Bone Metastases
 BACKGROUND
BACKGROUND
What are the top 3 sites of metastatic Dz?
Top 3 sites of metastatic Dz:
1. Lung
2. Liver
3. Bone
What is the route of spread of cancer cells to the bone?
Most bone mets arise from hematogenous spread of cancer cells.
What part of the skeleton is more commonly affected by bone mets: axial or appendicular?
Bone mets more commonly affect the axial rather than the appendicular skeleton.
What part of the spine is most commonly affected by bone mets?
The thoracic spine is the most common site of bone mets. (Bartels RH et al., CA Cancer J 2008)
What 5 tumors are known to stimulate osteoclast activity?
Tumors known to stimulate osteoclast activity:
1. Breast
2. Prostate
3. Lung
4. Renal
5. Thyroid
In decreasing order, what 5 tumors carry the highest risk of bone mets?
Top 5 tumors with regard to the risk of bone mets (in decreasing order):
1. Prostate
2. Breast
3. Kidney
4. Thyroid
5. Lung
What is the most common presenting Sx of bone mets?
Most pts with bone mets present with pain.
 WORKUP/STAGING
WORKUP/STAGING
What is the workup for bone mets?
Bone met workup: H&P, characterization of pain, assessment of fracture risk, assessment for weight-bearing bone, orthopedic consult as necessary, plain films, and bone scan
What imaging test is 1st line in evaluating bone mets?
Initial imaging of asymptomatic bone mets usually involves a bone scan (skeletal scintigraphy). If symptomatic, directed plain films and bone scan as well as subsequent clinically directed CT and/or MRI may be beneficial.
When may plain films be useful when evaluating bone mets?
In the setting of bone pain with a positive bone scan, plain films may show an impending fracture or a pathologic fracture.
What cancer is associated with mixed lytic and sclerotic lesions?
Breast cancer is associated with mixed sclerotic and lytic lesions.
What cancers are associated with primarily blastic lesions?
Tumors with predominantly blastic lesions:
1. Prostate
2. Small cell lung cancer
3. Hodgkin lymphoma
What cancers are associated with primarily lytic lesions?
Tumors with predominantly lytic lesions:
1. Renal cell
2. Melanoma
3. Multiple myeloma
4. Thyroid
5. Non–small cell lung cancer
6. Non-Hodgkin lymphoma
What imaging test can help to differentiate degenerative Dz from mets?
CT and/or MRI can help to distinguish between degenerative Dz and bone mets.
When cord compression is suspected, what imaging is indicated?
MRI of the entire spine is indicated if cord compression is suspected.
What scoring system predicts for pathologic fracture?
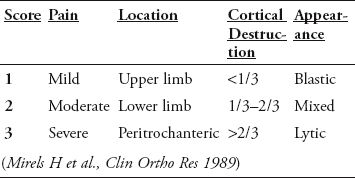
The Mirels scoring system is a weighted system based on a retrospective review that predicts the risk of pathologic fracture through metastatic lesions in long bones. Score ranges from 4–12. A score <7 can be treated with RT alone, while a score ≥8 requires internal fixation prior to RT. (Mirels H et al., Clin Ortho Res 1989)
What are the components of the Mirels scoring system?
What 2 risk factors predict for pathologic fracture of the femur?
Factors predicting for pathologic fracture of the femur:
1. Axial cortical involvement >30 mm
2. Circumferential cortical involvement >50%
(Van der Linden Y et al., J Bone Joint Surg Br 2004)
 TREATMENT/PROGNOSIS
TREATMENT/PROGNOSIS
Name 6 Tx for bone mets.
Bone met Tx:
1. Chemo
2. Radionuclides
3. Local EBRT
4. Endocrine therapy
5. NSAIDs
6. Narcotics
What supportive measures can be used for pts with painful bone mets?
Supportive care for bone mets may include orthopedic braces such as thoracolumbosacral orthosis, canes, walkers, and wheelchairs.
What interventional procedures can decrease pain from cancer-associated vertebral body collapse (i.e., compression fracture)?
Kyphoplasty and vertebroplasty are procedures performed by interventional radiologists that can address pain from vertebral body collapse. They are often performed in conjunction with EBRT.
What is the difference between kyphoplasty and vertebroplasty?
Vertebroplasty utilizes fluoroscopic guidance to inject bone cement (methyl methacrylate) into the collapsed vertebral body. In kyphoplasty, an inflatable bone tamp is inserted to restore the height of the vertebral body, creating a cavity that can be filled with bone cement.
According to the ASTRO Guidelines for Palliative RT for bone mets, what factors favor the inclusion of surgical decompression in addition to EBRT for spinal cord compression?
