Fig. 1 a, b
Osteopenia and osteomalacia. a Osteopenia is characterized by quantitative bone abnormality with decreased bone density and cortical thinning (arrows). b Osteomalacia is characterized by qualitative bone abnormality with intracortical lucencies (arrows)
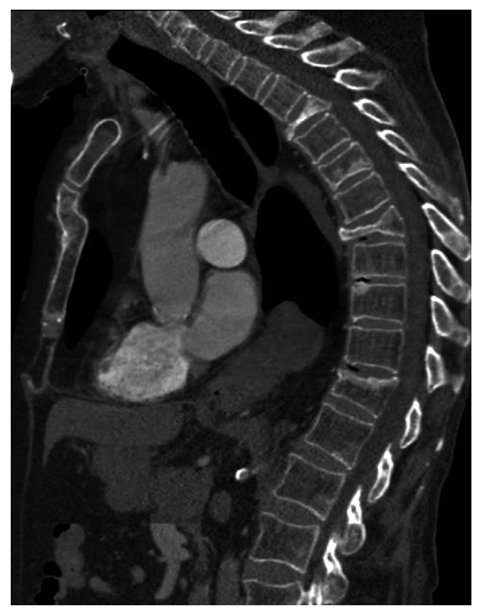
Fig. 2
Osteoporosis. Presence of multiple vertebral fractures with focal bone sclerosis superimposed on a background of hypertrophic osteoporosis. Note the sternal fracture associated with kyphosis
Prevalence of Osteoporosis
Osteoporosis is a serious public health problem for which, over the past 20 years, there have been significant advances in knowledge of its epidemiology, pathophysiology and treatment. In the western world, osteoporosis is reported to affect one in two women and one in five men over the age of 50 years [4]. The risk of fracture increases with advancing age and progressive loss of bone mass, and varies with the population being considered. The incidence of hip fracture has doubled over the past three decades and is predicted to continue to grow beyond what one would predict from increased longevity. After hip or vertebral fracture, mortality rate is about 20% greater than that expected. At 1 year after hip fracture, 40% patients are unable to walk independently, 60% have difficulty with one essential activity of life, 80% are restricted in other life activity, and 27% will have been admitted to a nursing home for the first time [4].
Clinical Presentation and Etiology
Generalized osteoporosis is a chronic disease with late clinical consequence (low-energy insufficiency fractures) (Fig. 2). Vertebral fractures are the most commonly occurring osteoporotic fracture. They occur as an acute event related to minor trauma or they occur spontaneously, and they can be accompanied by pain, which generally resolves spontaneously over 6–8 weeks. Vertebral fractures cause disability and limited spinal mobility and are associated within increased morbidity. They are powerful predictors of future fracture with a 12% increased risk of a future vertebral fracture within 12 months if a single vertebral fracture is present (22% increased risk in the presence of multiple fractures) [2]. Questionnaires are also available to evaluate fracture risk (FRAX). Consequently, the accurate identification and clear reporting of vertebral fracture by radiologists have vital roles to play in the diagnosis and appropriate management of patients with, or at risk of, osteoporosis. There is evidence that vertebral fractures are under-reported [European Society of Skeletal Radiology, Osteoporosis Group (ESSR.org); International Osteoporosis Foundation (www.osteofound.org)].
Generalized osteoporosis is the end-stage of several diseases and can be either primary or secondary (Boxes 1 and 2).
