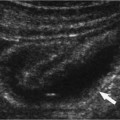
13 Biopsy, Drainage, and Percutaneous Treatment of a Mass The process to biopsy or drain a mass or to perform percutaneous treatment such as radiofrequency ablation (RFA) of a tumor begins with a consultation request. This clinical request is part of a consultation between the requesting physician and the radiologist who will perform the procedure. This consultation should include a review of the patient’s pertinent clinical history, the objectives of the requested procedure, a review of pertinent imaging studies, an assessment of whether the procedure is indicated and technically feasible, the determination of the disposition of any tissue or fluid obtained, and an assessment of the patient’s willingness and ability to tolerate the procedure. After the decision to perform the procedure has been made, the radiologist must choose a method of guidance. Three primary modalities can be used to guide percutaneous interventional procedures: fluoroscopy, computed tomography (CT), and sonography. In a few situations, the pathological condition or the patient’s anatomy may dictate a particular method of guidance. In most instances, however, sonographic guidance has proved to be quicker and easier than the other methods. In Asia and in many parts of Europe, sonography is the dominant method used to guide the performance of most nonvascular and interventional procedures. At several academic and private hospitals in the United States, sonography is used to guide 95% of all biopsies and drainages of abdominal, pelvic, pleural, and mediastinal masses. The advantages of sonography include real-time guidance, multidirectional imaging, identification and avoidance of major vessels, portability, excellent anatomical resolution, and reduced cost. The cost savings of sonography result from the lower capital expenses and operating costs of sonographic equipment and the potential use of CT scanners for diagnostic purposes, rather than for intervention. The two primary methods of performing sonographically guided intervention are the free-hand technique and the attached-guide technique. Advocates of the free-hand technique claim it allows for greater freedom in choosing needle placement and better needle visibility. Advocates of guides claim that they provide greater accuracy for deep biopsies, quicker needle localization, diminished teaching time, and improved coordination in procedures performed with nonradiologists. Because few companies manufacture needle guides for high-frequency probes, most near-field biopsies are performed with the free-hand technique. However, we believe that use of an attachable guide makes a biopsy or drainage of a mass more than 5 cm deep easier and quicker. The success of sonographic guidance depends highly on optimization of the sonographic equipment. Important parameters that should be controlled are the type of probe, the gray scale, the field of view, and the focus. All of these variables have a direct effect on the visualization of the pathological condition and the needle. For near-field biopsies, the best results are usually obtained with 7 to 10 MHz linear probes. Most abdominal biopsies are best performed with 3.5 or 2.5 MHz sector probes. The field of view should be chosen to maximize visualization of the pathological condition and the needle. As a general rule, the field of view should be adjusted so that the needle traverses at least one third of the image. Under no circumstances should a large field of view be used when performing a biopsy of a small near-field lesion. The probes should be focused at the level at which the needle is expected to enter the lesion. Visualization of the needle can be improved by needle motion (use of an in-and-out motion with approximately a 1 cm excursion) and a slight rocking motion of the probe. This rocking motion can bring a needle that has deviated slightly out of the ultrasound plane back into the field of view. With the attached-guide technique, the speed and success of the procedure can be improved by using two sets of hands: one person holds the probe and corrects it, and the second person places the needle catheter. Although the use of two people requires precise communication, it can produce less traumatic and more accurate results. In academic centers, the second person is usually a resident or fellow. In private practice, the most logical choice for the second person would be a sonographer. The most crucial task in the two-person technique is holding the probe, which is usually performed by the attending radiologist. The delivery of the anesthetic and placement of the needle are easier tasks and are usually done by the second person. Percutaneously guided intervention may seem difficult and dangerous; however, in most instances, it is relatively simple and safe. Its success requires adherence to a few basic principles: 1. Check for and correct coagulopathy in all patients with a prothrombin time greater than 15 seconds, a partial thromboplastin time greater than 45 seconds, or fewer than 50,000/mm3 platelets. 2. Defer the procedure if the patient has taken aspirin during the prior week. 3. Use abundant amounts of local anesthetic for procedures performed with needles larger than 22 gauge. 4. Do not use a local anesthetic for simple 22 gauge aspirations. 5. Confirm the location of all needle or catheter tips before obtaining a biopsy specimen or deploying drainage catheters. 6. Avoid crossing major vessels. 7. Do not aspirate potentially sterile fluid collections through the bowel. 8. Use a subcostal approach when possible. The following discussion provides examples of the standard approaches used to perform a biopsy or to drain masses. When performing percutaneous biopsies, we use only a 20 gauge end-cutting needle and an 18 gauge core biopsy gun. After the patient has been prepared for the procedure, the probe is covered with a sterile sheath, and a biopsy guide is attached. The pathological condition is located, and the path of the biopsy chosen. When possible, a subcostal approach is used to prevent the potential complications (pneumothorax, contaminated pleural space, and lacerated intercostal artery) of an intercostal approach. If the procedure is a biopsy of a liver tumor, then every attempt is made to perform the biopsy through a mantle of normal liver parenchyma. This precaution reduces the risk of bleeding because normal liver tissue is less likely to bleed than a tumor. Additionally, by choosing a biopsy path through the least vascular portion of the tumor, the risk of bleeding can be further reduced. Anesthetic is administered through the biopsy guide with a 10 cm long, 22 gauge spinal needle. Conceptually, an attempt is made to create a cylinder of anesthesia from the skin to the mass or organ from which the biopsy specimen is to be obtained. A traditional skin wheal is not raised. No skin nick is made. When the 20 gauge biopsy needle is used, the needle is placed into the lesion, and the stylet removed. The specimen is obtained by moving the needle back and forth across the lesion without aspiration. When using the 18 gauge gun, the tip of the needle is advanced to a locatio ~5 mm from the margin of the lesion and then fired across the transition zone. Care is taken to ensure that there is adequate room for needle excursion. Catheters are placed using either the trocar or Seldinger technique. With either technique, copious amounts of anesthetic are administered both through the guide and as a skin wheal. A skin nick is made and blunt dissection is performed. Because it is difficult to pass a catheter through the thoracic or abdominal fascia, adequate dissection is often the key to successful catheter placement. The trocar technique is best reserved for large “cannot-miss” fluid collections. This conviction is based on the poor sonovisibility of most catheters, which makes confirmation of location difficult, and on the marked risk associated with making multiple passes with a large-diameter trocar catheter. The Seldinger technique is used to place catheters in fluid collections that are small or hard to reach. The advantage of this technique is that it uses small-diameter, echogenic access needles. Small access needles can be placed and repositioned with a greater margin of safety than trocar drainage catheters. After satisfactory access has been obtained, a drainage catheter is exchanged over a wire. The use of locking loop catheters markedly decreases the frequency of accidental catheter removal. We do not use any of the commercially available fasteners to secure a catheter to a patient; we prefer to suture the catheter in place. Physician’s orders for the care of indwelling catheters should include an in-and-out flushing of the catheter with 10 mL of sterile saline solution every 8 hours and monitoring the input and output of the catheter. Diagnostic aspirations of localized fluid collections, pleural effusions, and ascites are performed without anesthetic. A single 22 gauge needle is placed in one pass into the fluid collection. If no fluid is obtained with this puncture, however, lidocaine is administered along the needle tract as the initial needle is withdrawn. When a 22 gauge aspiration fails (that is, when the needle is in the area of interest, but no fluid has been obtained), an 18 gauge needle is used for aspiration. If the 18 gauge needle fails to obtain fluid, the procedure may be canceled or continued with a drainage catheter.
Mode of Image Guidance for Percutaneous Treatment
Ultrasound-Guided Percutaneous Treatment
Methods
Technique
Percutaneous Biopsy
Percutaneous Catheter Drainage
Paracentesis and Thoracentesis
General Applications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree