifications for patient management.
Radiographic Findings
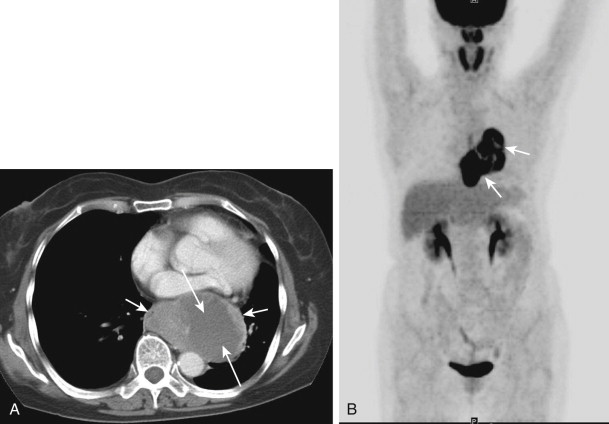
Esophageal GISTs typically appear on barium studies as discrete submucosal masses that are indistinguishable from leiomyomas or other mesenchymal tumors in the esophagus ( Fig. 22-9 ). Like GISTs elsewhere in the gastrointestinal tract, however, esophageal GISTs tend to be larger, more heterogeneous (secondary to cystic changes and necrosis), and more enhancing lesions than esophageal leiomyomas on contrast-enhanced CT ( Fig. 22-10A ). Esophageal GISTs also have uniform and marked fluorine-18-deoxyglucose (FDG) avidity on positron emission tomography (PET)/CT scans ( Fig. 22-10B ), another useful imaging feature for differentiating these tumors from leiomyomas. Radiologists should be familiar with the imaging and clinicopathologic features of esophageal GISTs and of the importance of differentiating these lesions from leiomyomas because of their apparent malignant potential.

Leiomyomatosis and Idiopathic Muscular Hypertrophy
Esophageal leiomyomatosis is a rare benign condition in which neoplastic proliferation of smooth muscle causes marked circumferential thickening of the esophageal wall, usually in the distal esophagus. This condition is found predominantly in children and young adults who present with long-standing dysphagia. Esophageal leiomyomatosis can occur sporadically or on a familial basis with autosomal dominant inheritance. In some cases, this condition is associated with widespread visceral leiomyomatosis or hereditary nephritis (Alport’s syndrome). Depending on the extent of the lesion, an esophagectomy or esophagogastrectomy is almost always curative.
Idiopathic muscular hypertrophy of the esophagus is closely related to esophageal leiomyomatosis. This condition is characterized by non-neoplastic thickening of smooth muscle in the esophageal wall, possibly as a response to severe esophageal spasm. In contrast to patients with leiomyomatosis, these individuals usually remain asymptomatic or present with dysphagia during late adulthood. Occasionally, however, patients with idiopathic muscular hypertrophy of the esophagus may have such severe dysphagia that an esophagectomy is required.
Radiographic Findings
Esophageal leiomyomatosis may be manifested on barium studies by smooth, tapered narrowing of the distal esophagus with decreased or absent esophageal peristalsis, mimicking the appearance of primary achalasia ( Fig. 22-11A ). However, the narrowed segment tends to be longer than that in achalasia, and leiomyomatosis is sometimes associated with relatively symmetric paracardiac defects in the gastric fundus because of bulging of this thickened mass of muscle into the proximal stomach (see Fig. 22-11A ). CT may reveal marked circumferential thickening of the distal esophageal wall, resembling the findings of secondary achalasia caused by metastatic tumor at the gastroesophageal junction ( Figs. 22-11B and C ). However, leiomyomatosis usually occurs in children or adolescents with long-standing dysphagia, whereas secondary achalasia occurs in older adults with recent onset of dysphagia and weight loss. Thus, despite its rarity, the diagnosis of esophageal leiomyomatosis can usually be suggested on the basis of the clinical and radiographic findings.