Box 1
Causes of primary osteoporosis
• | Idiopathic juvenile osteoporosis: self-limited (2- to 4-year duration) form of osteoporosis in pre-pubertal children. Acute course of the disease with growth arrest and fractures. Mild to severe forms. Differential diagnosis: osteogenesis imperfecta or other forms of juvenile osteoporosis, cortisolism and leukemia |
• | Post-menopausal (type I) osteoporosis: onset at the time of menopause but important bone loss during first 4 years after the menopause related to reduction in blood estrogen. Clinically significant in women 15–20 years after the menopause. Fractures in bones with high trabecular cortical ratio (vertebral bodies and distal forearm) |
• | Senile (type 2) osteoporosis: found in men and women 75 years or older and caused by age-related bone loss (agerelated impaired bone formation associated with secondary hyperparathyroidism as a consequence of reduced calcium absorption from the intestine secondary to decreased production of the active metabolic vitamin D in the kidney). Reduction in both cortical and trabecular bone. Fractures in vertebrae but also in bones with low trabecular cortical ratio (tibia, humerus and pelvis) |
• | Osteogenesis imperfecta: congenital disorders due to gene mutation associated with osteoporosis of variable severity. Blue sclerae and occasional dental involvement |
Box 2
Causes of secondary osteoporosis
• | Endocrine: glucocorticoid excess, estrogen/testosterone deficiency, hyperthyroidism, hyperparathyroidism |
• | Nutritional: intestinal malabsorption, chronic alcoholism, chronic liver disease, partial gastrectomy, vitamin C deficiency |
• | Hereditary: homocystinuria, Marfan syndrome, Heler-Danlos syndrome |
• | Hematologic: sickle-cell disease, thalassemia, Gaucher disease, multiple myeloma |
• | Others: rheumatoid arthritis, hemochromatosis, long-term heparin therapy |
Imaging Findings in Osteoporosis
Radiography is relatively insensitive in detecting early bone loss (less than 30–40% loss of bone tissue). In addition, radiographic bone density is affected by patient characteristics and radiographic factors used. The subjectivity of visual judgment of bone density on conventional radiographs supports the value of modern quantitative techniques such as bone densitometry.
The radiologic appearance of osteoporosis is essentially the same, irrespective of the cause (primary and secondary osteoporosis). The main radiographic features of generalized osteoporosis are decreased bone density and cortical thinning (Fig. 3). A decrease in radiographic bone density, in the absence of fractures, is termed osteopenia. It is caused by resorption and thinning of trabeculae. The process initially affects secondary (parallel to biomechanical forces) trabeculae; the primary (perpendicular to biomechanical forces) trabeculae can appear more prominent as they are affected at a later stage.
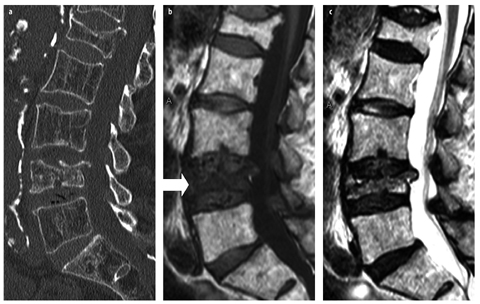
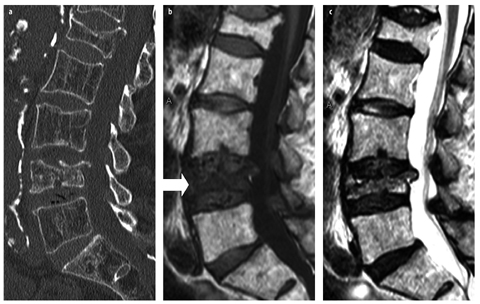
Fig. 3 a–c
Severe osteoporosis and vertebral fractures. a Sagittal computed tomography reformat of the lumbar spine shows reduced trabecular bone density and fractures. b Corresponding sagittal T1-weighted spin-echo image shows normal bone marrow except in a recent vertebral fracture (arrow). Altered trabecular bone pattern is not visible on a routine magnetic resonance image. c Corresponding sagittal SE T2-weighted spin-echo image shows intermediate to low signal intensity in recent L4 vertebral fracture
Cortical thinning occurs as a result of endosteal, periosteal or intracortical (cortical tunneling) bone resorption. Endosteal resorption is the least specific radio — graphic finding because it may be evident in metabolic disorders, including osteoporosis, and also in bone marrow disorders. Intracortical tunneling is more specific, occurring mainly in disorders with rapid bone turnover such as diffuse osteoporosis and reflex sympathetic osteodystrophy. Subperiosteal resorption is the most specific finding, and is diagnostic of hyperparathyroidism.
Osteoporosis remains occult on magnetic resonance imaging (MRI) (Fig. 3), although a relationship between trabecular bone density and marrow fat has been reported. The presence of multiple vertebral fractures with different ages (increased amount of fat in old fractures, and marrow edema or infiltration in recent fractures) suggests increased bone fragility and, hence, o steoporosis.