1. Solitary site of tumor progression
2. Absence of visceral or brain mets
3. Spinal instability
4. Age <65 yrs
5. Karnofsky performance score (KPS) ≥70
6. Projected survival >3 mos
7. Slow progression of neurologic symptoms
8. Maintained ambulation
9. Nonambulatory for <48 hrs
10. Relatively radioresistant tumor (i.e., melanoma)
11. Site of origin suggesting relatively indolent course (i.e., prostate, breast, kidney)
12. Previous EBRT failed
(Lutz S et al., IJROBP 2011)
In what cancers may chemo eradicate bone mets?
Chemo can cure bone mets from lymphomas and germ cell tumors.
What is the chief action of bisphosphonates? Name 2.
Bisphosphonates inhibit osteoclast activity. Pamidronate and zoledronic acid are 2 common bisphosphonates.
What is denosumab (XGEVA)?
Denosumab is a fully human monoclonal antibody that targets receptor activator of nuclear factor-kappa beta ligand (RANKL), thereby inhibiting maturation of osteoclasts.
What are the American Society for Clinical Oncology (ASCO) 2011 guidelines for bone-modifying agents (BMAs) in the Tx of bone mets from breast cancer?
ASCO 2011 guidelines state that either bisphosphonates (pamidronate or zoledronic acid) should be administered q3–4wks or denosumab should be administered q4wks to breast cancer pts with evidence of bone metastases. BMAs are adjunctive therapy, not recommended for 1st-line therapy and should be used concurrently for pain relief with analgesics, chemo, RT, and/or hormonal therapy. (Van Poznack C et al., JCO 2011)
Name 4 radionuclides used to treat bone mets.
Radionuclides available in the U.S. for Tx of bone mets:
1. Strontium-89
2. Samarium-153
3. Phosphorus-32
4. Radium-223 (currently for prostate cancer only)
For each of these radionuclides, name the method of decay, half-life, average particle energy per decay, and particle range.
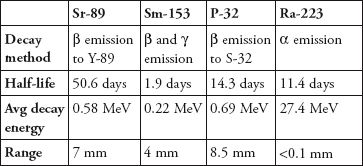
Describe the clinical implications of the differences in physical properties between strontium-89, samarium-153, phosphorus-32, and radium-223.
1. Both strontium-89 and phosphorus-32 emit β particles with higher energy than those of samarium-153, causing deeper tissue penetration. Though these higher-energy β particles may have a therapeutic benefit, they can also cause greater marrow toxicity.
2. The half-life of samarium-153 is much shorter than that of strontium-89. Thus, the planned RT dose from samarium-153 is delivered more quickly, leading to faster time to pain relief in many published trials.
3. Radium-223 emits high-energy α particles, which have high linear energy transfer inducing double-stranded DNA breaks, but a short range resulting in very limited toxic effects on adjacent healthy tissues.
Why is phosphorus-32 seldom used for bone mets?
Phosphorus-32 was the 1st radionuclide to be used for bone mets, but it has greater hematologic toxicity compared with the other radionuclides available in the U.S.
When should radionuclides be considered?
Radionuclides should be considered in pts with adequate blood counts and multifocal painful bone mets imaged on bone scan.
What are some contraindications to radionuclides for bone pain?
Contraindications for using radionuclides for bone pain:
1. Myelosuppression
2. Impaired renal function
3. Pregnancy
4. Cord compression
5. Nerve root compression
6. Impending pathologic fracture
7. Extensive soft tissue component
What randomized data support the use of samarium-153?
A double-blind placebo controlled study of samarium-153 supports its use. 118 pts with symptomatic bone mets were randomized to low-dose samarium-153 (0.5 mCi/kg), high-dose samarium-153 (1 mCi/kg), or placebo. Pts receiving high-dose samarium-153 had significant improvement in pain during the 1st 4 wks per pt and medical evaluation. Relief persisted until at least wk 16 in 43% of pts. There was a significant reduction in the pain score and analgesic use only in pts receiving the high dose. (Serafini A et al., JCO 1998)
What randomized data supports the use of radium-223?
ALSYMPCA is a multi-institution double-blind placebo controlled study of radium-223 that showed an overall survival benefit for pts with castrate-resistant metastatic prostate cancer (14.9 mos vs. 11.3 mos, p <0.001). Pts were randomized 2:1 to 6 IV injections of radium-223 (dose 50 kBq per kg) q4 weeks vs. placebo injections on the same schedule. The trial was stopped early due to OS benefit on planned interim analysis. (Parker C et al., NEJM 2013)
What RTOG study originally reported no difference in bone pain relief between different fractionation schemes?
RTOG 7402 randomized 759 pts. Those with solitary bone mets were randomized to 40.5 Gy (2.7 Gy × 15) vs. 20 Gy (4 Gy × 5). Pts with multiple mets were randomized to 30 Gy (3 Gy × 10), 15 Gy (3 Gy × 5), 20 Gy (4 Gy × 5), or 25 Gy (5 Gy × 5). The initial report revealed that 90% of pts had some pain relief, and 54% had eventual CR of pain. There was no difference between regimens. (Tong D et al., Cancer 1982) Reanalysis showed that a higher # of fx correlated with CR of pain, suggesting that a more protracted course was more effective. The analysis was based only on physician assessment of pain. (Blitzer P et al., Cancer 1985)
Which pts are generally excluded from RCTs of different fractionations for bone-met RT?
RCTs assessing different fractionation schemes for the Tx of bone mets have generally excluded pts with cord compression and pathologic fracture.
Did the study by the Bone Pain Trial Working Party support single- or multi-fx Tx of bone mets?
The Bone Pain Trial Working Party supported single-fx Tx. The study (UK/NZ) randomized 765 pts with painful bone mets to 8 Gy × 1 vs. a protracted regimen (2 Gy × 5 or 3 Gy × 10). Pain relief was evaluated for up to 1 yr post-Tx by the use of a validated pt questionnaire. There was no difference in pain control between the arms. Re-Tx was twice as common with single-fx Tx (23% vs. 10%), though this may have been due to a greater willingness to re-treat pts who rcvd only 8 Gy × 1. (No author, Radiother Oncol 1999)
Did the Dutch Bone Metastasis Study support single- or multi-fx Tx of bone mets?
The Dutch Bone Metastasis Study supported single-fx Tx. 1,171 pts were randomized to 8 Gy × 1 fx vs. 4 Gy × 6 fx. Pain relief was evaluated for up to 2 yrs post-Tx by the use of a validated pt questionnaire. No difference was seen with respect to pain relief. However, re-Tx was more common in the single-fx arm (25% vs. 7%). (Steenland E et al., Radiother Oncol 1999) Reanalysis suggested that the higher rate of re-Tx in the single-fx arm may be related to a greater willingness to re-Tx pts who rcvd only 8 Gy × 1 fx. (Van der Linden YM et al., IJROBP 2004)
Did RTOG 9714 support single- or multi-fx Tx of bone mets?
RTOG 9714 supported single-fx Tx. The study randomized 898 pts with breast or prostate cancer to 8 Gy × 1 fx vs. 3 Gy × 10 fx. There was no difference in complete pain relief (15% vs. 18%) or partial pain relief (50% vs. 48%), but there was increased acute toxicity in the 3 Gy × 10 arm (10% vs. 17%). The re-Tx rate was significantly greater in the 8 Gy × 1 arm. (Hartsell W et al., JNCI 2005)
What were the results of the Chow et al. meta-analysis of trials comparing single- vs. multi-fx Tx of bone mets?
In this meta-analysis of trials comparing single- vs. multi-fx Tx of bone mets, no significant differences between fractionation schemes with respect to pain control were shown. However, re-Tx was more common with single-fx Tx. (Chow et al., JCO 2007)
What study supported use of hemibody irradiation (HBI) after focal RT for bone mets?
RTOG 8206 randomized pts treated with focal RT to HBI (8 Gy) vs. no further Tx. HBI increased the time to progression as well as the time to re-Tx. (Poulter C et al., IJROBP 1992)
What are the published response rates of RT for palliation of symptomatic bone mets irrespective of the fractionation scheme?
The published response rates of RT for palliation of symptomatic bone mets are 60%–80%.
What is the benefit of PORT after orthopedic stabilization?
PORT following orthopedic stabilization of impending or pathologic fracture decreases the need for 2nd surgery (2% vs. 15%) and increases the rate of regaining normal function (53% vs. 11.5%) as compared with surgery alone. (Townsend P et al., JCO 1994)
What data support the use of SRS for spinal mets?
Prospective nonrandomized data from the University of Pittsburgh support the use of SRS for spinal mets. 500 cases were treated with CyberKnife to a median dose of 20 Gy. SRS improved pain in 86% of cases (defined as a 3-point improvement on a 10-point pain scale). The majority of pts had prior Tx; however, in the 65 cases treated with SRS as the primary modality, the LC was 90%. (Gerstzen P et al., Spine 2007)
What is the MS of pts with metastatic cancer who present for palliative RT?
Risk factors: (1) nonbreast primary, (2) sites of mets other than bone, (3) KPS ≤60.
| # of risk factors | MS |
| 0–1 | ~60 wks |
| 2 | ~25 wks |
| 3 | ~10 wks |
(Chow E et al., JCO 2008)
 TOXICITY
TOXICITY
What are the expected acute and late RT toxicities associated with Tx of bone mets?
Potential toxicities from focal RT for bone mets:
Acute: skin irritation
Late: fibrosis, nerve damage, fracture, lymphedema
What is the main toxicity of radionuclide Tx?
Radionuclide Tx can cause significant myelosuppression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


