0–9 years
10–19 years
20–29 years
30+ years
Ewing sarcoma
Osteosarcoma
Osteosarcoma
Myeloma
Osteosarcoma
Ewing sarcoma
Chondrosarcoma
Chondrosarcoma
Primary lymphoma
Primary lymphoma
Ewing sarcoma
Osteosarcoma
Primary lymphoma
Primary lymphoma
MFH/fibrosarcoma
Chordoma
MFH/fibrosarcoma
Presenting symptoms may include pain, swelling, or even pathologic fracture. Although there certainly is overlap, benign tumors tend more to be incidental findings. Some benign tumors however can mimic malignant behavior with mass affect or pathologic fracture such as a giant cell tumor. Malignant lesions tend to cause bone destruction leading to localized findings, rest or night pain, and systemic symptoms such as fevers and weight loss. Pain may occasionally be an important distinguishing feature. For example, a benign enchondroma usually does not present with pain unless fractured, whereas a similarly appearing low-grade chondrosarcoma maybe painful. Other pertinent symptoms include a history of trauma or infection. Family history may suggest a heritable condition such as multiple hereditary exostoses. Likewise, personal history of cancer such as the breast or colon may suggest possible metastases.
Physical exam includes local inspection (i.e., swelling), lymph node assessment, and systemic observation (i.e., weight loss).
Imaging
Radiographs
The radiograph is the first line of imaging for initial evaluation of a bone lesion. This imaging modality is easy to access and inexpensive and provides a wealth of information that is essential to narrowing the differential diagnosis of most primary bone tumors. The entire bone should be imaged. Often a diagnosis is made with radiographs, and if benign, no further workup may be required. Further imaging with MRI, CT, or bone scan may be required if radiographic features are nonspecific. The selection of further imaging options should be discussed with your radiologist. Occasionally, radiography can fail to show an abnormality, such as a lytic lesion, which may only become detectable when it has resulted in 30–50 % loss of mineralization. In cases where there is a high clinical suspicion of underlying pathology with normal initial imaging, further modalities should be employed.
The key to radiographic assessment of bone tumors is the concept that their appearance reflects their underlying pathology. Crucial characteristics to evaluate include lesion location, growth rate, margin, matrix, periosteal reaction, and cortical involvement (Fig. 17.1). Although there is a significant overlap, tumors have common sites of involvement, for example, primary bone lymphoma preferentially involves the femur and pelvis. Multiple lesions are suspicious for metastasis although there are benign exceptions such as multiple hereditary exostoses and hemangiomas.
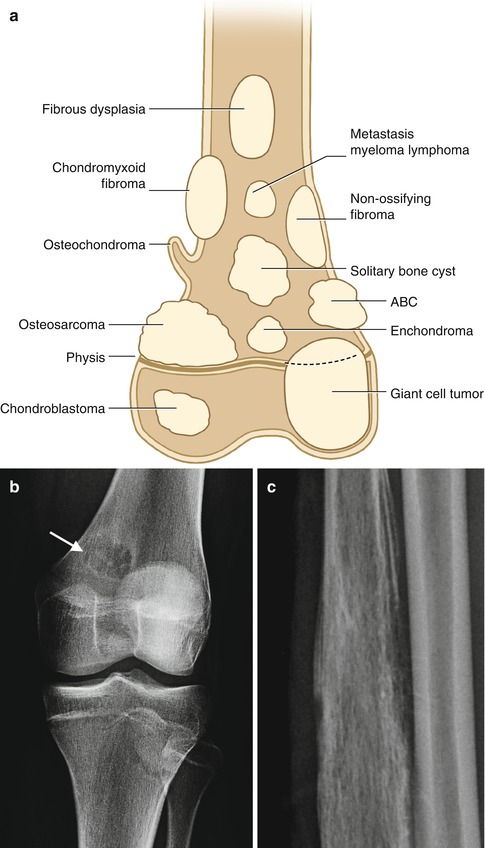
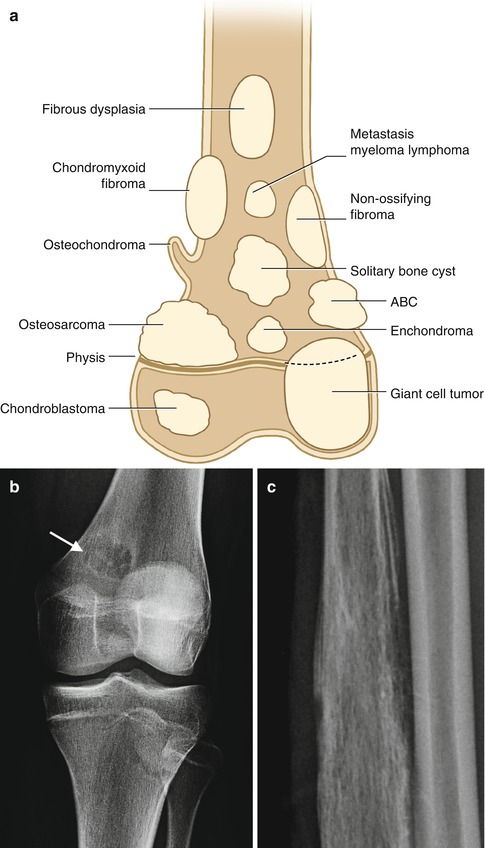
Fig. 17.1
(a) Common locations of bone tumors, (b) typical features of a benign bone lesion (arrow) with a well-defined margin, thin sclerotic rim, no cortical destruction, soft tissue mass or periosteal reaction and exhibited stability over time, lesion is typical for fibrous cortical defect when viewed in conjunction with lateral radiograph (not shown); (c) malignant lesion, Ewing sarcoma, with moth-eaten bone destruction, aggressive periosteal reaction and cortical breach
Very slow-growing or unchanged lesions over time usually suggest a benign process. The growth pattern reflects the balance between bone destruction and proliferation. A sclerotic rim indicates that the lesion’s growth rate is slow enough to allow new bone to form at the periphery. If the lesion grows too rapidly, new bone is unable to form around the lesion. An important consideration is the lesion’s impact on the structural integrity of the bone and adjacent structures. Aggressive features include periosteal reaction at the lesion’s edge indicating it has breached the cortex. An exception to this is a fracture through a benign lesion with secondary benign periosteal reaction. There are various subtypes of periosteal reaction based on appearance including laminated, hair-on-end, sunburst, or Codman triangle (Fig. 17.2). Soft tissue reactions represent tumor extension and are concerning. MRI is the most sensitive modality for assessing this although CT can be useful. Finally, many bone tumors have an internal matrix mineralization pattern that can suggest the underlying etiology. For example, chondroid matrix can appear as calcified rings and arcs. This pattern can be seen in both benign and malignant chondroid lesions and result from calcification at the periphery of multiple cartilaginous lobules (Fig. 17.3).
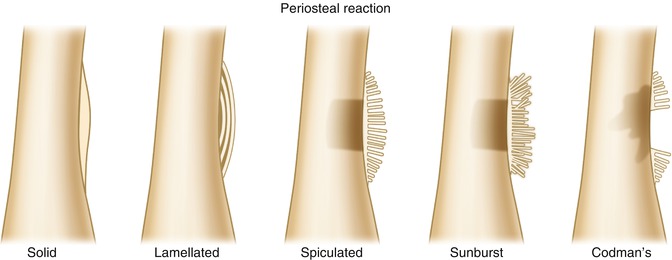
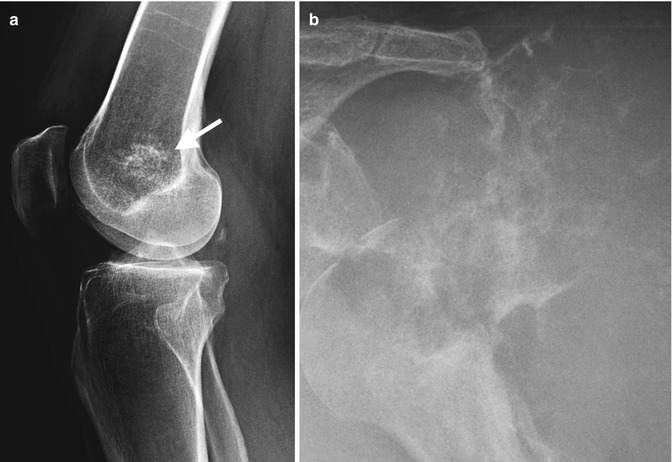
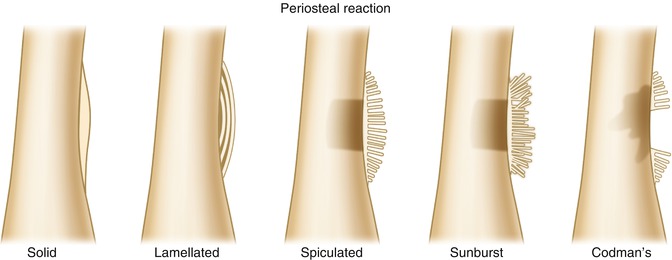
Fig. 17.2
Periosteal reaction types, benign to malignant (left to right)
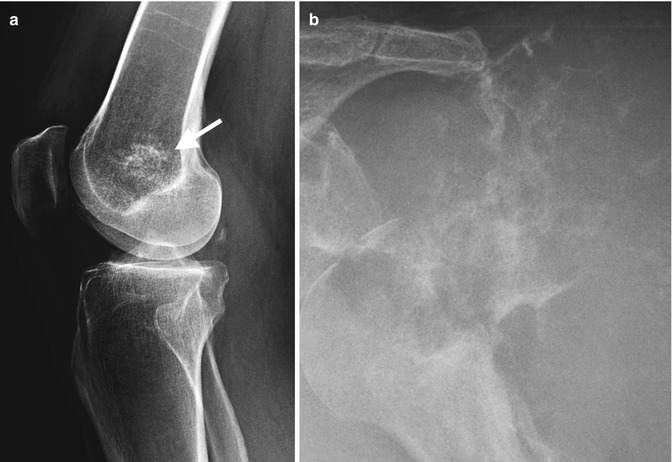
Fig. 17.3
Chondroid matrix in a benign enchondroma (arrow) (a) and a malignant chondrosarcoma (b)
Radiographic features suggesting a benign etiology include stability over time, narrow zone of transition, thin sclerotic rim, and without a cortical breach, soft tissue mass, or periosteal new bone. Conversely, cortical destruction, a wide zone of transition, and associated soft tissue mass and aggressive periosteal reaction are concerning features of malignancy.
MRI and CT
MR is excellent in evaluating the marrow signal intensity and soft tissue extension and can provide information not available with other imaging modalities. In general, the entire bone should be scanned to evaluate for skip lesions. MRI is the most sensitive technique for detecting marrow-based lesions. The MR imaging protocol for tumor evaluation depends on the location and radiographic features of the lesion. In certain cases, CT is preferable to MR imaging for tumor evaluation. CT is very useful to assess suspected intralesional mineralization, i.e., matrix. It is also excellent at demonstrating cortically based lesions, such as the central nidus of osteoid osteoma, and for evaluating subtle cortical erosion or penetration. In patients who cannot undergo MRI, CT with multiplanar capability is a reasonable substitute.
Bone scans may be helpful in assessing activity of a lesion and multiplicity, e.g., metastatic disease. In general, benign lesions demonstrate no or mild uptake and malignant lesions increased uptake on bone scans secondary to the osteoblastic response induced by the lesion. Bone scans carry a significant radiation burden, and discussion with your radiologist on the optimal imaging algorithm for your patient is advised in all cases.
The following is a brief overview of common tumors.
Benign Bone Tumors
Osteoma (Fig. 17.4)
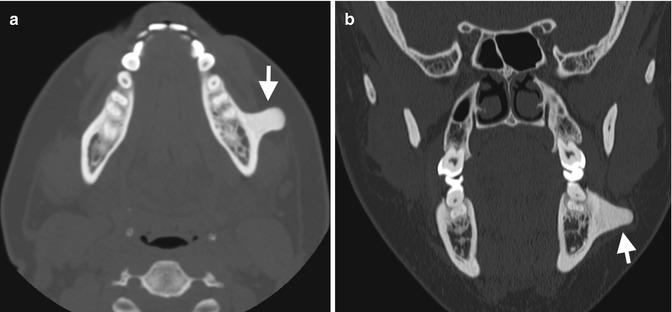
Fig. 17.4
Osteoma in an adult male patient presenting with a slow-growing mass left body mandible. (a) Axial and (b) coronal CT demonstrate a well-demarcated dense “ivory”-like bony lesion attached to an intact cortex
Osteoma is a slow-growing tumor and usually presents as an incidental finding. There is no gender or age association. This lesion is made of both woven and dense bone originating from the skull and occasionally in the long bones. All imaging modalities show a characteristic sharply defined bony surface lesion originating from the cortex.
Osteoblastoma
This is a rare osteoid-producing tumor that histologically is indistinguishable from an osteoid osteoma. A tumor size of 2 cm or larger is the main differentiating criterion. There are a variety of appearances depending on location. Spinal osteoblastomas tend to be expansile with a mineralized matrix and have a narrow zone of transition. In contrast in long bones, they may appear aggressive with prominent bone expansion, partial cortical destruction, with soft tissue infiltration.
Osteochrondroma (Fig. 17.5)

Fig. 17.5
Osteochondroma in a 15-year-old male presenting with knee discomfort postexercise. (a) Lateral and (b) AP radiographs demonstrate a well-defined lesion arising from a broad base and in continuity with the cortex of the proximal fibular diametaphysis with internal calcified matrix. (c) Axial T1 demonstrates no significant cartilage cap to lesion which extends along the posterior margin tibial neurovascular bundle and demonstrates continuity with underlying cortex (arrows)
These are cartilage-forming tumors and are relatively common. They are composed of lamellar bone covered by a cartilage cap. There is a male predominance and usually occurs in patients younger than 20 years. Imaging demonstrates cortical and medullary continuity, and it can be sessile or pedunculated in appearance. CT and MRI demonstrate a cartilage cap. After skeletal maturity, the cap should not be thicker than 2 cm. Increased thickness suggests possible transformation to chondrosarcoma.
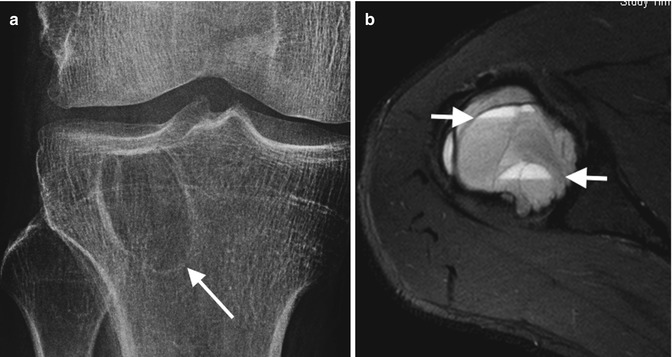
Chrondroblastoma (Fig. 17.6)
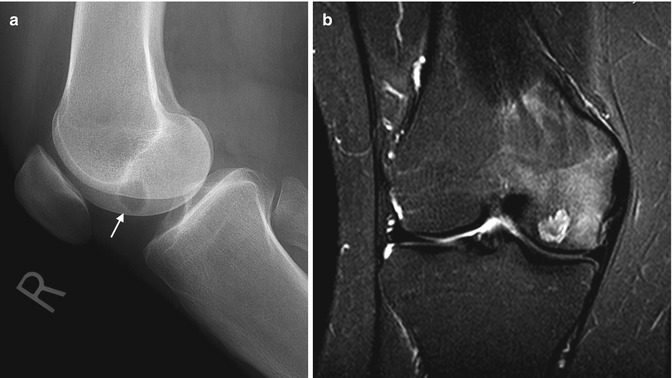
Fig. 17.6
Chondroblastoma in an 18-year-old male presenting with knee pain. (a) Lateral radiograph knee demonstrates a well-defined lytic lesion with thin sclerotic rim in the epiphysis medial femoral condyle (arrow). (b) Coronal T2FS MRI demonstrates the same lesion as well defined with internal heterogenous increased signal intensity on T2, thin low SI rim, and extensive surrounding bone marrow edema which is typical for this lesion
This is a rare lesion comprising less than 2 % of benign bone lesions. It occurs close to joints and therefore can present with some loss of joint function. It is twice as common in males as females, and most cases occur in children and young adults. Histologically, it is comprised of chondroblasts, occasional giant cells, and abundant chondroid matrix. It is most commonly seen in the proximal femur. Radiographs show a lucent lesion within the epiphysis with a thin sclerotic rim. The subtle chondroid matrix is better seen on CT, along with the adjacent periosteal reaction. The hallmark of this cartilaginous lesion is demonstrated on MR imaging and shows a typical low-to-intermediate signal of the tumor on fluid sensitive with extensive surrounding reactive marrow edema.
Giant Cell Tumor (Fig. 17.7)