Measurement of Osteoporosis
Several methods have been used to standardize measurements of cortical thickness (radiogrametry), trabecular pattern (Singh index) and vertebral deformity (morphometry) from radiographs (Box 3). None of these techniques is used currently because they lack accuracy and precision. Several quantitative techniques, including dual energy X-ray absorptiometry (DXA), quantitative computed tomography (QCT) and quantitative ultrasonography (QUS), have been developed to enable accurate and precise assessment of mineral bone density [2].
Box 3
Previous quantitative methods of osteoporosis available on conventional radiographs
• | Radiogrametry involves the measurement of cortical thickness of various bones on radiographs, and the most frequently used bone is the second metacarpal bone of the nondominant hand. The metacarpal index corresponds to the ratio between the mid diaphyseal diameter of the bone (from each periosteal surface) and the medullary cavity (distance between endosteal surface) |
• | Trabecular pattern was assessed by using the Singh index, which takes into account the number, thickness and arrangement of trabeculae in the femoral neck |
• | Vertebral morphometry according to various methods has been proposed to standardize a subjective visual assessment vertebral fracture and to quantify alteration in vertebral height and shape. Vertebral fractures are defined as endplate, wedge or crush. Changes in shape of the vertebrae are generally defined by the six points method, in which the anterior, mid and posterior points of the superior and inferior endplates of the vertebral body are identified, to measure anterior, mid and posterior height. The change in shape can be graded (mild, moderate, severe) for each pattern on deformity (wedge, biconcave, crush) |
Rickets and Osteomalacia
Rickets and osteomalacia are similar metabolic bone disorders characterized by inadequate or delayed mineralization of osteoid in cortical bone and trabecular bone in children and in adults, respectively [5].
Pseudofracture or Looser’s zone is the radiological hallmark of osteomalacia, as it represents cortical fracture without a mineralized callus. Looser’s zone corresponds to a linear cortical lucency frequently perpendicular to the cortex of the bone without periosteal reaction (Fig. 4). It typically involves the ribs, the superior and inferior pubic rami, and the inner margins of the proximal femora or lateral margin of the scapula. Widened physeal growth plate and metaphyseal cupping and fraying are the radiological signs of rickets that are best seen at rapidly growing ends of bone, such as distal femur and radius or anterior ends of ribs. Additional radiological findings of rickets/osteomalacia include bone deformities, osteopenia or a coarsened pattern of the cancellous bone [5].
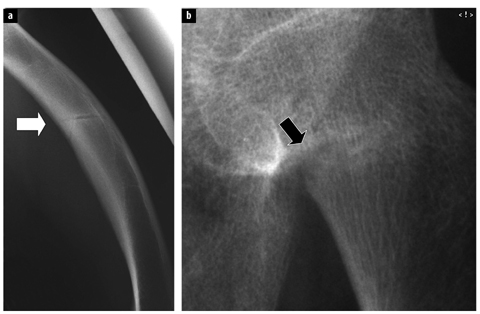
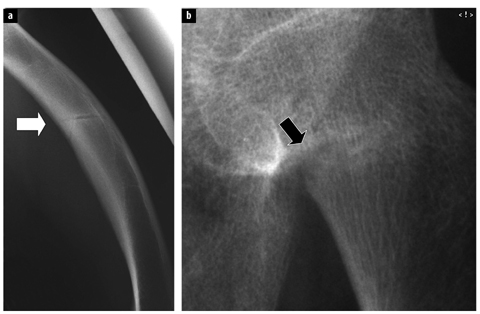
Fig. 4 a, b.
Osteomalacia. a Lateral radiograph of a femur demonstrates bone deformity with anterior bowing of the femoral shaft and cortical fracture (arrow). b Close-up radiograph of another patient with osteomalacia demonstrates pseudofracture or Looser’s zone with cortical discontinuity and bone resorption (arrow)
There is no magnetic resonance (MR) hallmark of osteomalacia, but the presence of multiple trabecular bone fractures with variable appearance at MRI (variable signal intensity on T2-weighted spin-echo images that are probably due to the various ages of the fractures) in a background of normal bone marrow should suggest the disease [6, 76] (Fig. 5). Fractures in osteomalacia can show a nonspecific bone marrow edema pattern or a more linear pattern with an occasional double line sign (probably due to the lack of adjacent edema). These fractures generally remain unchanged at short-term follow-up MRI, as osteomalacia is a disease in which the healing process is deficient. Typical cortical bone fractures or Looser’s zones are barely visible at MRI as the cortical lesion is barely visible and the adjacent marrow and soft tissue changes are discrete due to the chronicity of the lesion.
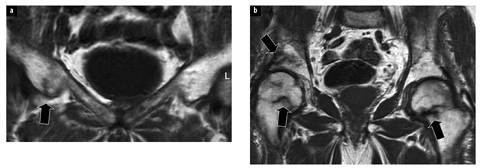
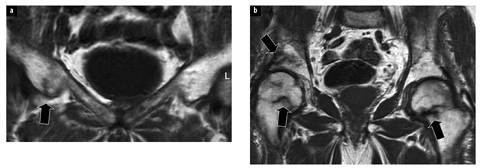
Fig. 5
Coronal T1-weighted image of the pelvis of a patient with osteomalacia demonstrates multiple trabecular bone fractures (arrows)
Renal Osteodystrophy and Hyperparathyroidism
The term renal osteodystrophy relates to all musculoskeletal manifestations of chronic renal failure [5]. Traditionally, renal osteodystrophy encompassed secondary hyperparathyroidism, osteomalacia, osteoporosis and soft tissue calcification. In fact, hyperparathyroidism and rickets or osteomalacia are the major pathologic processes of renal osteodystrophy. Primary hyperparathyroidism (generally related to the presence of a solitary adenoma in the parathyroid gland) and the classic radiographic changes of hyperparathyroidism are largely historical because diagnosis and treatment are based on serum calcium and parathyroid homone levels.
The radiographic signs of hyperparathyroidism that can appear in a patient with chronic renal failure (as in primary hyperparathyroidism) are phalangeal resorption in the hands and/or exclusive phalangeal tuft resorption (Fig. 6). The hands are the earliest and most sensitive sites for detection of hyperparathyroidism (other sites include the end of the clavicle, sacroiliac joint, and other periosteal surfaces, such as the proximal humeri or proximal femora).
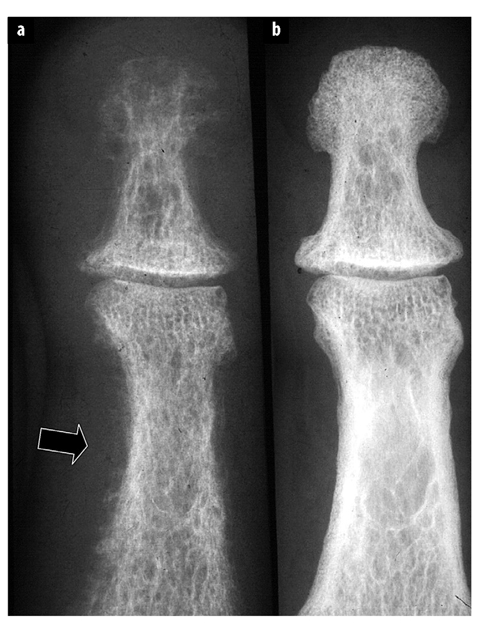
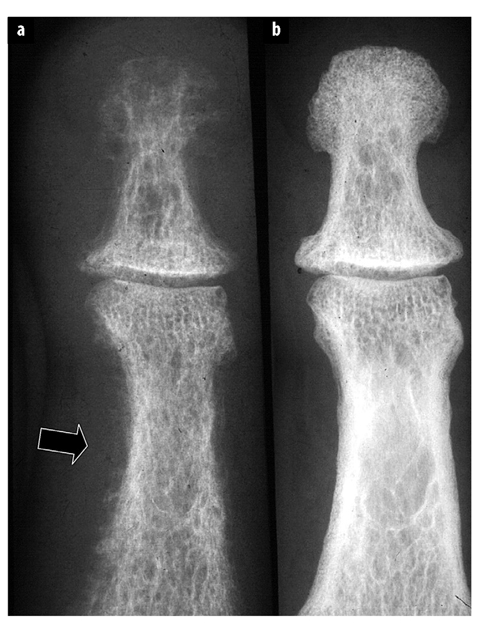
Fig. 6 a, b.




a Radiographic signs of hyperparathyroidism include sub — pe riosteal bone (arrow) and phalangeal tuft resorption. b After successful treatment, there is reappearance of woven (primary) bone
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree